An elderly woman with h/o diabetes and prior MI with a stent presented with acute nausea and vertigo to a very remote hospital where acute OMI must be given thrombolytics prior to transfer.
My former resident, Max Goder-Reiser saw her and, knowing that acute MI (OMI) can present without chest pain (especially in patients with Diabetes), and knowing that the patient has coronary disease with a previous stent, he was worried about acute MI and immediately recorded an ECG:
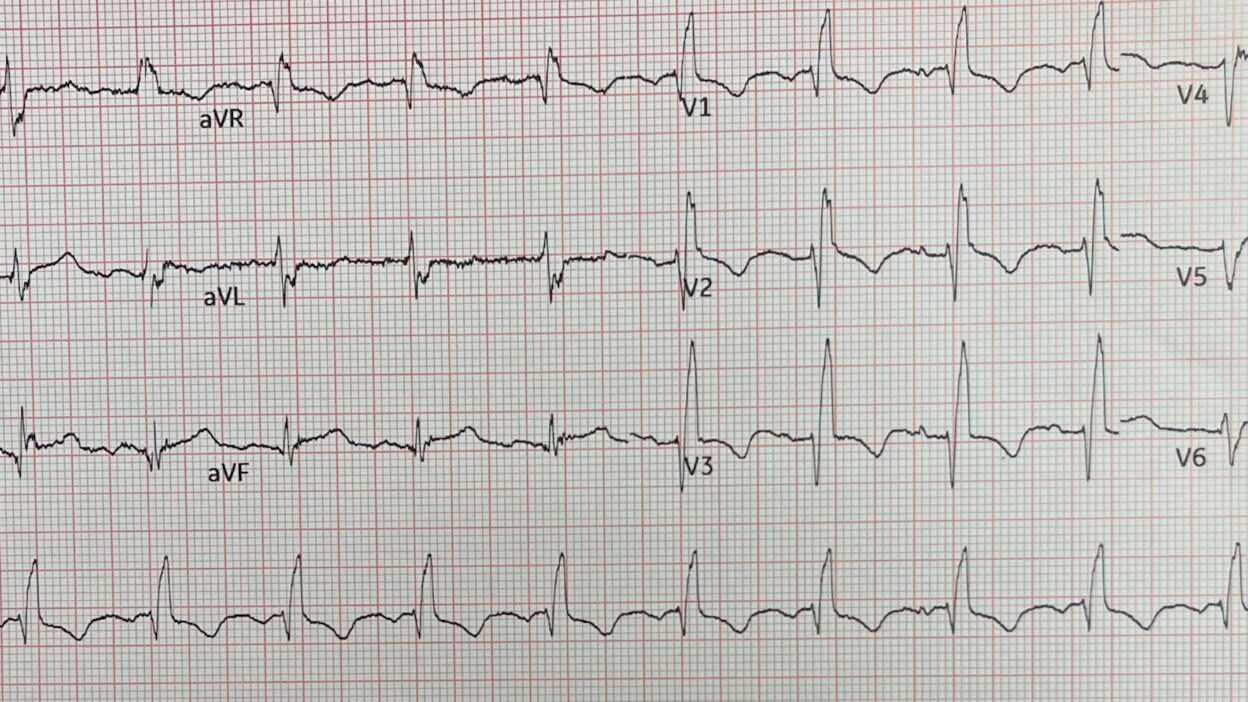
