A 70-something with no cardiac history called 911 for acute chest pain.
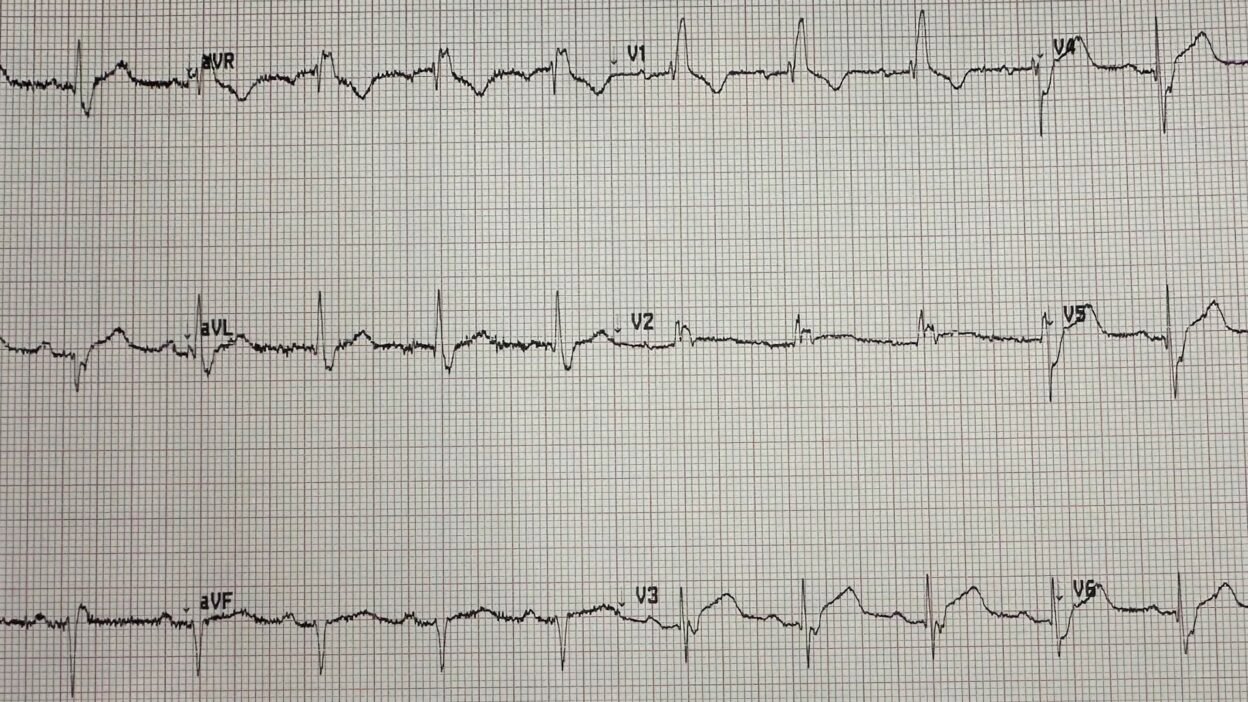
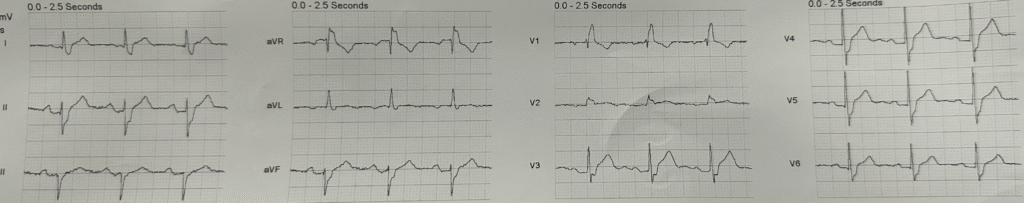
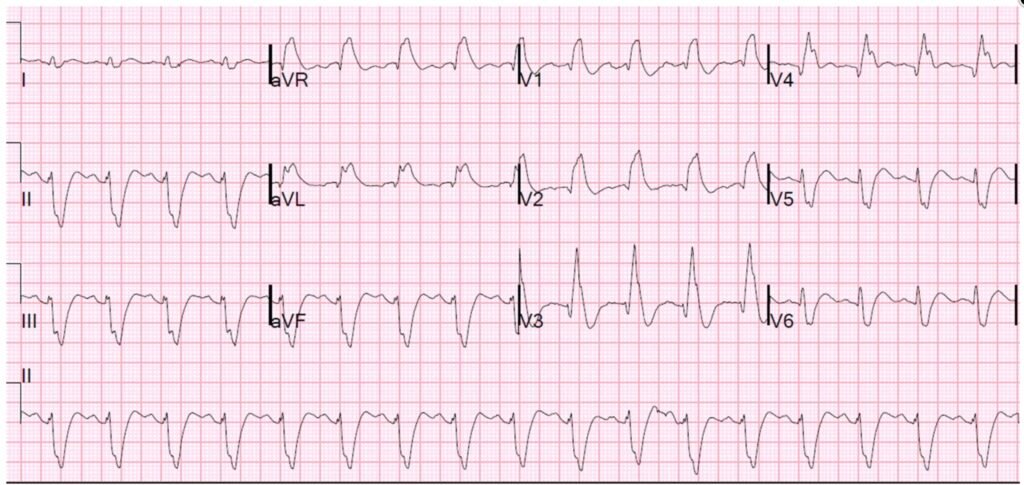
Here is the prehospital ECG:
What do you think?
