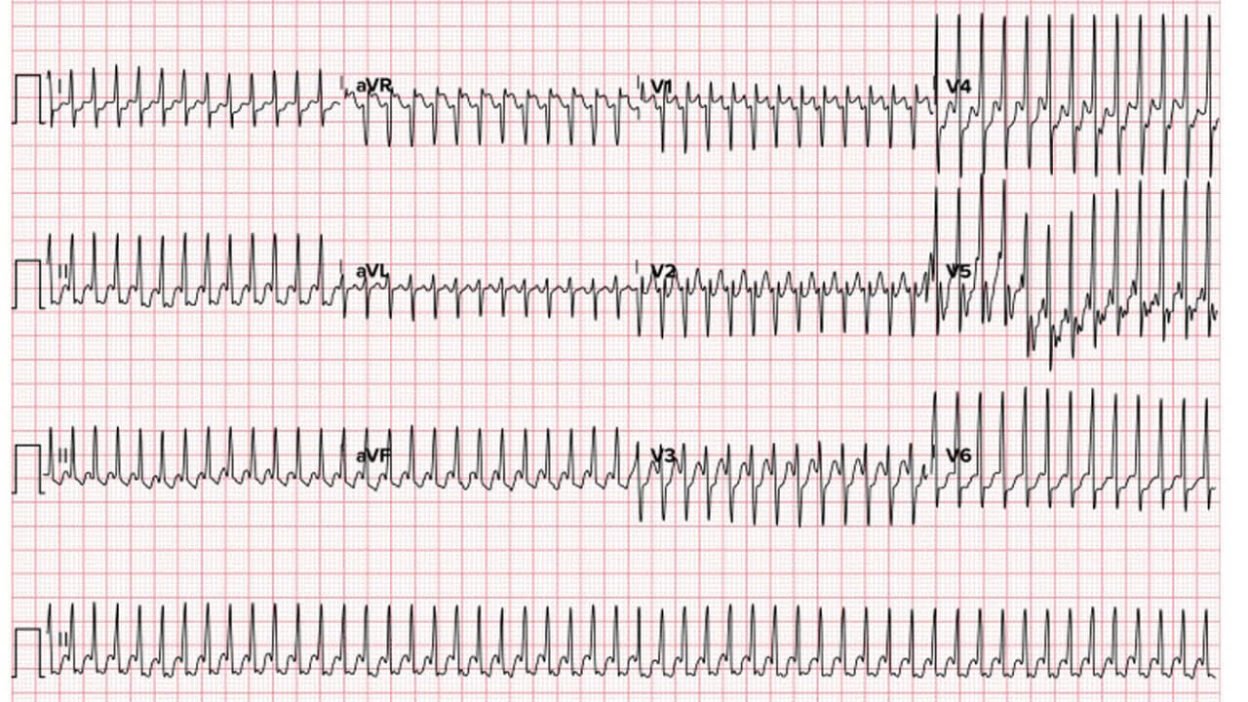
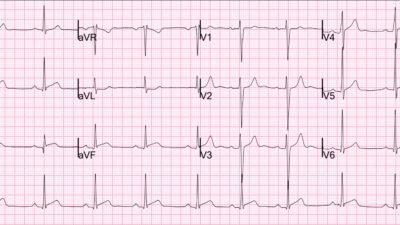
This was emailed to me by a reader with this info: 39-year-old male with no past medical history presents with 3 days of palpitations and 2 episodes of syncope in the past 8 hours.
(I later heard from a publisher that this is from their book and is copyrighted. The sender represented the ECG as from her own institution, and gave permission to use it. The publisher agrees to let me keep it here with attribution. I think the sender really believed that it came from a colleague at her own instutution. An honest mistake.)
This comes from this book, now with permisson:
What is it, and how did I respond?
