My partner brought me this ECG during a shift, not sure how to interpret it.
A 65 y.o. male with a past medical history significant for coronary artery disease, STEMI, NSTEMI, DVT, PE presented to the ED with chest pain and palpitations. Patient reported that about an hour and a half ago he started to have a funny feeling in his chest patient reported that the pain at the time was about 3 out of 10. This pain increased drastically to a 7 out of 10 radiated down his left arm felt stabbing in nature and he began sweating. At this moment time the patient became concerned and called an ambulance.
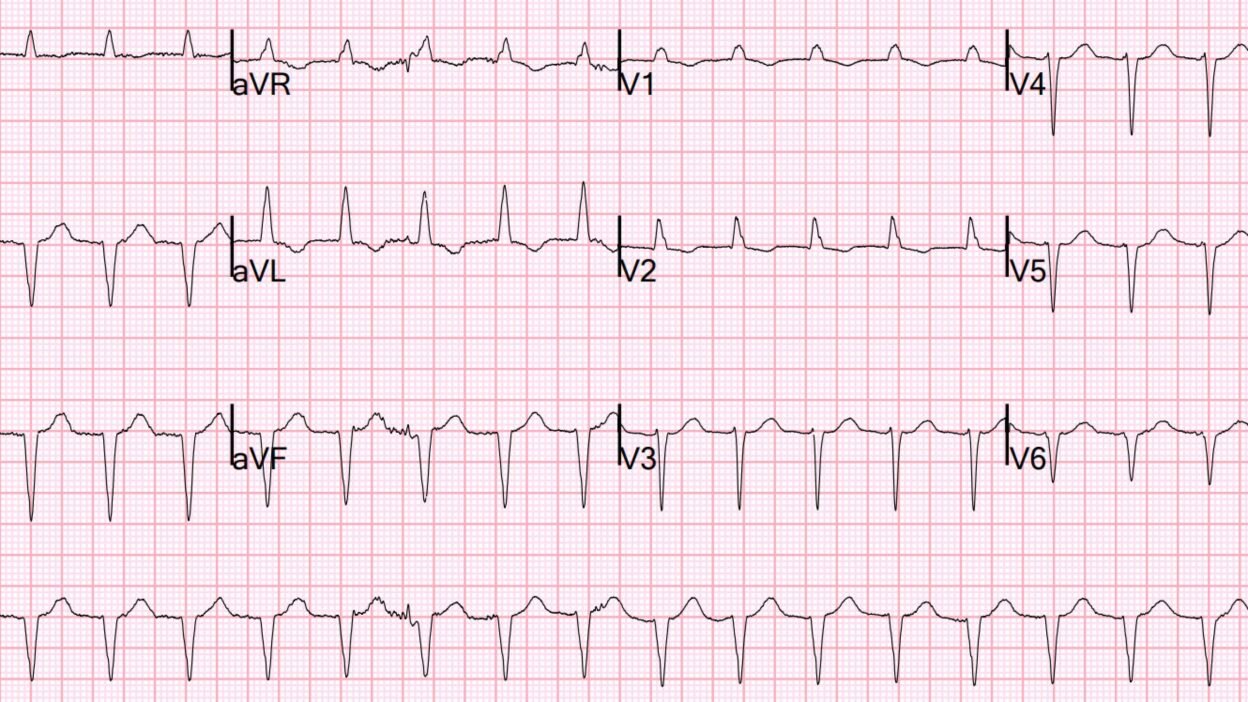
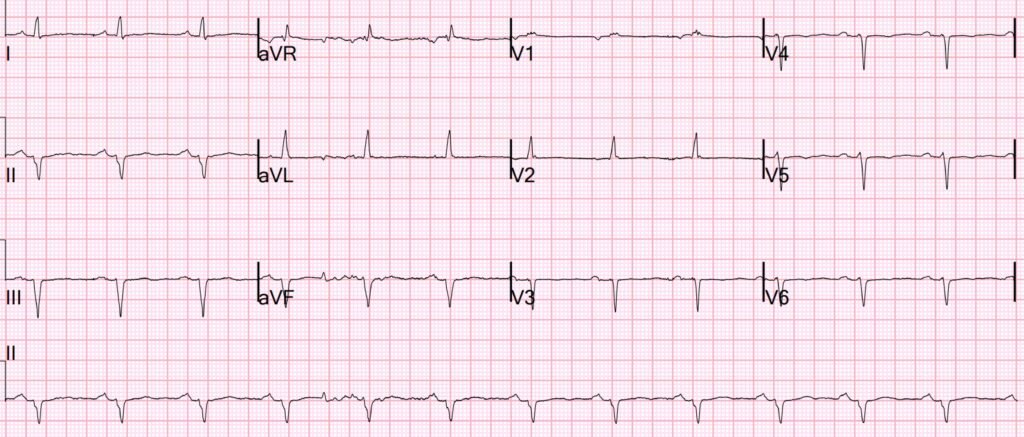
Here is his initial ED ECG:
What do you think?
