A multiparous 41 y.o. female with history of an episode Atrial Fibrillation with Rapid Ventricular Response (AF RVR) in the setting of pregnancy 15 years prior and recent stillbirth presented with recurrent AF RVR in the setting of a 34 week gestation based on bedside US.
The patient began feeling SOB with fast heart rate and dizziness the previous evening (approximately 12 hours prior). Since it continued, she presented to a smaller hospital, where her EKG showed possible AF RVR with rates as high as 180 bpm, then down to 140s after metoprolol.
Her d-dimer was also elevated at nearly 2000, so she was transferred to a tertiary center for management of AF RVR in the setting of high risk pregnancy.
On arrival, she reported no new complaints, and stated that she can still feel the baby moving, that she has not felt contractions, and she has not had any leakage of fluid. She had not sought prenatal care due to anxiety surrounding previous pregnancy ending in stillbirth.
BP 135/107 | Pulse (!) 181 | Resp (!) 29 | SpO2 (!) 92%
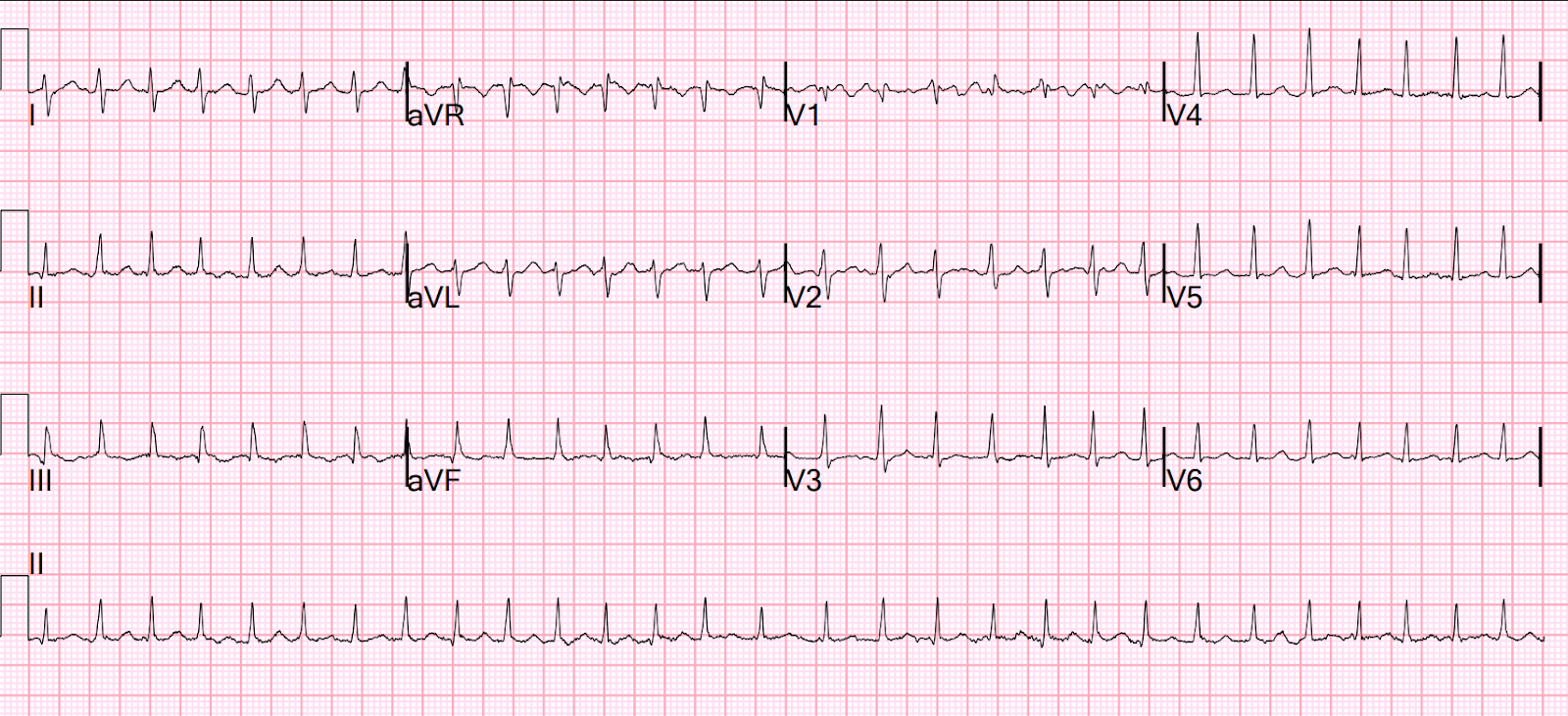
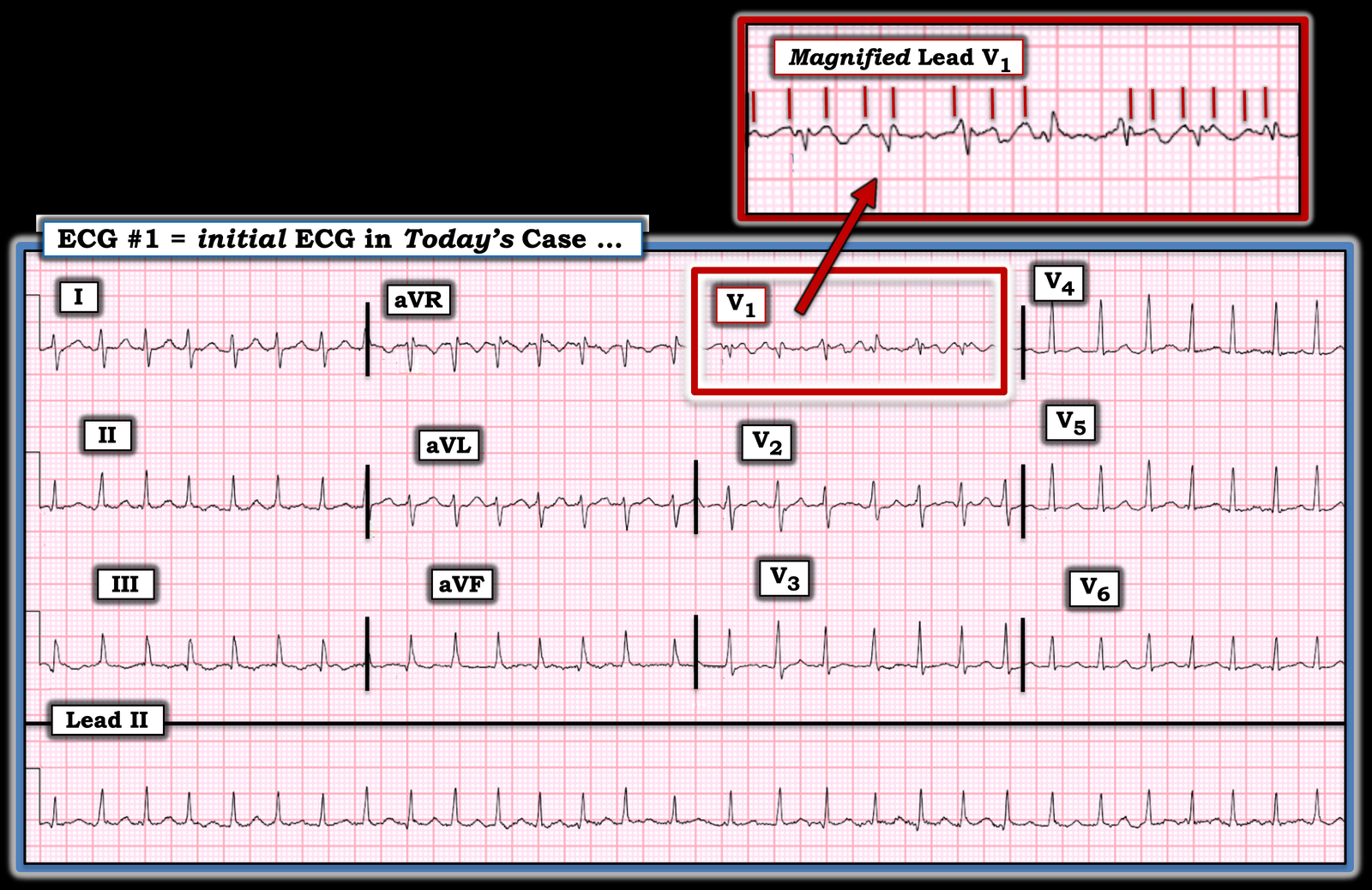
Here is her ED ECG:
Electrical cardioversion
Emergent or elective electrical cardioversion can be performed at all stages of pregnancy [13,50,76], and should be used for any sustained arrhythmia with hemodynamic compromise and can be considered for drug-refractory arrhythmias. In the third trimester, some physicians prefer to perform electrical cardioversion under general anesthesia and intubation, considering the more difficult airway and increased risk of gastric aspiration during pregnancy. Electrical cardioversion does not result in compromise of blood flow to the fetus [76]. While there is a theoretical risk of inducing an arrhythmia in the fetus, this risk is very small due to the high fibrillation threshold and small amount of energy reaching the fetus. Nonetheless, postprocedure continuous electronic fetal heart rate monitoring is recommended because of reported cases of emergency cesarean delivery due to fetal arrhythmias [77].
In one multicenter study, 27 pregnant females had 29 electrical cardioversions for supraventricular arrythmias (atrial fibrillation [44 percent], atrial flutter [30 percent], SVT [19 percent], atrial tachycardia [7 percent]) [78]. There were no maternal or fetal deaths. Median gestation at cardioversion was 28 weeks, and median gestation at delivery was 35 weeks. Postprocedure fetal monitoring was undertaken following cardioversion in nearly half the patients and in 7 percent, urgent delivery was required postcardioversion due to fetal bradycardia.
