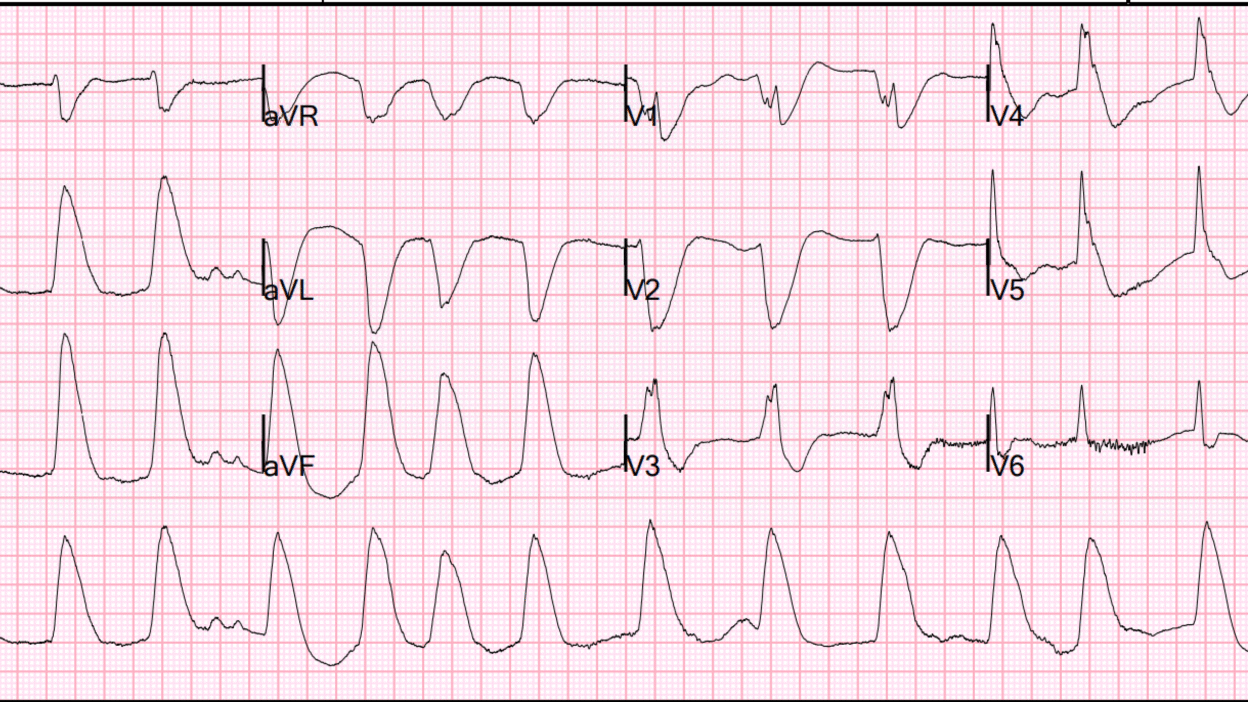
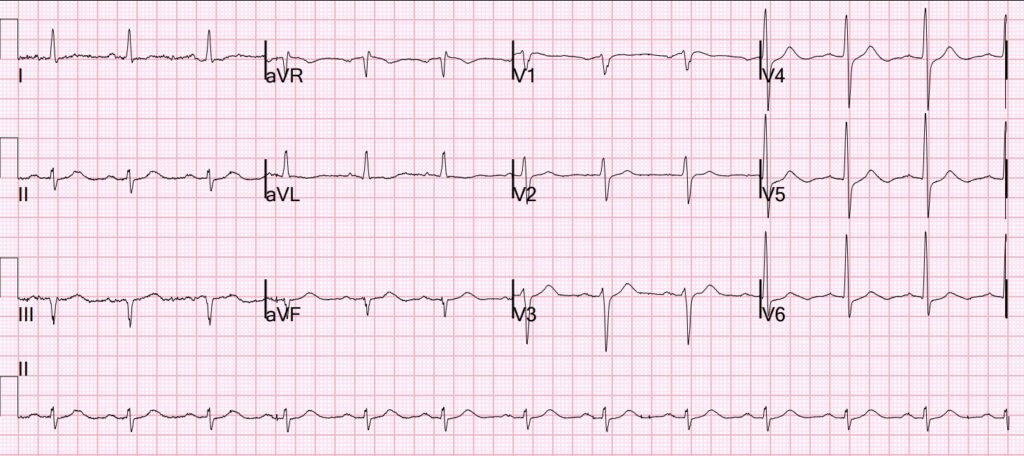
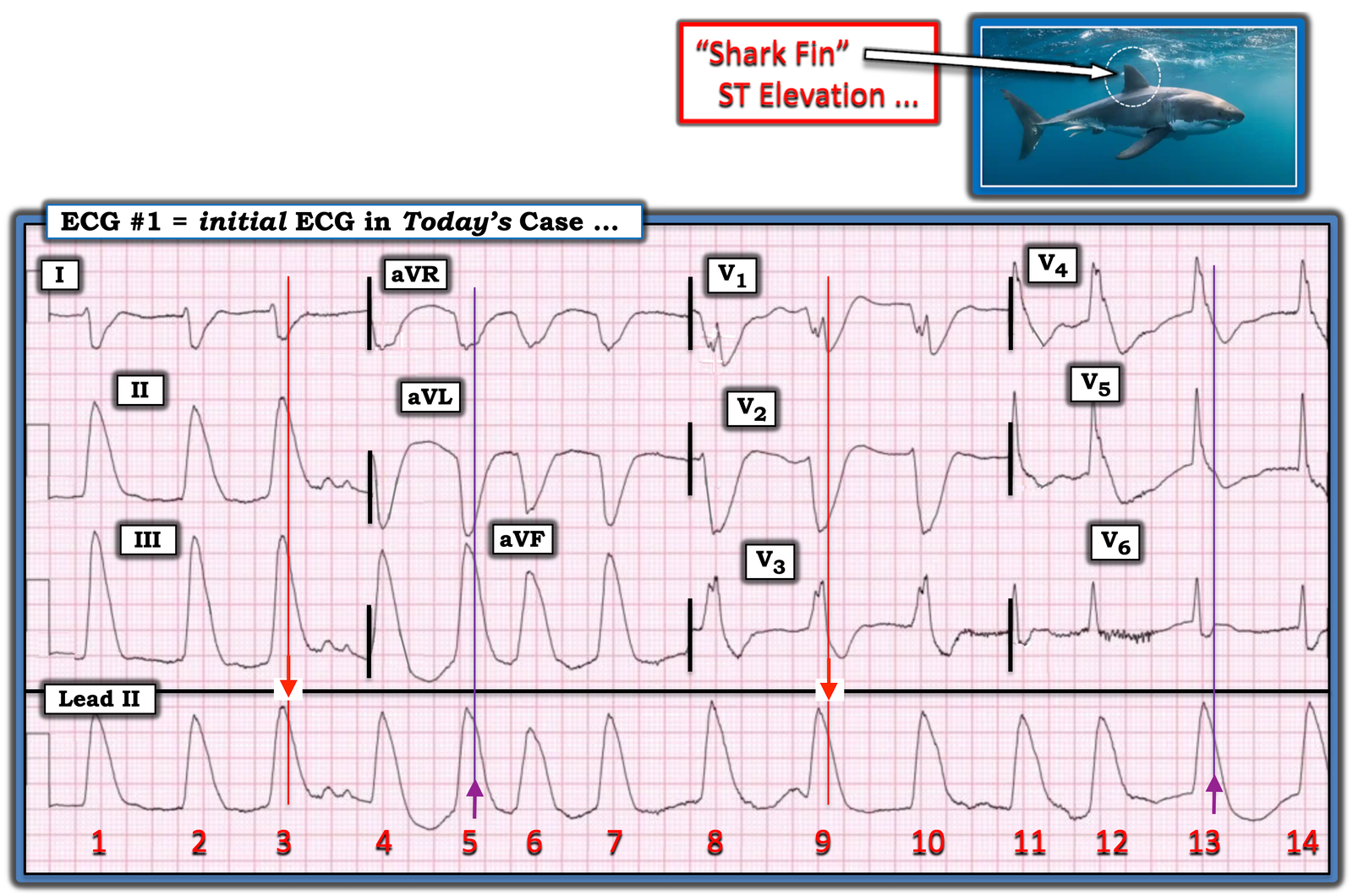
This is NOT a wide complex tachycardia. This is atrial fibrillation with “Shark Fin” pattern, an OMI pattern, and this time it is in the inferior leads, with posterior involvement shown by the inverted shark fin in V2. The end of the R-wave merges with ST Elevation, which slopes down. This has also been called “Giant R-wave”. Medics had seen this on the monitor and thought that it was ventricular tachycardia.