There is no evidence for OMI. But what is the rhythm? It is slightly fast (118), regular, appears slightly wide but really is only about 120 ms. There are no P-waves, no flutter waves. It looks too slow for SVT. Is it possibly some sort of ventricular tachycardia (VT)?
It is quite slow for VT, but very slow for PSVT (AVNRT or AVRT). There are no baseline flutter waves, and it would also be slow for flutter with 2:1 conduction. It cannot, of course, be atrial fibrillation because it is regular.
For any regular tachycardia, even if you think it might be VT, adenosine can be given (although it is best to avoid giving it to sinus tach!). It will not work for VT. For flutter, it will slow AV conduction and reveal flutter waves; see this post: What happens when you give adenosine to a patient with this rhythm?
For PSVT (AVNRT or AVRT), it is highly likely to terminate that rhythm, since those rhythms are re-entrant and dependent on the AV node.
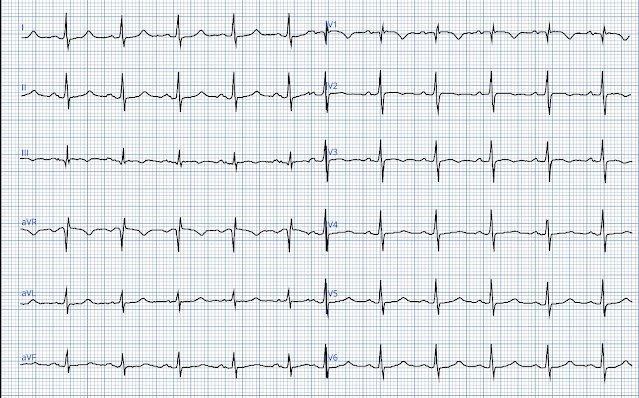
Here is what the PM Cardio app says:
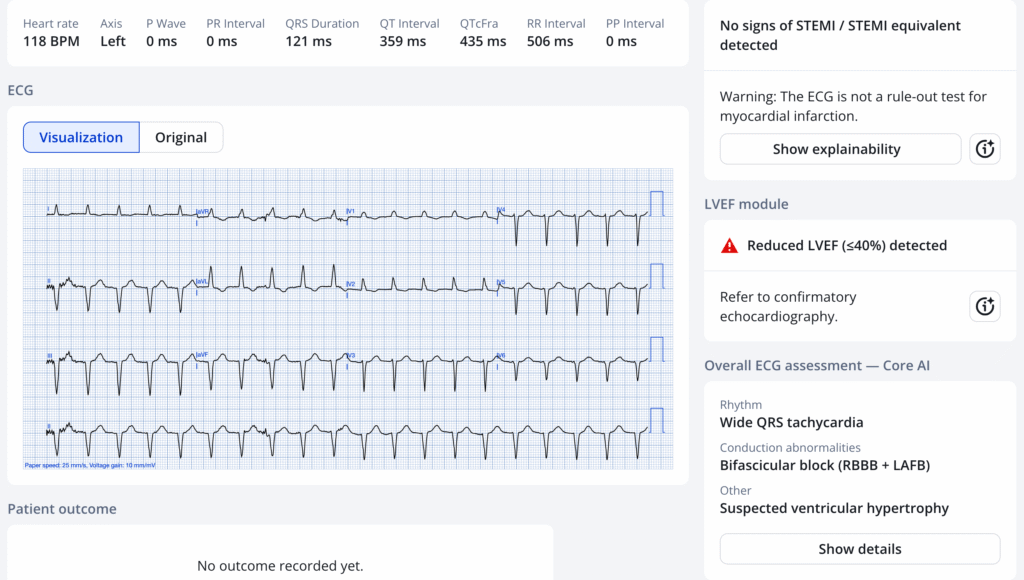
You can see that for rhythm, she only says “wide complex tachycardia”, but does not say what the rhythm is. However, by indicating RBBB and LAFB, the implication is that it is supraventricular.