There is right bundle branch block (RBBB) and left anterior fascicular block. There are 2mm of ST Elevation in V3 and V4. There is more than 1 mm STE in V5 and STE = 1 mm in V6. RBBB is “supposed to” have no ST Elevation anywhere. Usually, in V1-V3, there is ST depression discordant to a positive R’-wave. In this case, V3 does not have a positive R’-wave. Instead, there is a negative S-wave, and so one might expect discordant STE. The same goes for V4-6. However, V4-6 in RBBB usually have a wide S-wave but are not “supposed to” have any ST Elevation. The combination of RBBB and LAFB in the setting of suspected LAD Occlusion (OMI) is a particarly bad combination. When I have seen it, it is usually post-arrest, pre-arrest, or in the setting of acute cardiogenic shock. It is really terrible (see examples below).
In addition, the T-waves are suggestive of Hyperacute T-waves in V3-4.
The cath lab was activated prehospital for ST Elevation.
I was not the attending, but I showed up and looked at this prehospital ECG. I thought it was probably a “fake” (a STEMI mimic, or OMI mimic). It just did not look like OMI to me.
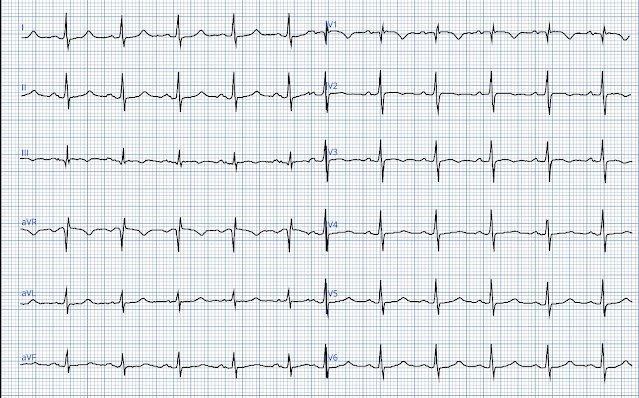
We recorded an ED ECG:
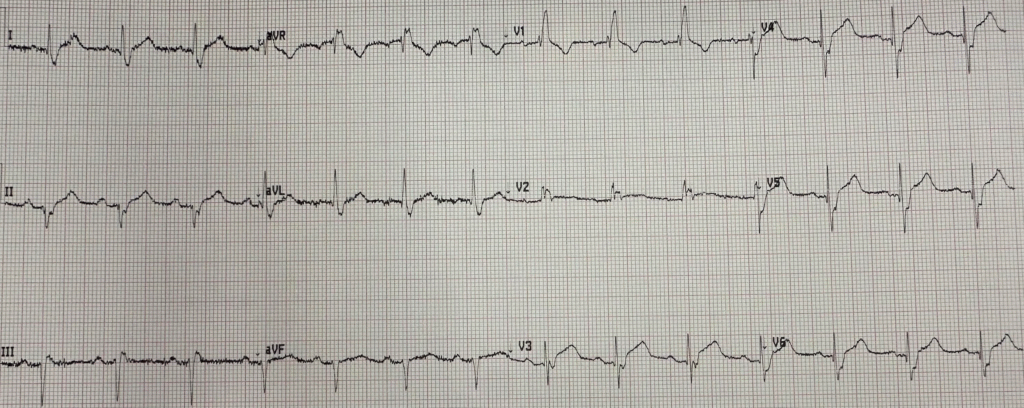
It looks the same.
I still thought it looked like a mimic.