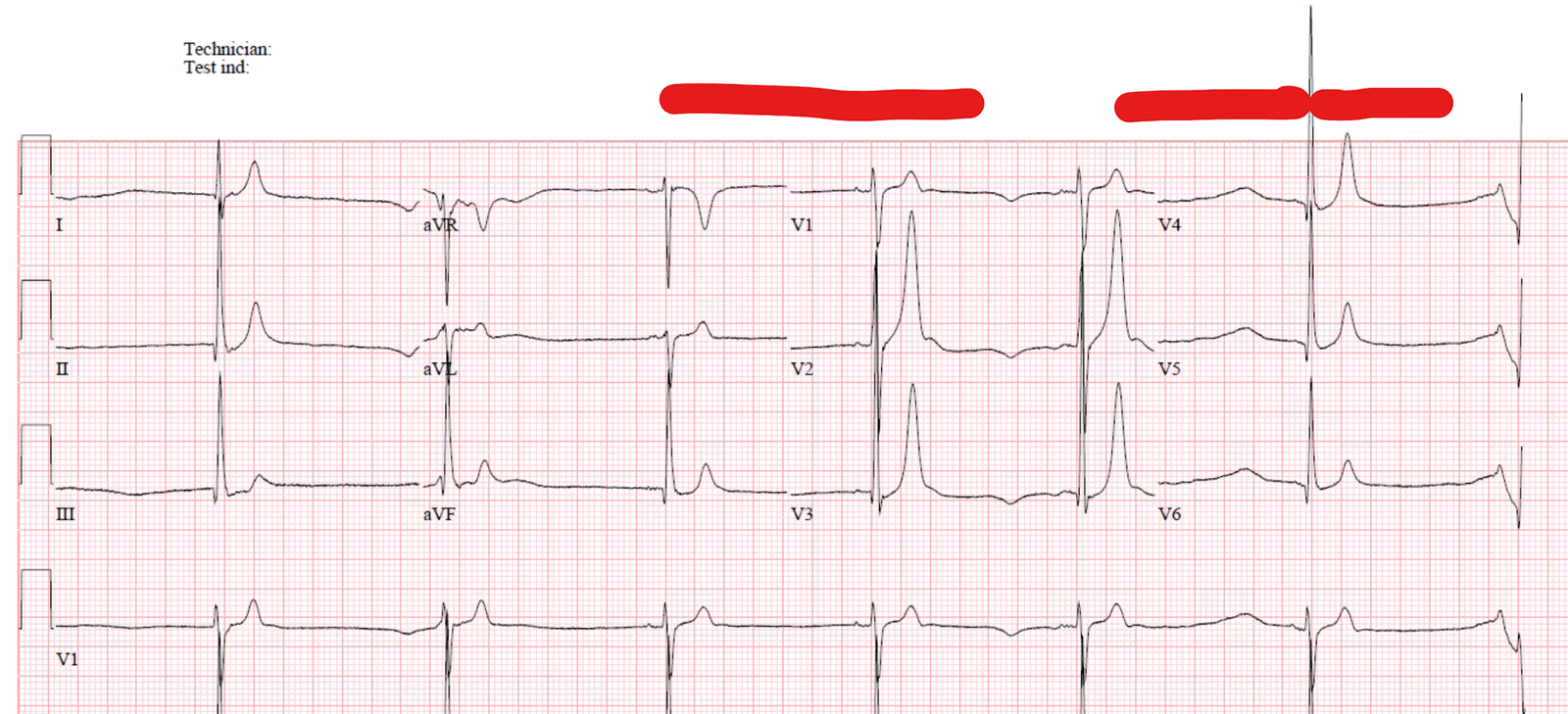
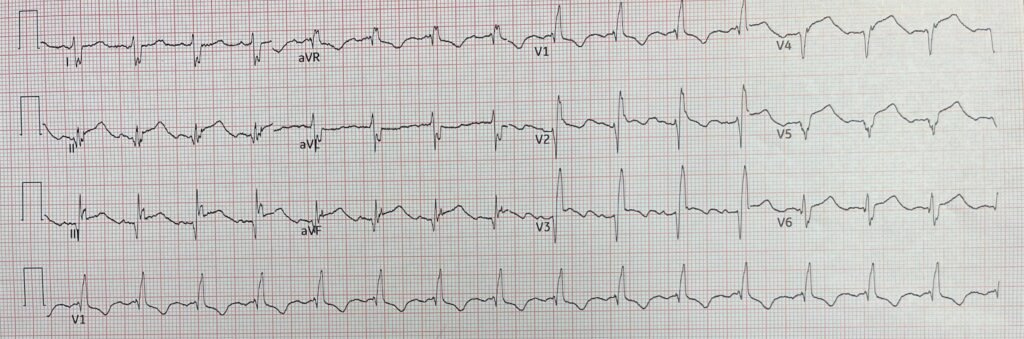
This is the initial 12-lead:
What do you think?
There is RBBB and Left Posterior Fascicular Block. There is no ST elevation that meets STEMI millimeter criteria. But Max was very concerned for LAD OMI with wraparound to the inferior wall due to STE in inferior leads and V4-6. Of course he was also concerned about overdiagnosis OMI because the patient was not complaining of chest pain. Bifascicular block in LAD OMI is a very ominous sign.