New PMcardio for Individuals App 3.0 now includes the latest Queen of Hearts model and AI explainability (blue heatmaps)! Download now for iOS or Android. https://www.powerfulmedical.com/pmcardio-individuals/ (Drs. Smith and Meyers trained the AI Model and are shareholders in Powerful Medical.)
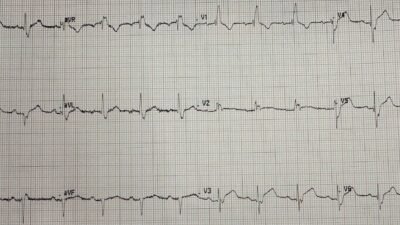
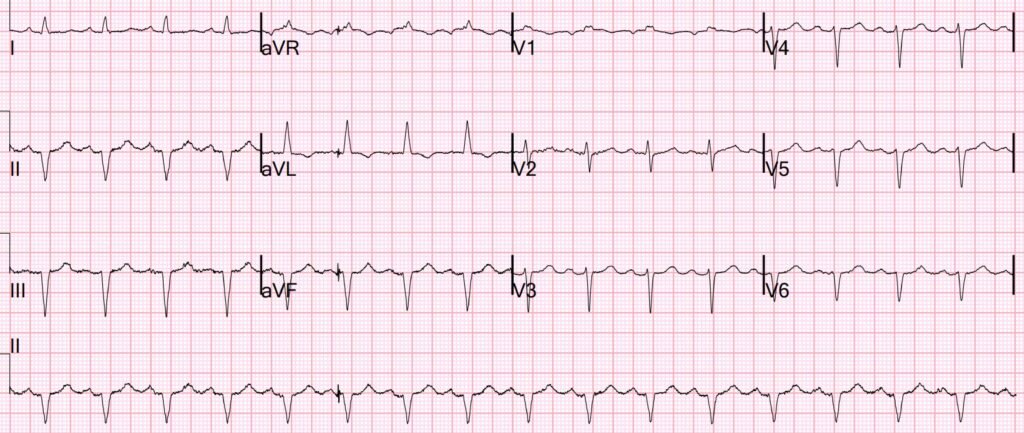
However, if you can find an old ECG, it may be very helpful:
What do you think?
This is clearly sinus rhythm, a supraventricular rhythm. The QRS complexes are identical to the QRS complexes above, proving that the presenting ECG is supraventricular tachycardia. It could still possibly be atrial flutter at a slow flutter rate of 236, with 2:1 conduction, but much less likely.
Therefore, adenosine was given:
Sinus rhythm now. Successful conversion with adenosine.
Diagnosis: PSVT. Probably slow AVNRT. The patient was not on any medications that would cause a slow AVNRT.
======================================
MY Comment, by KEN GRAUER, MD (7/21/2025):
Among the most instructive cases are those from patients, “who don’t read the textbook”. I was therefore intrigued by today’s case — which once again shows that almost always is not 100%.