My response: “Atrial flutter with 1:1 conduction. This AV node conducts too fast. Probably hyperthyroid.” You can see flutter waves at a rate just above 300, and a corresponding ventricular rate just above 100.
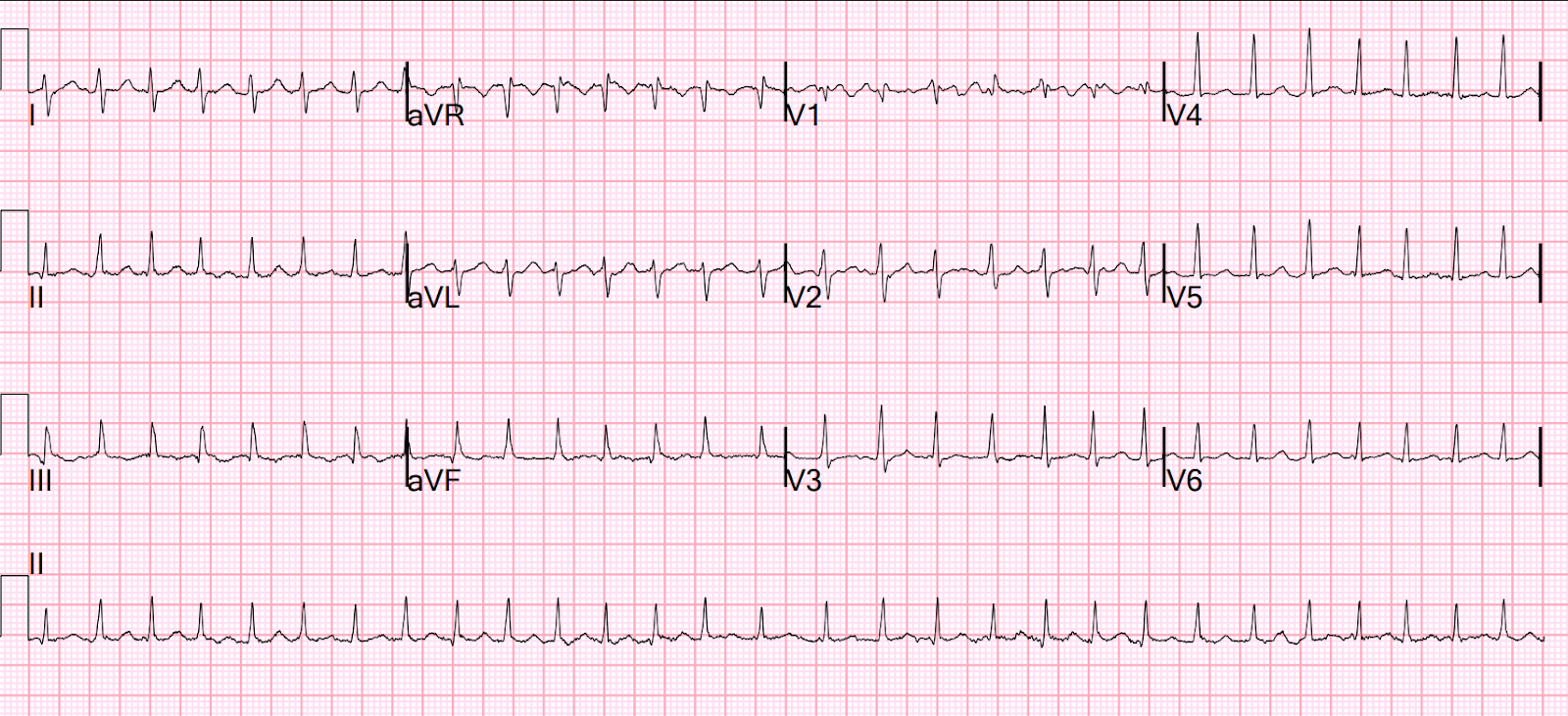
Case answer: This patient’s ED workup was consistent with thyroid storm. He was chemically cardioverted with adenosine after which he
briefly went into sinus tachycardia before going into atrial fibrillation with RVR at ~140 bpm. Atrial fibrillation is commonly seen with thyroid storm and will often be refractory to rate control or cardioversion until the elevated thyroid hormones are treated.
