A male in his 60s presented complaining of dysnpea and chest pain. He was tachypneic and ill appearing.
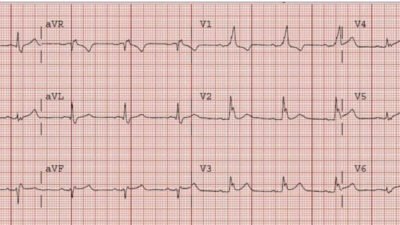
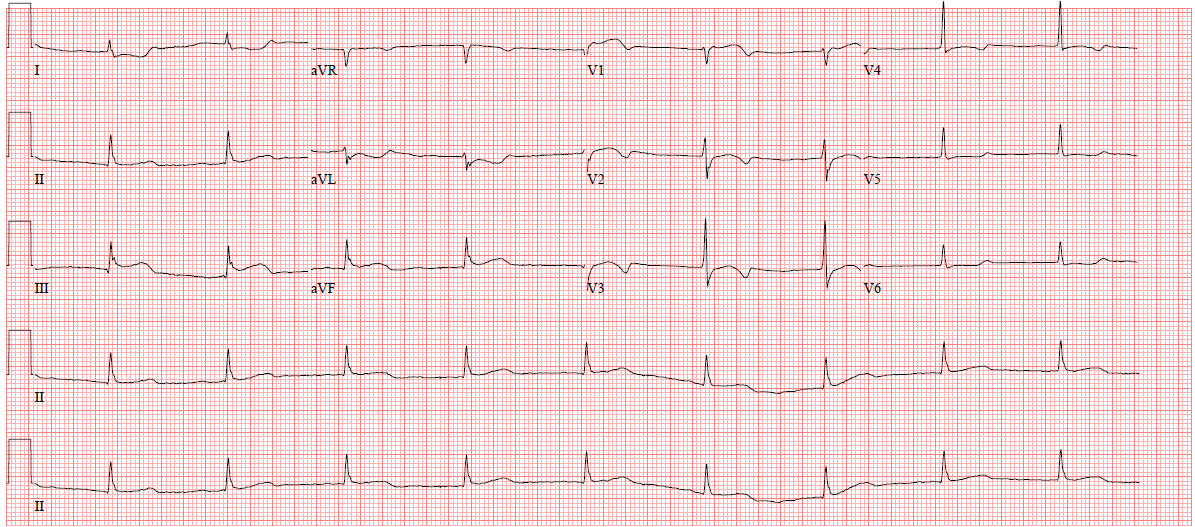
I was texted this ECG. The physician worried about PE mostly, but also MI:
 |
| My response was: “incomplete RBBB. No evidence of acute MI. Certainly could be PE. What does the cardiac echo show?” |
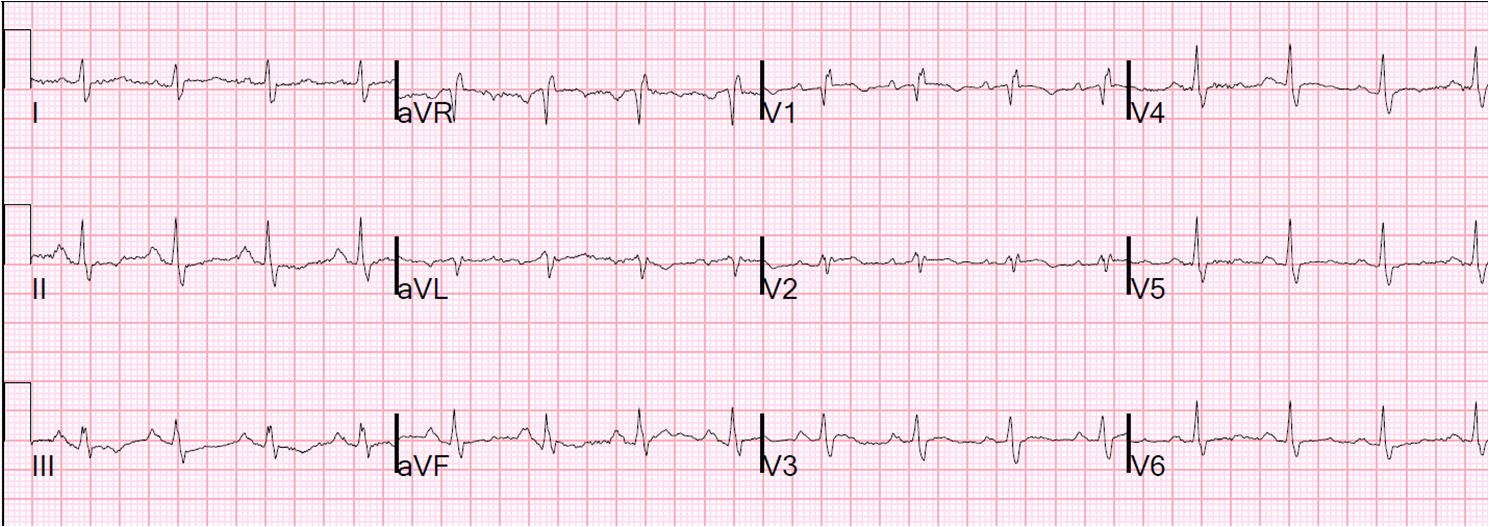
The bedside echocardiogram showed a serpiginous echogenic structure in the right atrium that was also flowing in and out of the right ventricle. The RV was enlarged.
I am sorry that I had to take this video down because my colleague wants to submit it to an academic journal. I have left the still frame in.
 |
| Still frame of the video: Blue circle show thrombus snaking throughout right atrium and right ventricle. |
The patient was given IV tPA and rapidly improved. A subsequent ultrasound showed no more thrombus.