= = =
======================================
MY Comment, by KEN GRAUER, MD (10/9/2025):
Two aspects of today’s case merit special attention: i) The rhythm diagnosis; and, ii) Treatment considerations of the rhythm diagnosis, given the pregnant state of this patient.
= = =
The Rhythm Diagnosis:
For clarity in Figure-1 — I’ve reproduced the patient’s initial ECG. There was uncertainty about the rhythm when the patient was first seen.
- That the rhythm was supraventricular and tachycardic was obvious from the narrow QRS in all 12 leads — and the rapid rate.
- KEY Point: Although at first glance, the rhythm in Figure-1 may look regular — it is not regular. That the rhythm is actually irregularly irregular (with slight-but-real variation in the R-R interval throughout the entire long lead II rhythm strip) — can be verified within seconds by use of calipers (To Emphasize — With practice, the irregular irregularity of this rhythm can be immediately recognized without calipers, as I was able to do).
- There are no P waves in any of the 12 leads.
- Therefore: The finding of an irregularly irregular rhythm with narrow QRS and no P waves — defines this rhythm as AFib (Atrial Fibrillation), here with a rapid ventricular response.
- NOTE #1: It is common for AFib with a rapid ventricular response to “look” regular — which may lead to misdiagnosis of a reentry SVT rhythm (such as AVNRT or orthodromic AVRT). While most patients tolerate IV Adenosine — this medication is not without potential for side effects. Given that Adenosine is not effective for AFib — recognizing today’s rhythm could have avoided the trial of Adenosine.
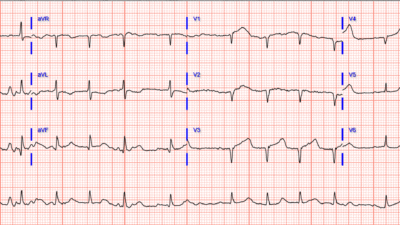
- NOTE #2: Review of the magnified insert of lead V1 (in the upper right corner of Figure-1) — suggests that there is atrial activity in this lead. But the vertical RED lines that I have highlighted are not flutter waves. It is common for there to be transient “organization” of AFib wavelets — and when this happens, you may see atrial deflections that almost look regular in lead V1 (which is the closest lead for recording atrial activity). But AFlutter (Atrial Flutter) is characterized by regular atrial activity, that in a patient not on antiarrhythmic medication — typically manifests an atrial rate range between ~250-350/minute.Therefore — the irregularity of the atrial activity in Figure-1, which at times far exceeds 300/minute rules out AFlutter as the rhythm diagnosis.
= = =
Figure-1: I’ve labeled the initial ECG in today’s case.
= = =
Treatment Considerations of AFib in a Pregnant Patient:
My review of AFib Treatment during Pregnancy encompassed the following publications: Tamirisa et al (J Am Coll Cardiol EP 1:120-135, 2022) — Cacciotti and Passaseo ( J Atr Fib 3(3):295, 2010) — and — Youssef ( Eur Soc Card 15(17), 2019):
- Overall — AFib is not a common complication of normal pregnancy. That said, I found it difficult to estimate the prevalence of this arrhythmia — as frequency estimates will depend on multiple factors including age and health status of the patient, and presence of precipitating factors.
- There are additional complicating factors in today’s case. These include the patient’s age (41 years old) and multiparous status (G8P6) — with lack of prenatal care (because of patient anxiety resulting from the previous pregnancy ending in stillbirth). Estimated gestation of this current pregnancy = 34 weeks. Of note — this patient had a previous episode of AFib in 2009 during one of her earlier pregnancies!
= = =
Regarding Treatment:
- First priority (as for any patient with new, rapid AFib) — is to ensure hemodynamic stability. If/as needed — electrical cardioversion appears to be safe at all stages of pregnancy. (During and after electrical cardioversion — fetal monitoring is advised, given the risk of fetal arrhythmias).
- Look for Potential Precipitating Factors — which is critical, since if an underlying cause of AFib is present — this will greatly affect treatment decisions (Rule out hyperthyroidism, alcohol use, cocaine or other illicit drug use, sympathomimetic or other stimulant medication, electrolyte disturbance — adult congenital heart disease — rheumatic heart disease — peripartum cardiomyopathy — or other form of underlying heart disease) ==> An Echo, TSH, CBC, electrolytes, etc. — all part of the immediate work-up.
- Medications for Rate Control — Beta-blockers are recommended as 1st-line for AFib rate control. Digoxin has a long history of being safe in pregnancy (assuming no preexcitation). Verapamil is a 2nd-line agent (and is favored over Diltiazem). And, if rate control with hemodynamic stability can be achieved — it may be reasonable to hold off decision of cardioversion, given a high percentage of patients who spontaneously convert to sinus rhythm within the first 24 hours of hospitalization.
- Amiodarone — should not be used in pregnancy (significant adverse effects).
| NOTE: I’ll recommend the above reference by Tamirisa et al — as this is a 2022 State of the Art Review by JACC on Arrhythmias in Pregnancy. This article contains detailed reference tables of specific drugs and treatments for the various arrhythmias during pregnancy. |
= = =
= = =
= = =