So was this extremely fast AVNRT, AVRT, or atrial flutter with 1:1 conduction? We may never know. Conversion after adenosine certainly makes one believe that it is AVNRT or orthodromic AVRT, but there do appear to be flutter waves. I think AVNRT or AVRT are most likely. In any case, the AV node is working VERY fast.
Learning point: K. Wang, who wrote the fantastic EKG Atlas (below) told me years ago that the only way an AV node can conduct at this accelerated rate is if the patient is hyperthyroid, which results in very high sympathetic tone.
The literature on this is scant. Other etologies of extreme catecholamine surge could (theoretically) do this as well, including sympathomimetic drugs, pheochromocytoma, etc.
Although such rapid conduction can be seen with an accessory pathway, that would not have such a narrow complex.
The therapy here is obvious: electrical cardioversion.
Online version of Dr. Wang’s Atlas (free)
See other cases of atrial flutter with 1:1 conduction. But all of them have a much slower atrial rate, often due to type 1 (usually 1c) antidysrhythmic, such as flecainide.
A young woman with palpitations. What med is she on? With what medication is she non-compliant? What management?
Challenging Rhythms in an 80-something Man
Narrow Complex Tachycardia at a Rate of 220
Wide-complex tachycardia that didn’t follow the rules
And still more
= = =
======================================
MY Comment, by KEN GRAUER, MD (Note that although I first published My Comment on 10/7 — I revised it on 10/8/2025):