So I put it through the PMCardio Queen of Hearts AI app:
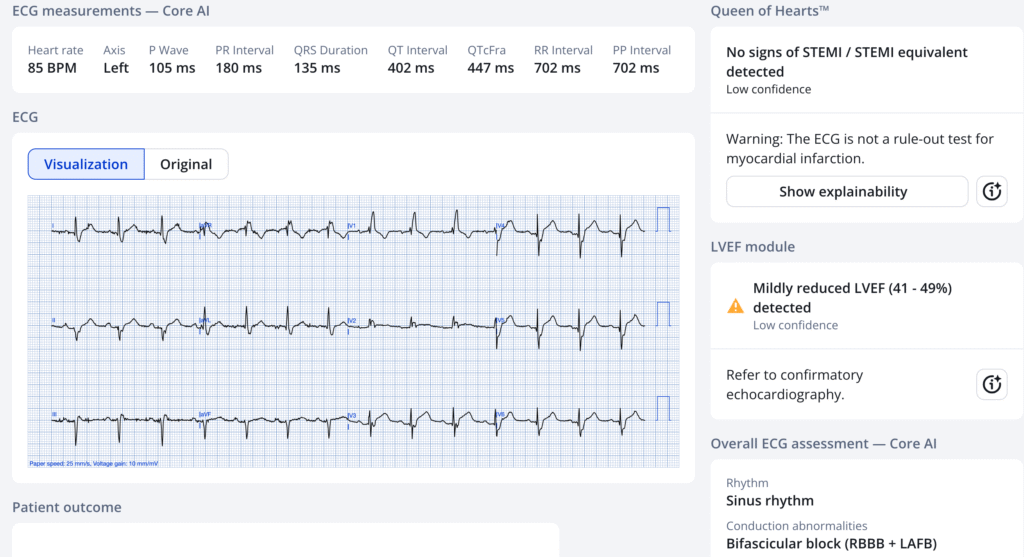
She also thinks there is no “STEMI or Equivalent”
There was no previous ECG for comparison.
I did not think the ECG was specific for OMI, and neither did the Queen of Hearts, but both of us had low confidence, and there was no previous ECG for comparison. But the pretest probability was high and the consequences of missing an LAD OMI in the presence of RBBB and LAFB was too terrible to rely on, and so we activated the cath lab.
Angiogram was negative and all trops were undetectable.
We have data that is submitted for publication showing a decrease in false positive ECGs from 45% to 10% with use of the Queen of Hearts.
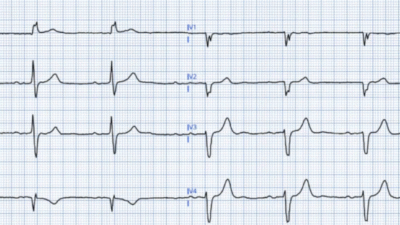
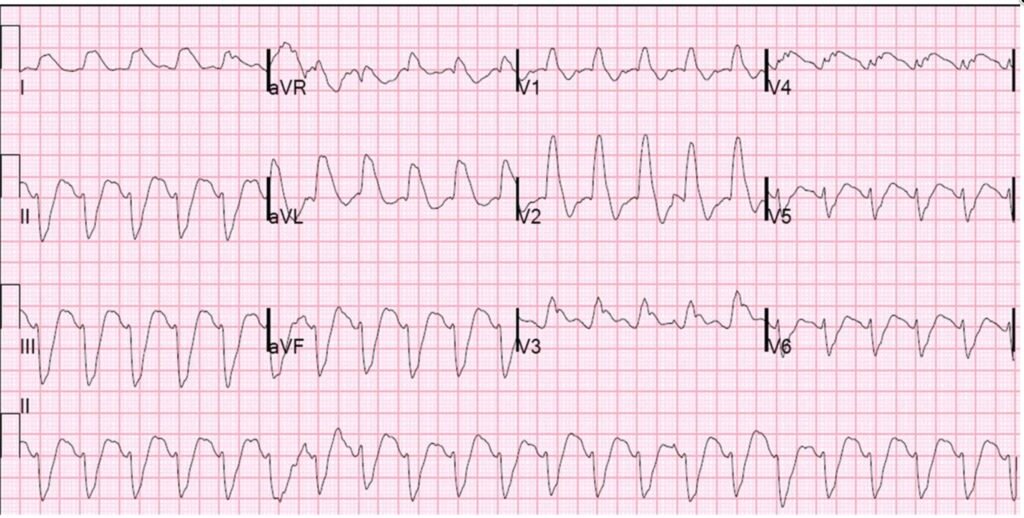
A few examples of RBBB/LAFB with LAD or Left Main OMI.