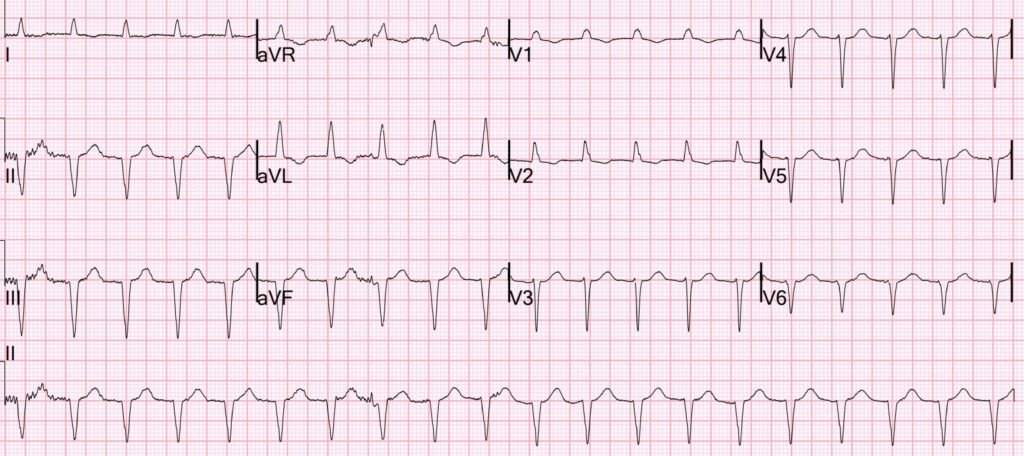
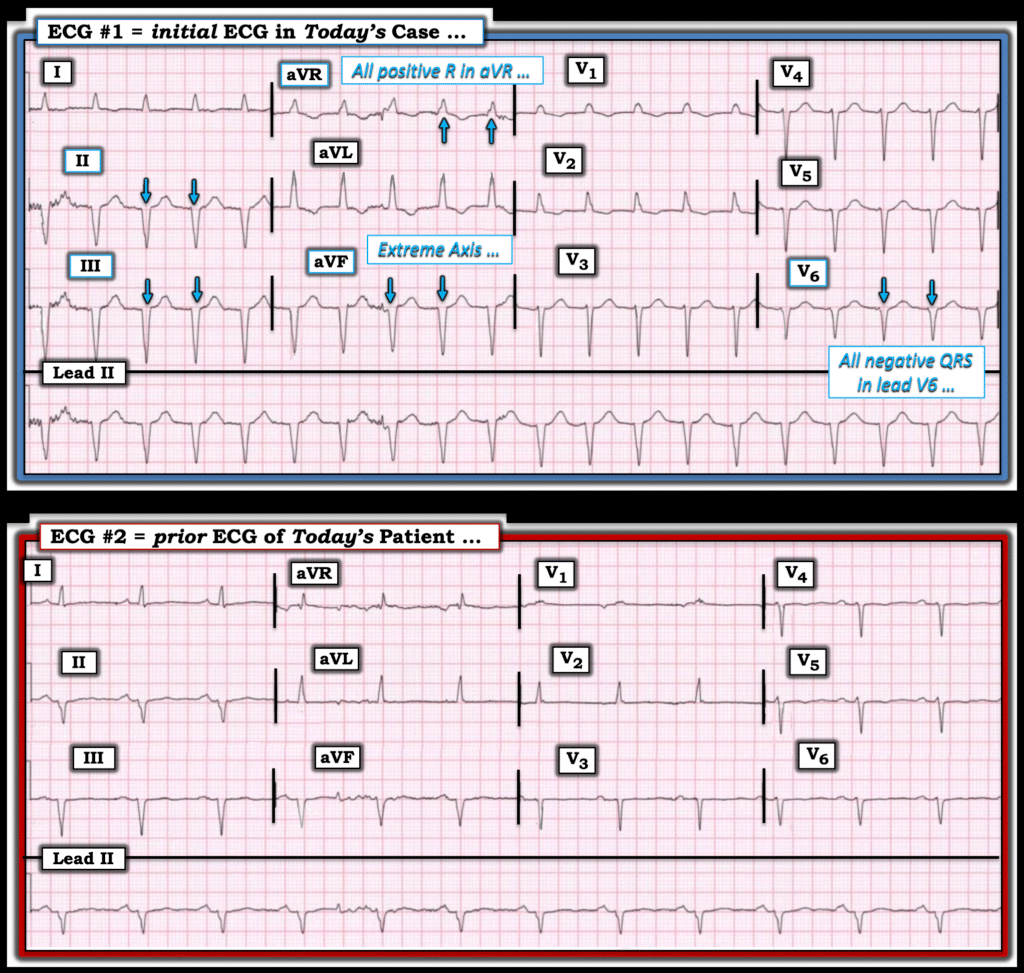
- For clarity in Figure-1 — I’ve reproduced the first 2 ECGs in today’s case.