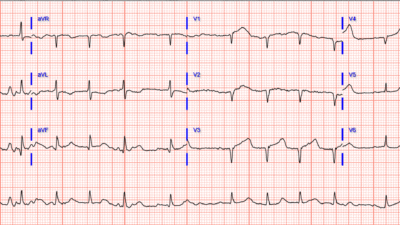
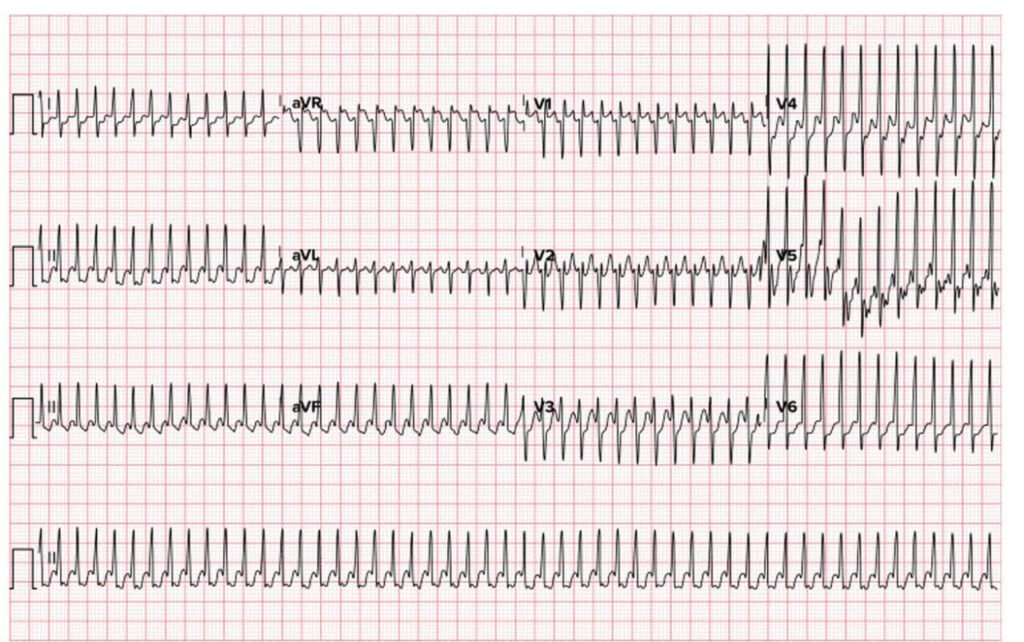
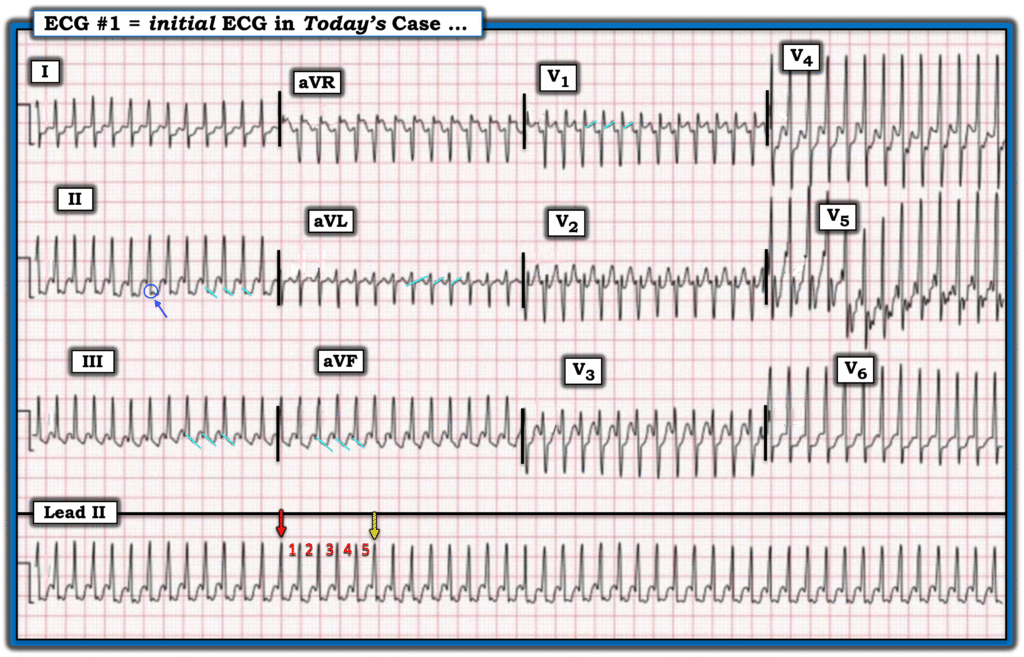
As per Dr. Smith’s initial reply — I also thought today’s ECG (that I’ve reproduced in Figure-1) suggested a single, immediate answer = AFlutter (Atrial Flutter) with 1:1 AV conduction. That said, to the differential diagnosis — I had to add AVRT (AtrioVentricular Reentry Tachycardia), in which an AP (Accessory Pathway) participates in the reentry circuit — as both orthodromic and antidromic forms of AVRT may on rare occasions reach SVT rates this fast.
- The rhythm in Figure-1 — is a regular, exceedingly fast narrow-complex tachycardia without clear sign of atrial activity. Although there does seem to be suggestion of a notching at the very end of the QRS complex in lead II (within the BLUE circle) — no such notching is seen in the other inferior leads, as it typically is when there is retrograde atrial conduction from a reentry SVT rhythm.
- That the indication of atrial activity is uncertain in Figure-1 should not be surprising — given how very fast the heart rate is (ie, There simply isn’t much place to put P waves given that the R-R interval is entirely taken up by the QRS and ST-T wave). Almost like an ambiguous image — after looking at this tracing multiple times, I wondered about 1:1 flutter waves ( = slanted light BLUE lines in leads II,III,aVF; aVL; V1). I finally concluded that atrial activity is uncertain.