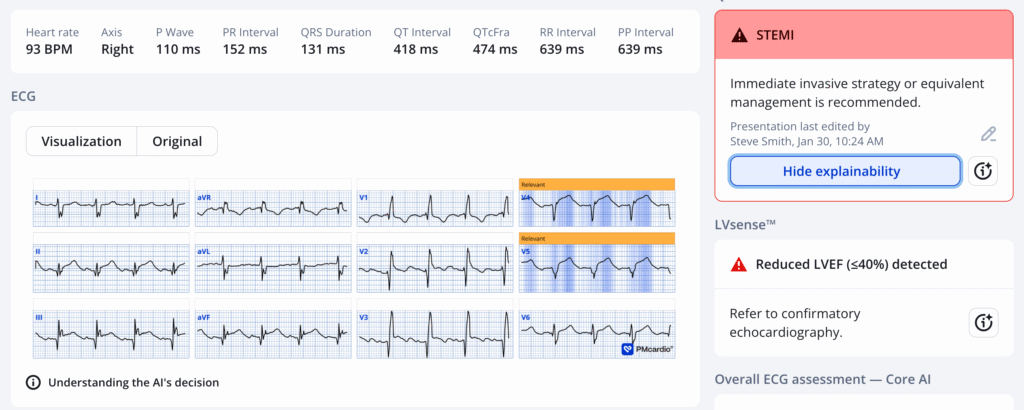
Max used the PMCardio Queen of Hearts AI ECG OMI Model:
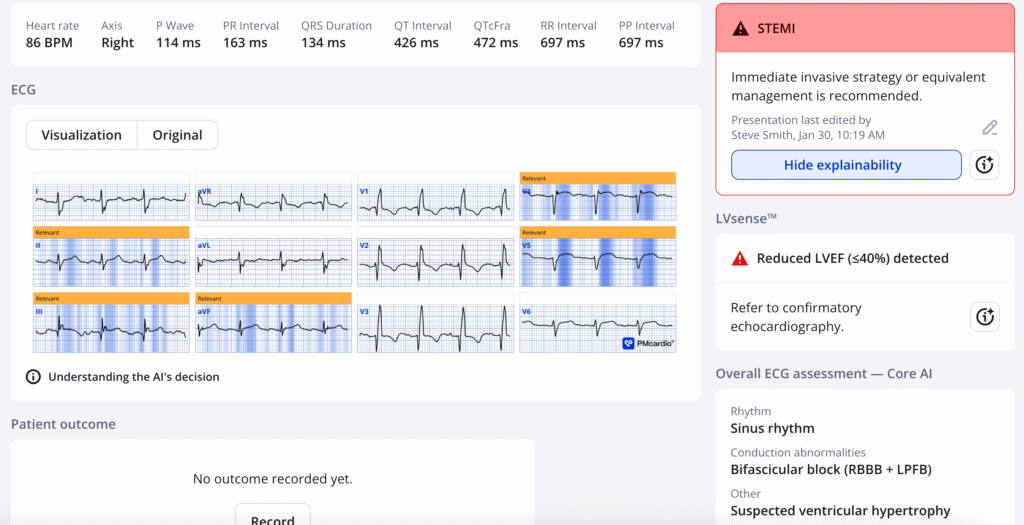
She sees it all, and diagnoses “STEMI Equivalent” (OMI) with a certainly of 0.91 (>98% specific).
Score interpretation: [> 0.5 for all comers is 98% specific; 0.5-0.67 is low confidence; 0.67-0.84 is mid-confidence 98% specific; 0.84-1.00 is > 98% specific; 0.30 – 0.50 is indeterminate.]
New PMcardio for Individuals App 3.0 now includes the latest Queen of Hearts model and AI explainability (blue heatmaps)! Download now for iOS or Android. https://www.powerfulmedical.com/pmcardio-individuals/ (Drs. Smith and Meyers trained the AI Model and are shareholders in Powerful Medical). As a member of our community, you can use the code DRSMITH20 to get an exclusive 20% off your first year of the annual subscription. Disclaimer: PMcardio is CE-certified for marketing in the European Union and the United Kingdom. PMcardio technology has not yet been cleared by the US Food and Drug Administration (FDA) for clinical use in the USA.
Max questioned the patient about chest discomfort and she denied any at all.
Nevertheless, Max wanted to give thrombolytics. He called the cardiologist at a distant referral center and she said “It is not a STEMI” and was adamantly opposed to giving thrombolytics.