What is the Rhythm in the Initial ECG?
Today’s initial ECG qualifies as a regular WCT (Wide-Complex Tachycardia) — which generally means that we need to assume VT until proven otherwise. That said — Dr. Smith appropriately adds the caviats that: i) The QRS in ECG #1 is not nearly as wide as most VT rhythms are (some fascicular VTs may only be 0.11 second in duration — which is why I define “wide” in adults as ≥0.11 second in duration) — and, ii) The rate of the initial ECG in today’s case is not overly fast at 118/minute (which is a ventricular rate that really falls within the “gray zone” between a faster Accelerated IdioVentricular Rhythm vs a true VT rhythm).
- For these reasons — Dr. Smith appropriately asks, What is the rhythm?
Figure-1: Comparison between today’s initial ECG — and a prior ECG.
Almost Always is Not 100%
Despite the caviats in ECG #1 of a minimally widened QRS and the slower-than-expected ventricular rate — I initially thought the rhythm was VT.
- Given the patient’s age (65-years old) and the known history of significant coronary disease — statistical odds very strongly favor VT as the diagnosis until proven otherwise.
In addition — a number of my “Go-To” criteria that almost always indicate VT as the etiology for a regular WCT are present in ECG #1. These include:
- Extreme Axis Deviation — which I define as an entirely negative QRS in either lead I and/or lead aVF (present in ECG #1 in each of the inferior leads).
- An entirely negative QRS in Lead V6 — which generally indicates no electrical activity directed toward the left (therefore suggesting electrical activity begining from below, or in the ventricles).
- An entirely positive R wave in lead aVR — similar to an all negative QRS in lead V6, and suggesting electrical activity arising from the apex in the ventricles.
- No resemblance to any known conduction defect — QRS morphology in ECG #1 resembles neither RBBB (no wide terminal S wave in lateral lead I — and essentially all negative QRS complexes from V3-thru-V6) — nor LBBB (ruled out by the positive R in V1 and the all negative QRS in V6).
And then a previous ECG on this patient was found! (ECG #2 in Figure-1).
- The prior ECG in Figure-1 shows sinus rhythm (upright P waves with constant PR interval thoughout the long lead II rhythm strip). It also shows an essentially identical QRS morphology in all 12 leads as was seen in the initial ECG — thereby proving the initial rhythm is supravenricular!
Learning Points:
- On occasion — a bizarre or otherwise highly unusual QRS morphology may be present with sinus rhythm in a baseline tracing. Development of a reentry SVT rhythm (AVNRT, AVRT) in such a patient will be regular, fast, will not manifest sinus P waves — and will therefore look like VT. Such was the case with today’s patient — in whom extensive previous infarctions was the reason that 7/12 leads lack appreciable R waves.
- Although some fascicular VTs may manifest a QRS duration of 0.11 second — most VTs will be wider ( = a hint that VT was not the cause of the initial rhythm in today’s case).
- And because QRS duration of today’s initial tracing was not more than 0.11 second — the fact that QRS morphology does not resemble either of the common forms of fascicular VT (ie, no rbbb/lahb and no rbbb/lphb pattern) — is another hint that VT is not the cause of today’s initial rhythm.
- Although most reentry SVT rhythms (ie, AVNRT, AVRT) will be faster than 120/minute — they can be slower (automatic ectopic tachycardias may also occasionally be slower, in the range of 100-110/minute).
- Today’s patient presented with severe CP. A tachycardia may sometimes be the cause of new CP (which can be established as the cause IF the patient’s CP suddenly resolves after restoration of sinus rhythm! ).
- Almost always is not 100% … As helpful as ECG criteria may be for distinguishing between VT and supraventricular rhythms — some patients “do not read the textbook”, so there can always be exceptions. Ready access to a prior ECG on your patient can be invaluable (although most of the time this will not be available to you at the time you need to begin treating the regular WCT patient in front of you).
=========================