- KEY Point: The heart rate in today’s tracing is over 300/minute! Note below in Figure-1 that I’ve placed a RED arrow precisely on an R wave occurring on a heavy grid line. Five large boxes later — we see that the 5th QRS complex occurs slightly before the 5th heavy grid line (the YELLOW arrow marking the R wave of the 5th QRS complex — that occurs before the 5th heavy grid line). This tells us that the R-R interval is a little less than 1 large box in duration — which means that the heart rate is over 300/minute!
- To Emphasize — AFlutter with 1:1 AV conduction is rare! That said, especially when 1:1 AFlutter presents with a ventricular rate as fast as we see in Figure-1 — this constitutes a medical emergency in need of immediate synchronized cardioversion.
- To Also Emphasize — AVRT typically does not go as fast as the rhythm in Figure-1. That said — it can on rare occasions attain rates of ~300/minute (and up to ~320/minute in infants and young children) — especially if conditions prompting extreme increases in sympathetic tone are ongoing.
- BOTTOM Line: I suspect the rhythm in Figure-1 is AFlutter with 1:1 AV conduction. That said — I cannot rule out an unusually fast AVRT.
= = =
Figure-1: I’ve reproduced today’s ECG to show that the R-R interval is slightly less than 1 large box in duration — which means that the heart rate is over 300/minute!
= = =
I Favor Atrial Flutter in Figure-1 …
In my experience — the most likely rhythm to produce a regular SVT (SupraVentricular Tachycardia) in an adult at a rate ≥300/minute is AFlutter with 1:1 AV conduction.
- The usual atrial flutter rate range in adults in untreated AFlutter is between 250-350/minute (most commonly very close to 300/minute). Because of an inherent “protective” function of the AV node — 1:1 AV conduction is rare. As a result, by far — the most common response of the AV node is to only allow 1 out of every 2 flutter impulses to conduct through the AV node. This explains why the usual ventricular rate with untreated AFlutter is close to 150/minute (300 ÷2 = 150/minute) — with the usual ventricular rate range in a patient presenting with untreated AFlutter being between ~130-to-170/minute.
- NOTE: I unfortunately do not have specific follow-up to the conclusion of this case — and therefore do not have a definite answer as to whether the etiology of the rhythm in Figure-1 is AFlutter with 1:1 AV conduction (as I suspect) — or an exceedingly fast AVRT. My comments below are based on my hunch that the rhythm is 1:1 AFlutter.
= = =
When Might You See AFlutter with 1:1 AV Conduction?
As stated above — AFlutter with 1:1 AV conduction is rare. That said — it can occur — and when it does, it is almost always in association with one or more of the following circumstances (See Murthy et al — BMJ Case Rep, 2013):
- The patient is on some kind of antiarrhythmic drug (most often, a Class IC agent such as flecainide or propafenone). This is because these agents slow the atrial rate of flutter — such that AFlutter at an atrial rate of say, 220/minute (instead of 300/minute) may be slow enough for the AV node to conduct 1:1 unless the patient is also taking an AV nodal blocking agent.
- KEY Point: Although taking a 1C agent is probably the most common predisposing cause 1:1 AV conduction with AFlutter — since these drugs slow the atrial rate of flutter — 1:1 AV conduction will typically not present with 1:1 AFlutter at a ventricular rate as fast as in today’s case! As a result — a patient on a 1C agent may be able to tolerate 1:1 AFlutter for longer than if the flutter rate is 300/minute.
Other Conditions that may predispose to 1:1 AFlutter:
- The patient may have an AP (Accessory Pathway) that allows faster conduction of atrial impulses to the ventricles.
- Hyperthyroidism is associated with greatly increased sympathetic activity that potentiates AV conduction (as was seen in today’s case).