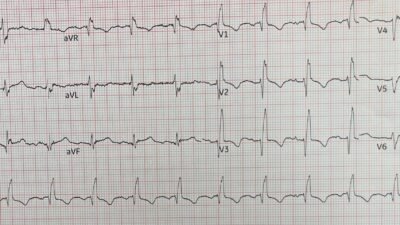
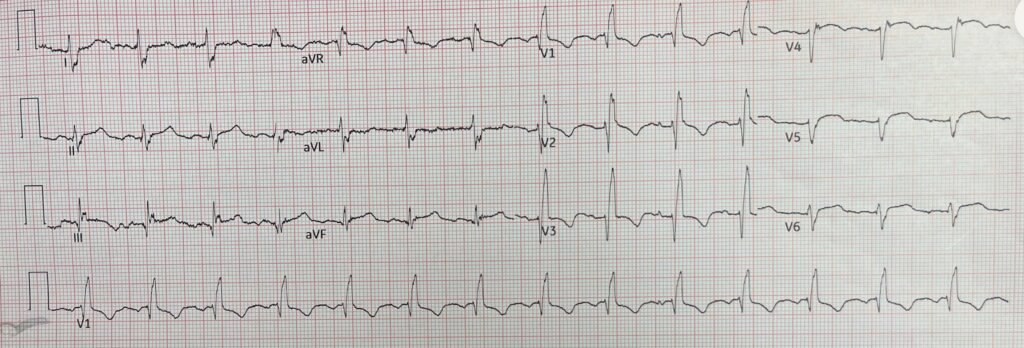
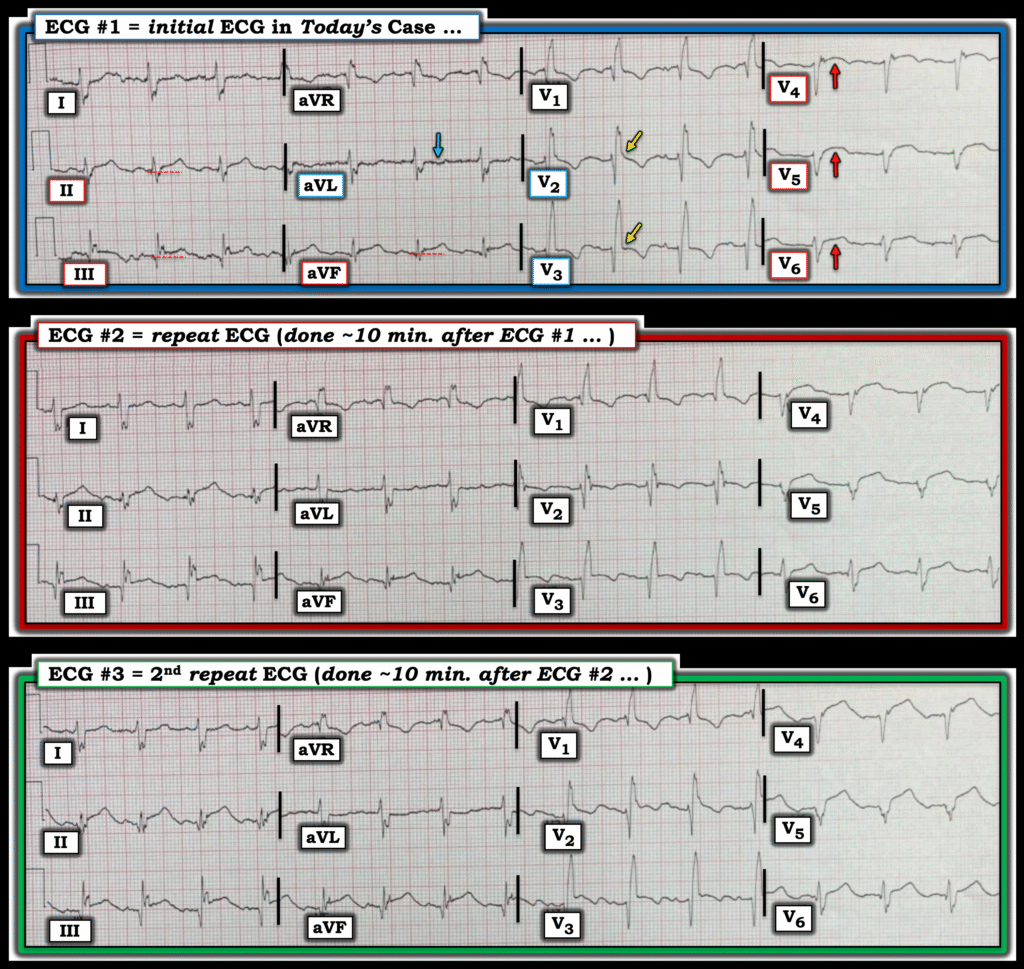
So Max recorded another ECG at 10 minutes:
Now the STE is greater and meets STEMI criteria, There is now a trace of concordant STE in V3 (ST segment should never be concordant to the R’-wave in RBBB), and the T-wave in V4 has turned upright. The Queen gives a result of 0.95 on this one (higher confidence)
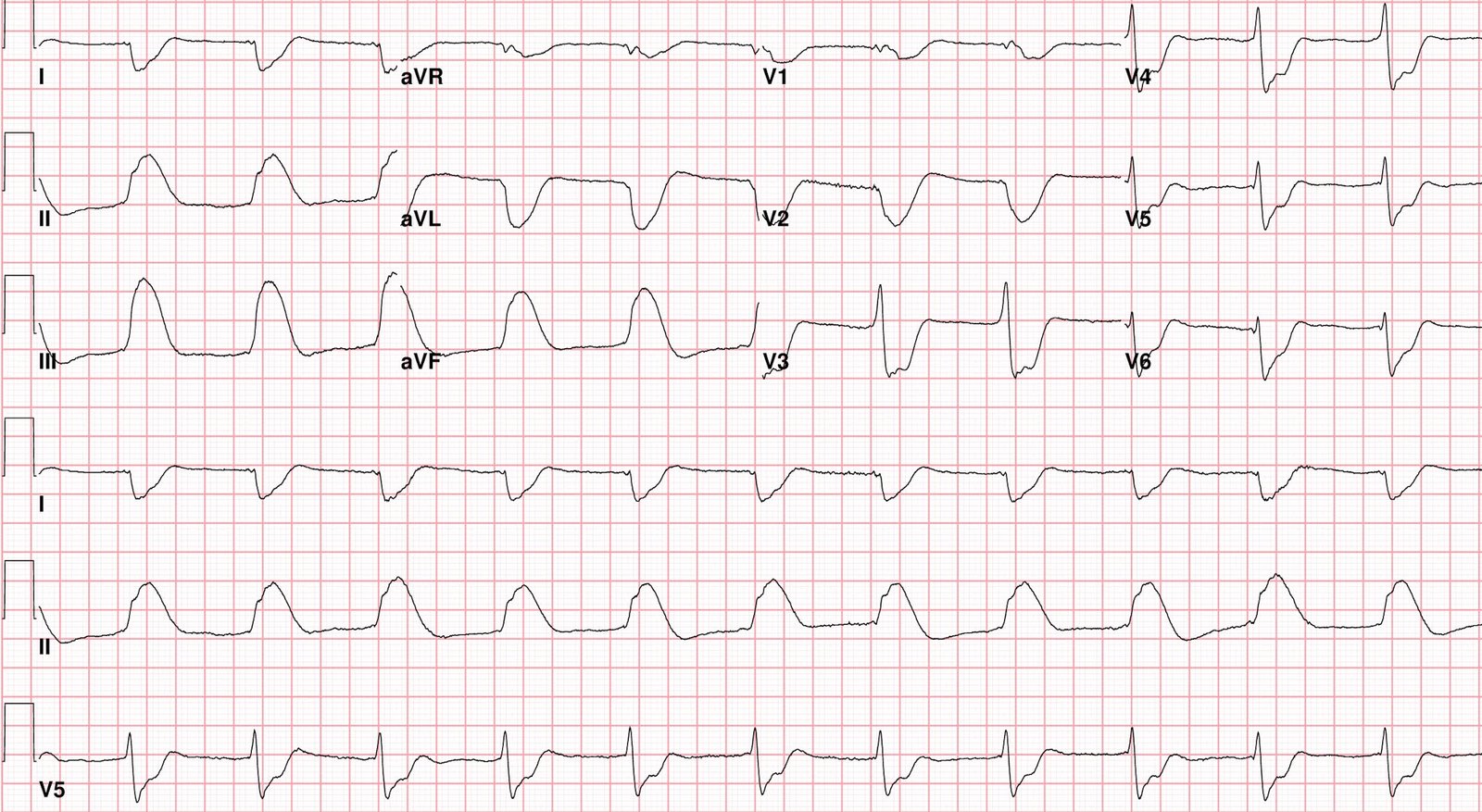
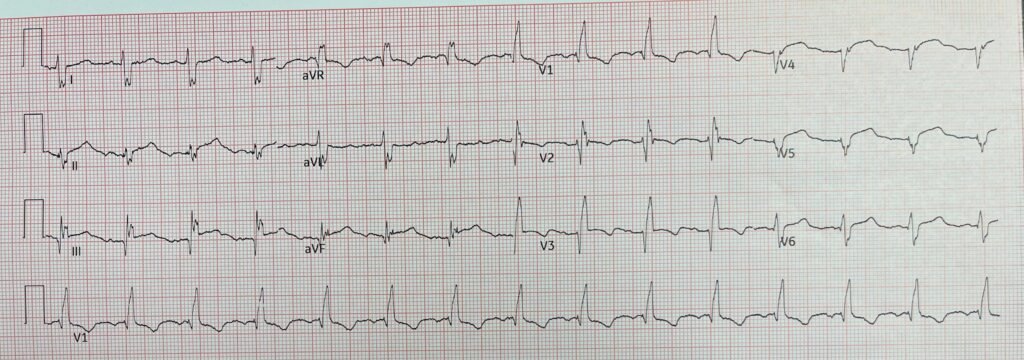
He still waited another 10 minutes for this one:
Now there is still more STE in V4. There is concordance now in V2 and V3. Clearly diagnostic of LAD OMI.
The Queen now gives a result of 1.00, the highest confidence possible.
Although the ECG now meets STEMI millimeter criteria, it is not an electrocardiographically obvious STEMI to the average emergency physician or cardiologist. The Cardiologist still did not approve of Max giving thrombolytics, but he gave them anyway.
All symptoms resolved by the time of transfer to the receiving center.
Unfortunately, he did not have time to record a post-thrombolytic ECG and does not have follow up.