And here are two of them (Both accurately diagnosed as OMI by PMCardio Queen of Hearts)
Wide Complex Tachycardia; It’s really sinus, RBBB + LAFB, and massive ST elevation
======================================
MY Comment, by KEN GRAUER, MD (7/26/2025):
Assessment of an ECG for acute ischemia in association with a conduction defect (ie, LBBB, RBBB) is often challenging. That said — much of the time, such assessment can be made in time-efficient fashion with attention to a number of specific features. Today’s case illustrates the application of some of these features.
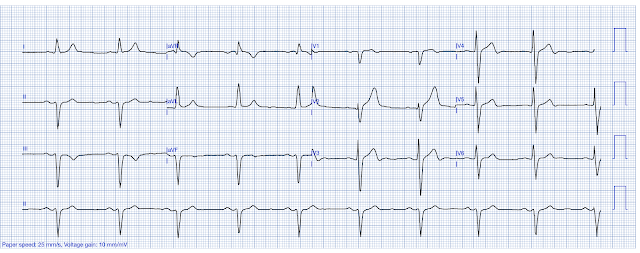
- For clarity in Figure-1 — I’ve reproduced and have labeled the initial ECG in today’s case.
= = = = = = = = = = = = = = = = = = = =
Today’s Initial ECG:
As per Dr. Smith — today’s patient is a 70-something year old woman with new CP (Chest Pain), whose initial ECG is shown in Figure-1.
- That the rhythm is sinus — is confirmed by the presence of upright P waves with a constant and normal PR interval in lead II.
- The QRS complex is wide with bifascicular block (RBBB established by the rsR’ in lead V1 — and LAHB established by the predominantly negative QRS complex in the inferior leads).
- KEY Point: As emphasized in My Comment at the bottom of the page in the April 13, 2020 post, among others — the ST-T wave in lead V1 with RBBB should be oppositely directed to the last QRS deflection. This is seen in Figure-1 (ie, the last QRS deflection is the large upright R’ — with the ST-T wave in lead V1 appropriately negative).
- But in addition — a similarly oppositely directed ST-T wave should also be seen at least in lead V2, if not also in V3. But instead of ST-T wave depression in lead V2 — there is subtle-but-real ST segment coving and elevation (within the RED rectangle in Figure-1).
- The RED arrow in neighboring lead V3 highlights ST segment straightening and J-point ST elevation that should not be there!
- In this context — the ST segment straightening with J-point ST elevation seen in 5 other leads (BLUE arrows in Figure-1) potentially represents an extension of what appears to be hyperacute changes in leads V2 and V3.
- As per Dr. Smith — the finding of RBBB/LAHB in association with the above described findings in this older patient with new CP — should suggest the possibility of acute LAD OMI until proven otherwise ==> justification to activate the cath lab!
Figure-1: I’ve reproduced and labeled today’s initial ECG (To improve visualization — I’ve digitized the original ECG using PMcardio).
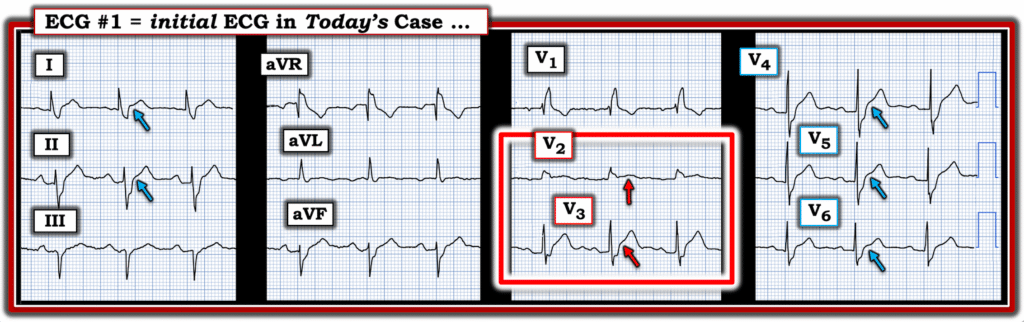
P.S.: As noted above by Dr. Smith — the cath report was negative. That said — the bifascicular block is real. Access to a prior ECG might have avoided the need for cardiac cath — but prior tracings are not always readily available at the time they are needed in the acute situation.
- BOTTOM Line: The above noted ST-T wave findings in 7/12 leads are suspicious enough to justify prompt cath. As per Dr. Smith — Better prompt cath then to risk overlooking potentially lethal LAD OMI.
==============================