- And, on rare occasions — exercise has been reported to cause 1:1 AV conduction of AFlutter (due to both an increased flutter cycle length of flutter waves, as well as to enhanced AV conduction from the increase in sympathetic activity). And while exercise alone is an unlikely culprit — in combination with an antiarrythmic drug, an accessory pathway and/or hyperthyroidism, this could be enough to precipitate 1:1 AFlutter.
CAVEAT #1: While one or more of the predisposing factors listed above will most often be associated with those rare cases of 1:1 AFlutter that do occur — a case report by Murthy et al ( BMJ Case Rep, 2013 ) describes a 50-year old man who presented with 1:1 AFlutter at the very rapid rate of 280/minute but without any predisposing conditions.
- NOTE: While I did encounter occasional other case reports of patients presenting with 1:1 AFlutter — most of these were in patients taking Class I antiarrhythmics, in whom the ventricular rate of AFlutter was usually significantly slower than the rate of today’s patient.
= = =
CAVEAT #2: Be aware that when the ventricular rate of 1:1 AFlutter is very fast — that the QRS may widen as a result of rate-related aberrant conduction. Snipes et al looked at 8 patients not on antiarrhythmics and without preexcitation — who presented with 1:1 AFlutter disguised by QRS widening that understandably prompted a misdiagnosis of VT ( J Innov Card Rhythm Manag 15(10):6041-6046, 2024 ).
- P.S.: Presumably the reason this study by Snipes et al consisted of only 8 patients — is that AFlutter with 1:1 AV conduction is rare, so very difficult to find patients to include in a study … That said — the “Take-Home” Point of this small patient sample is to be aware that 1:1 AFlutter with rate-related aberrant conduction may simulate VT (and probably does so more often than we realize).
A Final Consideration in Today’s Case:
Today’s Patient was a previously healthy 39-year old man who presented with 3 days of palpitations, including 2 syncopal episodes.
- It’s important to be aware of the entity known as TCM (Tachycardia-induced CardioMyopathy) — in which left ventricular dysfunction may develop solely as a result of a persistently increased heart rate.
- In Huizar, Ellenbogen et al’s review of this subject ( JACC 73:2328-2344, 2019 ) — they cite a highly variable duration of tachycardia in patients who went on to develop TCM, with a duration as short as 3 days being enough to result is depressed LV function.
- The “good news” — is that many (most) patients with TCM recover LV function once the tachycardia is controlled (usually within 1-3 months) — with this providing proof that the persistent rapid heart rate was in fact the cause of the patient’s cardiomyopathy.
- Regarding today’s patient, given the duration of symptoms prior to presenting in the ED ( = 3 days of palpitations, including 2 syncopal episodes) — assessment of LV function will be an essential part of management.
= = =
Learning Points:
- It is rare to see a regular SVT (ie, narrow-complex tachycardia) at a rate of ≥280/minute in an adult. That said, as shown in today’s case — this phenomenon does occur, especially if there is predisposition to such rapid rates because of hyperthyroidism, an accessory pathway, excessive sympathetic tone.
- Clear sign of atrial activity will usually not be seen in SVT rhythms at this fast of a rate — and if present, it will usually not be diagnostic (as in today’s tracing). In these cases — the rhythm diagnosis is between AFlutter with 1:1 AV conduction vs AVRT.
- Distinction between 1:1 AFlutter vs AVRT is not critical to initial management — since both rhythms respond to immediate cardioversion, which will often be the treatment of choice.
- Adenosine would be expected to convert AVRT — whereas it is unlikely to convert 1:1 AFlutter. However, it may slow conduction of impulses through the AV node with AFlutter — resulting in a short-lived reduction in heart rate that might help diagnostically by revealing underlying flutter waves. Whether the provider will be comfortable administering IV Adenosine to a patient in a regular SVT rhythm at extreme rates (ie, >280/minute) is something for which, “Ya gotta be there”.
- Definitive care depends on whether a treatable cause of the rhythm is found (ie, hyperthyroidism) — and if not, refer for EP testing and probable ablation.
= = =
= = =