Learning Points:
- It is a myth that thrombolytics are only beneficial in patients who have ST Elevation, and even more of a myth that millimeters are important. We recently re-analyzed all the data from the FTT meta-analysis, and unlike that analysis we excluded the 9000 patients from ISIS-3 whose final diagnosis was unknown. For patients who were known to have MI, the relative mortality risk was 0.799 for those who received thrombolytics vs. those who did not.
de Alencar JN, de Jesus Oliveira MH, Bulhoes E, et al. Thrombolysis in non-ST-elevation myocardial infarction: systematic review and meta-analysis of randomised controlled trials. 2025;12(2). Available from: https://openheart.bmj.com/content/12/2/e003700
- 1/3 of patients who are diagnosed with MI (both STEMI and NSTEMI) do not have chest pain. Reference and abstract below.
- Many more never even present with their acute MI because it is totally silent, and not discovered until a later visit with an incidental ECG or imaging study. (“Silent MI”)
- When uncertain, FREQUENT serial ECGs are critical.
- Even when the ST Elevation meets millimeter criteria, the ECG can be subtle.
- Do not trust your cardiologist consultant when it comes to diagnosing OMI on the ECG. You are the expert, along with the Queen of Hearts.
____________
Absence of Chest pain in acute MI
Canto JG, Shlipak MG, Roger WJ. Prevalence, clinical characteristics, and mortality among patients with myocardial infarction presenting without chest pain. JAMA 2000;283(24):3223–9.
Abstract
Context Although chest pain is widely considered a key symptom in the diagnosis of myocardial infarction (MI), not all patients with MI present with chest pain. The extent to which this phenomenon occurs is largely unknown.
Objectives To determine the frequency with which patients with MI present without chest pain and to examine their subsequent management and outcome.
Design Prospective observational study.
Setting and Patients A total of 434,877 patients with confirmed MI enrolled June 1994 to March 1998 in the National Registry of Myocardial Infarction 2, which includes 1674 hospitals in the United States.
Main Outcome Measures Prevalence of presentation without chest pain; clinical characteristics, treatment, and mortality among MI patients without chest pain vs those with chest pain.