Shark Fin has also been called:
“Triangular QRS-ST-T waveform“
Madias JE. The “giant R waves” ECG pattern of hyperacute phase of myocardial infarction. J Electrocardiol 1993;26:77–82.
Cipriani A, D’Amico G, Brunello G, et al. The electrocardiographic “triangular QRS-ST-T waveform” pattern in patients with ST-segment elevation myocardial infarction: Incidence, pathophysiology and clinical implications. J Electrocardiol [Internet] 2018;51(1):8–14. Available from: http://dx.doi.org/10.1016/j.jelectrocard.2017.08.023
Here is the history:
This ECG was texted to me with the history that there was a bee sting.
Question: so what is the diagnosis?
My response: “Kounis syndrome”
Patient was outside when he was stung by multiple bees, witnessed by family. There was no known history of bee allergy. The patient then fell and struck head on porch railing followed by seizure activity.
EMS found patient with eyes open and moaning without signs of anaphylaxis, but then became unresponsive and went into cardiac arrest. ACLS was initiated, he was found to be in Ventricular fibrillation, then underwent defibrillation, then found to be in Ventricular tachycardia, and again underwent defibrillation along with other ACLS medications epinephrine and amiodarone.
He arrived in the ED going in and out of ventricular fibrillation.
ACLS continued, with several rounds of epinephrine given, along with several rounds of defibrillation. The patient had ROSC and loss of pulses x3, with ultimate sustained ROSC. Due to hypotension and poor LV function on bedside echo, and epinephrine infusion was initiated.
This is when the above 12-lead ECG was recorded.
Case Continued:
This ECG was sent to me only with the info that the patient had been stung by multiple bees. I responded: “Kounis syndrome”.
Until they received my response, the providers thought that they were dealing with a “wide complex rhythm” and treated with lidocaine. The QRS narrowed and they attributed that to the lidocaine,
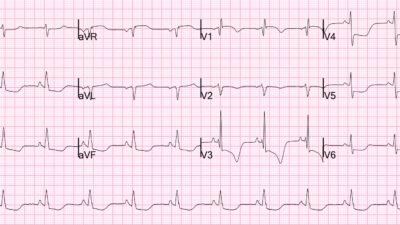
25 minutes after 1st ECG:
Shark Fin has resolved, there is now sinus rhythm (I believe there is some lead reversal because the P-wave is negative in lead II)
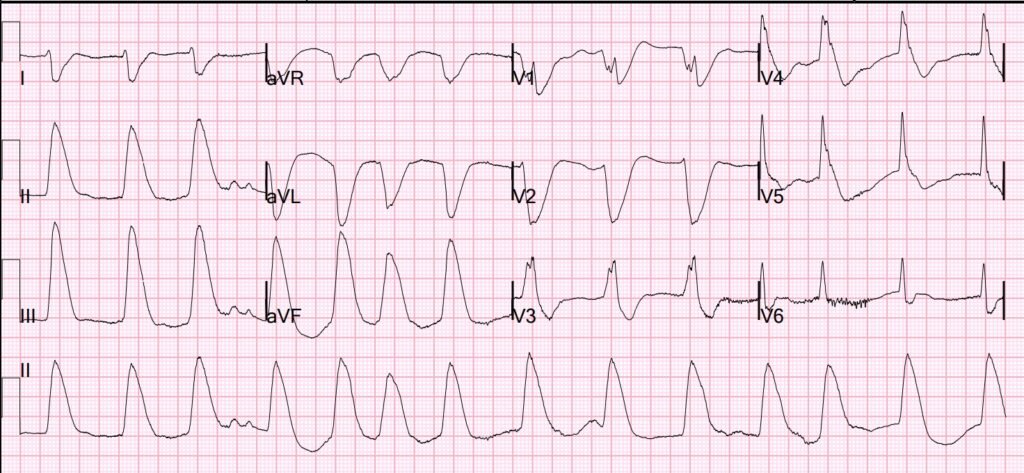
70 minutes after 1st ECG:
Sinus rhythm. Residual ischemia present
Angiogram showed spasm, but no coronary disease:
Mild Plaque no angiographically significant obstructive coronary artery
disease. Coronary artery spasm (on pressors) resolved after Intracoronary Nitroglycerine, spasm noted in proximal LAD and Mid RCA
Echocardiogram:
Normal left ventricular cavity size, wall thickness and moderately reduced
systolic function; estimated left ventricular ejection fraction 35-40%.
