Sent by anonymous, written by Pendell Meyers
A woman in her 50s presented with acute chest pain and shortness of breath.
She appeared well with normal vital signs.
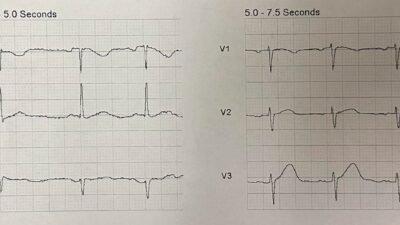
Here is her triage ECG:

What do you think?
The ECG shows sinus rhythm with normal QRS complex and signs of acute LAD occlusion. This ECG shows the Precordial Swirl sign that we coined and published here. It includes STE and/or HATW in V1-V2, with reciprocal STD and/or TWI in V5-V6. At the time we submitted this manuscript, we didn’t yet have the ability to automatically quantify HATW. As the best available alternative, we described a T wave to S wave ratio of 0.40 or more, which is very clearly exceeded in V2 in this case.
Smith: Precordial swirl is an LAD occlusion proximal to the first septal perforator, such that not only is most of the LAD Territory at risk, but the septum is ischemic, with corresponding ST elevation from left to right in the septum resulting in STE in V1, which overlies both the septum and the RV (RV MI can also mimic precordial swirl). All explained here in this post from 2013, with diagram, before we coined the term “precordial swirl”. Septal STEMI with ST elevation in V1 and V4R, and reciprocal ST depression in V5, V6
Smith: There is also evidence of inferior OMI in lead III, with STE and HATW, but with STD in I, II, aVF, V4-6. This suggest additional Aslanger’s pattern: both at once? This is academic, as OMI is already obvious and cath lab activation required.
Some cases of Aslanger’s pattern here, and here.
Case continued: Unfortunately the ECG was interpreted by the treating physician as “minimal ST depression in the lateral leads”, so routine chest pain workup was initiated.
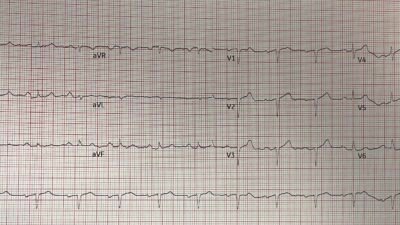
Here is what the physician would have seen during triage if they used the Queen of Hearts:

PMcardio for Individuals now includes the latest Queen of Hearts model, AI explainability (blue heatmaps), and %LV Ejection Fraction. Download now for iOS or Android: https://individuals.pmcardio.com/app/promo?code=DRSMITH20. As a member of our community, you can use the code DRSMITH20 to get an exclusive 20% off your first year of the annual subscription. Disclaimer: PMcardio is CE-certified for marketing in the European Union and the United Kingdom. PMcardio technology has not yet been cleared by the US Food and Drug Administration (FDA) for clinical use in the USA.
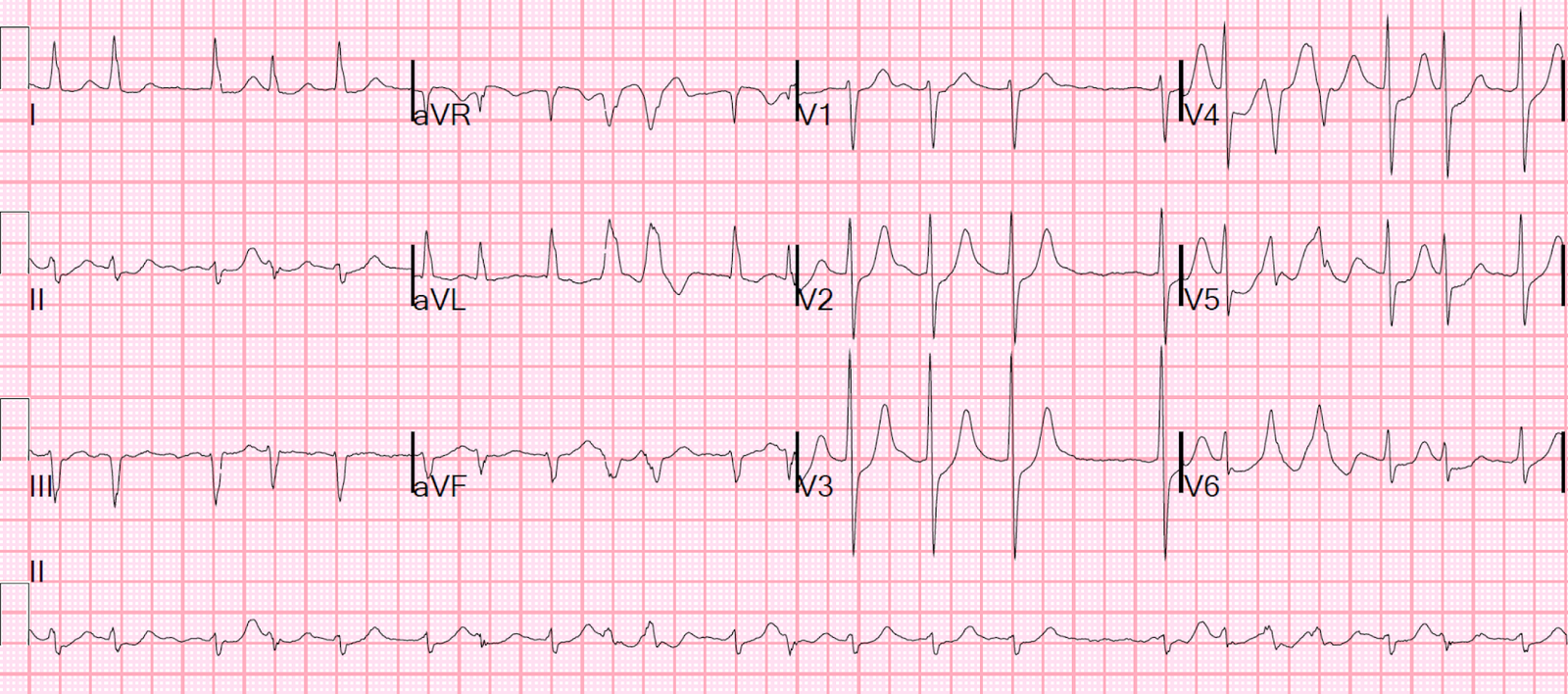
But instead the patient did not receive any repeat ECG until about 40 minutes later:


Because it was now recognized as “STEMI”, the cath lab was activated.
The patient had multiple episodes of ventricular fibrillation cardiac arrest in the cath lab.
The angiogram revealed ostial LAD occlusion (TIMI 0), which was successfully opened and PCI performed.
Unfortunately, cardiogenic shock progressed and the patient did not survive the hospitalization despite aggressive care.
See more cases of Precordial Swirl here:
= = =
======================================
MY Comment, by KEN GRAUER, MD (11/14/2025 ):
From an ECG interpretation viewpoint — I felt “gratified” on reading the interpretations by Drs. Meyers and Smith regarding today’s initial ECG — as my immediate thoughts left me unable to distinguish between Precordial Swirl vs Aslanger’s Pattern (with inferior MI, perhaps in association with acute RV involvement — to explain the ST elevation in lead V1) — with me also thinking (as per Dr. Smith) how it would seem unusual for both these conditions to occur simultaneously — at which point I thought to myself, “It’s an obvious OMI with need for prompt cath regardless … “.
- The above reflects my “academic” thoughts that came to me within seconds on seeing this interesting tracing.
- My personal thoughts were very different. I thought, “How frustrating — as the initial ECG tells us that some kind of acute event is clearly ongoing — and should not have been overlooked, as it was. And this patient died …”. While impossible to say if the patient might have survived had intervention been quicker — there are difficult but important lessons to be learned from this case.
= = =
Today’s Initial ECG:
Asis often the case — the history provides the 1st clue that “something” acute is ongoing ( = New-onset chest pain and shortness of breath in a patient with a relatively fast heart rate of nearly 90/minute). This history places the onus on us to rule out rather than to rule in an acute event.
- For clarity in Figure-1 — I’ve labeled today’s initial ECG. My “eye” was immediately drawn to the 2 leads within the RED rectangle. In a patient with new CP (Chest Pain) — there is simply no way that the coved ST elevation in lead V1 can be normal in an ECG without LVH and without QRS widening!
- That the QS wave in lead V1 is significant until proven otherwise — is supported by the subtle-but-present Q wave in neighboring lead V2 (BLACK arrow in V2). Given how tiny the QRS complex is in lead V2 — the unusually “fat” T wave in V2 is disproportionately “bulky”, and in association with the ST elevation in lead V1, is supportive of something acute that is ongoing.
- Drs. Meyers and Smith highlight 20 cases of Precordial “Swirl” (and/or “Swirl” look-alikes) in the October 15, 2022 post in Dr. Smith’s ECG Blog. At the bottom of the page in this Oct. 15, 2022 post — I highlight the distinct characteristics to look for in leads V1,V2 and V5,V6 that “make” the diagnosis of Swirl. Today’s initial ECG fits this description perfectly ( = different-than-expected shape to the ST elevation in lead V1 — most often with a flattened appearance to the depressed ST segment in V5,V6).
- On the other hand (as per Dr. Smith) — today’s initial ECG also fits perfectly with Aslanger’s Pattern (See the January 4, 2021 post) — because there is ST segment straightening with subtle ST elevation seen in lead III, but not in the other 2 inferior leads (leads II,aVF). It is the simultaneous occurrence of DSI (Diffuse Subendocardial Ischemia) in association with acute inferior OMI that produces the pattern seen in today’s ECG — in which there is ST flattening and depression seen in multiple leads (leads I,II,aVL,aVF,V4,V5,V6) with ST elevation in leads III, aVR and V1. If today’s ECG does in fact represent Aslanger’s Pattern (with DSI + simultaneous inferior MI) — I thought the extra amount of ST elevation in lead V1 might then reflect associated RV involvement.
BOTTOM Line (as per Drs. Meyers and Smith) — The history in today’s case of new CP and this initial ECG should prompt the need for immediate cath to define the anatomy and provide PCI.
- While the ST elevation in lead III is subtle — the ST elevation in lead V1 — and, the diffuse ST segment flattening and depression in multiple other leads (with ST elevation in lead aVR) are ECG findings that should not be missed.
- For any doubt about the above findings — the ECG should have been immediately repeated. Instead, 40 minutes passed before repeating the ECG. This case illustrates how quickly the acute proximal LAD occlusion of “Swirl” may sometimes progress — with the very unfortunate consequence of the patient’s demise.
= = =
Figure-1: I’ve labeled the initial ECG in today’s case.