Results Of all patients diagnosed as having MI, 142,445 (33%) did not have chest pain on presentation to the hospital. This group of MI patients was, on average, 7 years older than those with chest pain (74.2 vs 66.9 years), with a higher proportion of women (49.0% vs 38.0%) and patients with diabetes mellitus (32.6% vs 25.4%) or prior heart failure (26.4% vs 12.3%). Also, MI patients without chest pain had a longer delay before hospital presentation (mean, 7.9 vs 5.3 hours), were less likely to be diagnosed as having confirmed MI at the time of admission (22.2% vs 50.3%), and were less likely to receive thrombolysis or primary angioplasty (25.3% vs 74.0%), aspirin (60.4% vs 84.5%), β-blockers (28.0% vs 48.0%), or heparin (53.4% vs 83.2%). Myocardial infarction patients without chest pain had a 23.3% in-hospital mortality rate compared with 9.3% among patients with chest pain (adjusted odds ratio for mortality, 2.21 [95% confidence interval, 2.17-2.26]).
Conclusions Our results suggest that patients without chest pain on presentation represent a large segment of the MI population and are at increased risk for delays in seeking medical attention, less aggressive treatments, and in-hospital mortality.= = =
======================================
MY Comment, by KEN GRAUER, MD (1/31/2026):
The challenge posed by today’s case lies with the atypical history and subtle ECG findings in a patient with RBBB (Right Bundle Branch Block). That said — the diagnosis of an acute OMI should be made.
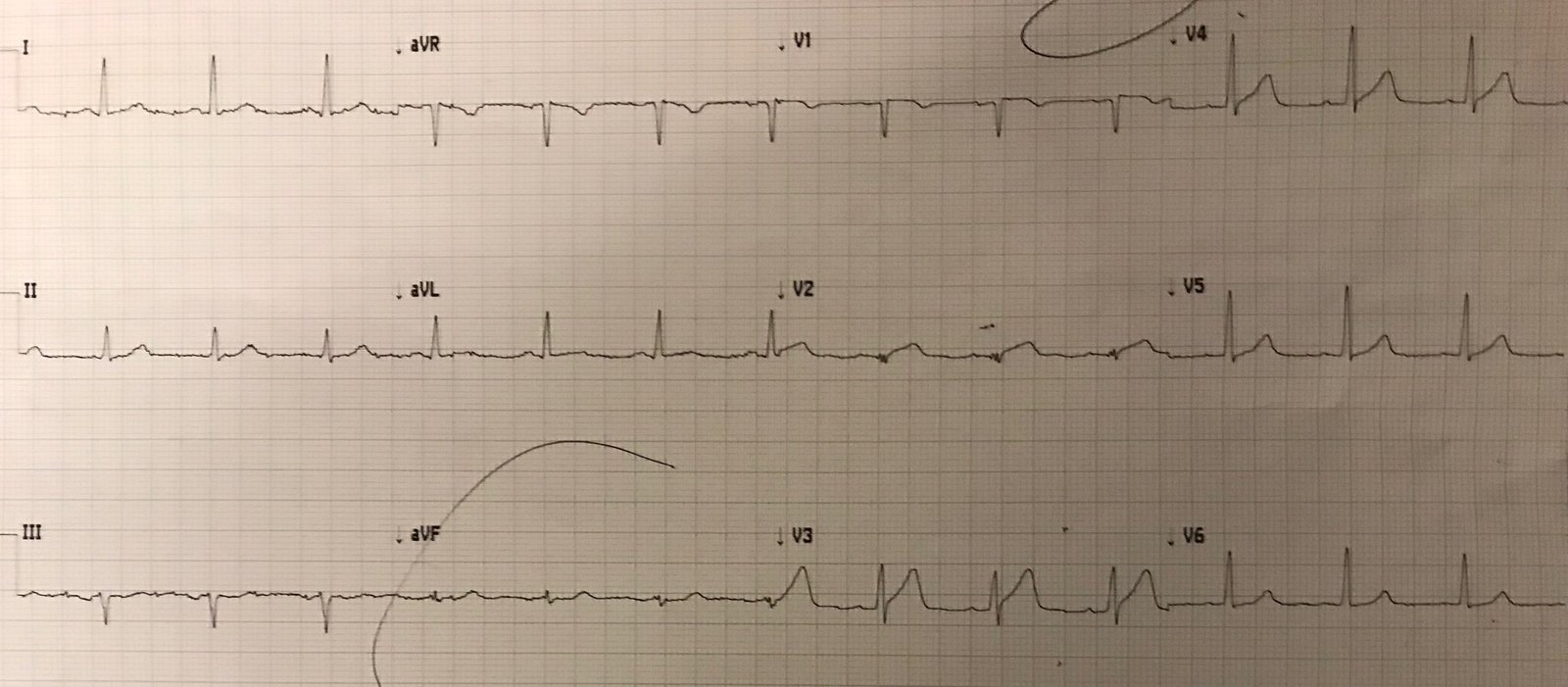
- To facilitate comparison in Figure-1 — I’ve put the 3 ECGs together.