Moderate global hypokinesis.
Peak hs Troponin I was 23,000 ng/L
Kounis Syndrome — Coronary Occlusion syndrome due to Anaphylactic Reaction
Cahuapaza-Gutierrez NL, Calderon-Hernandez CC, Chambergo-Michilot D, De Arruda-Chaves E, Zamora A, Runzer-Colmenares FM. Clinical characteristics, management, diagnostic findings, and various etiologies of patients with Kounis syndrome. A systematic review. Int J Cardiol [Internet] 2025;418(132606):132606. Available from: http://dx.doi.org/10.1016/j.ijcard.2024.132606
Highlights
•KS presents mortality rate of 7.47 %. However, timely and adequate management reduces the risk of mortality.
•KS is an acute coronary syndrome secondary to an anaphylactic reaction, most common in males with a age of 54.4 ± 16.5 years.
•Currently, four variants of KS are proposed, with type I, allergic coronary vasospasm, is the most common.
•New cases associated with ATAK complex syndrome and COVID-19 vaccines have been reported.
•About diagnostic findings, elevated cardiac troponin I was observed in most cases, as well as an ST-segment elevation.
= = =
======================================
MY Comment, by KEN GRAUER, MD (12/4/2025):
Today’s case by Dr. Smith is strongly suggestive of Kounis Syndrome — an important entity to be aware of (See the March 1, 2023 post in Dr. Smith’s ECG Blog).
- Having been previously healthy — the 67-year old man in today’s case was gardening, when he was suddenly stung by multiple bees. This resulted in cardiac arrest requiring multiple defibrillations.
- ROSC was ultimately achieved and maintained. Cardiac catheterization revealed no significant obstructive coronary disease — with coronary artery spasm in the proximal LAD and mid-RCA that resolved with intracoronary NTG.
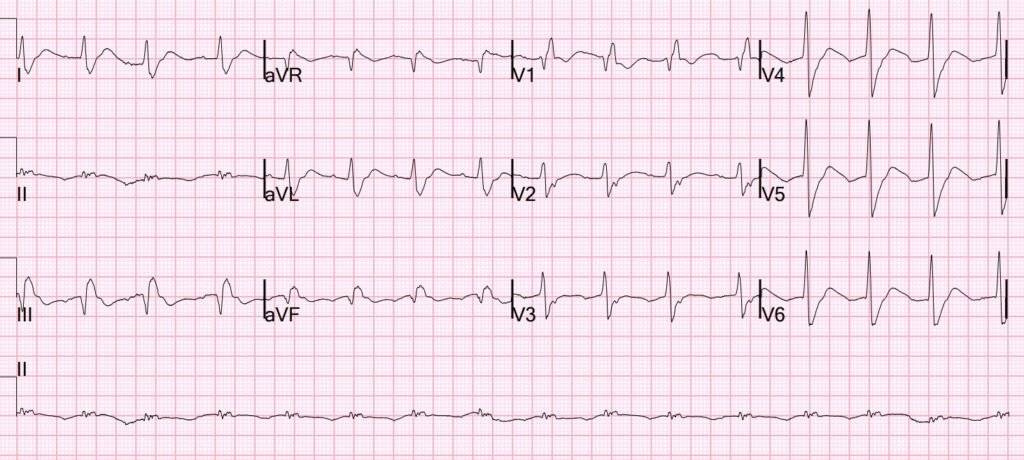
For clarity in Figure-1 — I’ve reproduced today’s initial ECG. The rhythm is irregular — P waves are absent — and the QRS appears to be wide. That said — I thought much of the QRS widening was artificially produced by marked ST-T wave deviations (ie, “Shark Fin” ST elevation and ST depression — as discussed in the June 11, 2018 post, among many additional references to this phenomenon in Dr. Smith’s ECG Blog).