= = =
Despite the Absence of Chest Pain . . .
Not all patients with acute OMI have acute CP (Chest Pain). Today’s patient did not. Instead — today’s patient was an older woman with a known history of diabetes and of a prior MI with stent placement. Thus, despite the absence of CP — today’s patient falls into a higher risk category. Careful scrutiny of her initial ECG is therefore essential.
- The rhythm in ECG #1 is sinus at a rate of ~80/minute.
- The QRS is wide due to complete RBBB (rSR’ in lead I — with wide terminal S waves in leads I,aVL and V6).
- In addition — there is notching (fragmentation) in each of the limb leads. (Fragmentation typically indicates “scar” — in this case ostensibly from this patient’s prior infarction).
= = =
As noted by Drs. Goder-Reiser and Smith — there is ST elevation in the inferior leads, and in leads V4-thru-V6.
- The amount of ST elevation in the inferior leads is not a lot. Nevertheless — the dotted RED lines indicate that the ST elevation in these leads is real. My “eye” was captured by the ST segment straightening (especially in leads II and aVF in Figure-1) — with the subtle-but-definite reciprocal ST depression in lead aVL confirming that an acute event has occurred (BLUE arrow).
- The amount of ST elevation in leads V4-thru-V6 is also not great. However — the lack of R wave progression in these lateral chest leads and ST segment coving in leads V4,V5 with ST segment straightening in lead V6 tell us that these findings are “real” and indicate infarction at some point in time (which is why finding a prior ECG on this patient would have been so helpful).
- PEARL: My “eye” was especially captured by the slight-but-real ST elevation in lead V2 — as well as by the baseline (instead of depressed) J-point in lead V3. Anterior leads with RBBB should manifest an ST-T wave that is oppositely directed to the terminal R’ (ie, in the form of slight ST depression). The absence of this J-point depression (YELLOW arrows) suggests that the ST elevation seen in leads V4,V5,V6 actually begins with lead V2 (and should be assumed acute until proven otherwise).
= = =
BOTTOM Line: We unfortunately do not have a prior ECG available for comparison in today’s patient. The above-described findings clearly indicate extensive infarction has occurred at some point in time. The problem given the atypical history (ie, with no CP) — was to distinguish between: i) LV aneurysm from prior extensive infarction, with residual ST elevation; — vs — ii) Prior infarction that now presents with new infarction. I was not initially sure if ECG #1 represented an acute or very recent infarction, now with residual ST elevation in multiple leads as a result of a left ventricular aneurysm — or — whether some (or most) of the above-described findings are real and “new”.
- Although I initially wavered between “old” vs “new superimposed on old” for the QRST appearance in leads V4-thru-V6 — I strongly suspected acute OMI until proven otherwise because: i) The lack of CP proves nothing (up to 1/3 of STEMIs do not have CP at the time of their initial ECG — Canto et al in JAMA 283(24):3223-3229, 2000 — Also see My Comment on “Silent MI” in the September 5, 2024 post); — ii) The inferior lead ST elevation in association with subtle-but-real reciprocal ST depression in lead aVL (BLUE arrow) looks acute; — and, iii) The subtle-but-real J-point ST elevation that occurs between lead V1 and V2 also looks acute (YELLOW arrows).
- CREDIT to Dr. Goder-Reiser, who astutely recognized these ECG features — and knew that the way to establish beyond doubt acute OMI in-progress was simply to repeat the ECG within 10 minutes.
= = =
P.S.: It’s worth spending a moment on Figure-1 to review the serial ECG changes that occurred within the space of 20 minutes.
- The progressive serial elevation of the J-point in the inferior leads seen in ECGs #2 and #3 is impressive. Note how obvious the inferior lead ST segment straightening has become by ECG #3. Now go back to ECG #1 and appreciate how this ST straightening was recognizable in its early stage on the initial ECG.
- Similarly — Note how the ST segment coving in leads V2 and V3 becomes more obvious in ECGs #2 and #3. Now go back and focus on the YELLOW arrows in ECG #1 to appreciate how this subtle clue was recognizable in its early stage on the initial ECG.
= = =
Figure-1: The 3 ECGs in today’s case.
= = =
= = =