- The KEY to identifying Shark Fin ST-T waves lies with identifying the end of the QRS complex — something often easier-said-than-done because of fusion between the QRS and enlarged ST-T waves.
- Although admittedly less-than-certain about my J-point landmark in Figure-1 — my best guess is represented here by the 2 vertical RED time lines that I drew in leads I,II,III; and in V1,V2,V3.
- Using the intersection of these vertical time lines with QRS complexes in the long lead II — I extended upward PURPLE time lines to define the end of the QRS in the other 6 leads.
- Bottom Line: The sudden occurrence of dramatic Shark Fin ST-T wave deviations following a severe allergic bee sting reaction — in association with the cardiac cath finding of coronary spasm (relieved by IC-NTG) — is consistent with one of the mechanisms of Kounis Syndrome.
= = =
Figure-1: I’ve reproduced and labeled today’s initial ECG.
= = =
Kounis Syndrome:
I found the manuscript by Rodríguez-Ruis et al to be an excellent review on Kounis Syndrome (Heart Views 20(3):122-125, 2019 ). The subtitle of their manuscript, “A More Commonly Encountered Cause of Acute Coronary Syndrome” highlights the importance of our awareness of this syndrome — as it may occur not only in older individuals with known coronary disease, but also de novo in younger adults with no prior history of coronary disease.
- The syndrome arises following an allergic or hypersensitivity reaction that results in mast cell activation that prompts release of any of a variety of inflammatory mediators (including histamine, serotonin, leukotriene, cytokines, prostaglandins — among others).
- Potential triggers of Kounis Syndrome are multiple — including antibiotics (among other medications) — insect stings (bees, wasps, spiders) — contrast media — foods (shellfish, certain fruits) — urticaria itself.
- A Kounis reaction may initiate acute ACS by one of 3 mechanisms: — i) Coronary spasm (as in today’s patient); — ii) Acute coronary occlusion (from damage to existing plaques from inflammatory mediators that may lead to plaque damage, rupture and acute thrombosis); — or, iii) Stent thrombosis due to damage from inflammatory mediators.
- Regarding symptoms — onset may be abrupt (as in today’s case) — or more gradual with nausea, vomiting, chest pain, shortness of breath or allergic manifestations of itching, hives, swelling.
- A KEY to treatment is to stop the allergic reaction (ie, use of IV steroids, antihistamines, oxygen, epinephrine [if/as needed] ) — as well as the usual treatments of coronary spasm or occlusion.
Additional considerations put forth in this Rodriguez-Ruis manuscript including the following:
- Active use of nitrates/calcium channel blockers if coronary spasm is the mechanism vs PCI for acute coronary thrombosis.
- Beta-blockers are best avoided if coronary spasm is suspected (ß-blockers may exacerbate spasm by the unopposed alpha-adrenergic effect of this drug).
- Awareness that epinephrine may worsen vasoconstriction in patients with coronary spasm (careful monitoring is essential).
- Morphine should be avoided because it may stimulate further histamine release (and thus exacerbate the allergic cascade of Koumis Syndrome).
- After treatment — evaluate the cause of the allergic reaction.
= = =
= = =
= = =