Written by Jesse McLaren
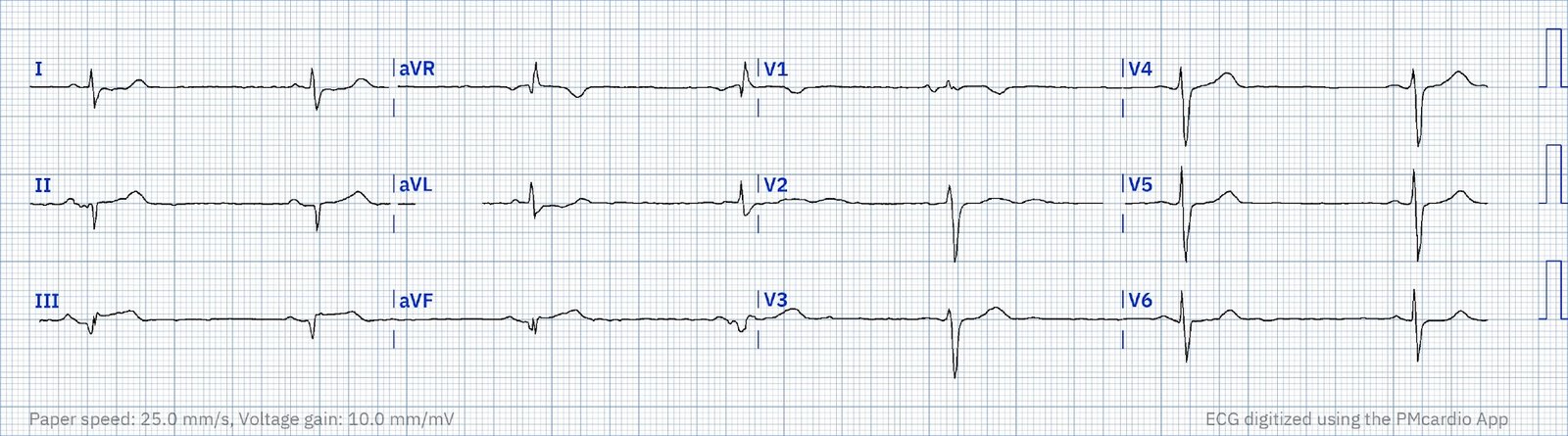
A 75 year old
with a history of CABG called EMS after 24 hours of chest pain. HR 40, BP
135/70, RR16, O2 100%. Here’s the paramedic ECG (digitized by PMcardio). What
do you think?
There’s sinus
bradycardia, normal conduction, normal axis, delayed R wave progression, and
normal voltages. There are inferior Q waves and lead III has mild concave ST
elevation, with subtle reciprocal ST depression in I/aVL. This is diagnostic of
inferior OMI, likely from the RCA. The patient has a history of CABG so some of
these changes could be old, but with ongoing chest pain and bradycardia in a
high risk patient this is still acute OMI until proven otherwise.
I sent the ECG
to Dr. Meyers without any information, and he immediately replied, “inferior
OMI.” I also sent this to the PMcardio app Queen of Hearts. Trained by Smith
and Meyers, it delivered the same immediate reply of OMI with high confidence:
But there are
multiple barriers to getting the patient to the cath lab:
a. STEMI negative: the EMS automated
interpretation read, “STEMI negative. Inferior infarct, age undetermined. Sinus
bradycardia.” According to the STEMI paradigm, the patient doesn’t have an
acute coronary occlusion and doesn’t need emergent reperfusion, so the
paramedics can bring them to the ED for assessment, without involving
cardiologists. But the latest ACC consensus on the evaluation of chest pain in
the ED warns that “STEMI criteria will miss a significant minority of patients
with acute coronary occlusion.”[1]
b. late presentation: even if there were
STEMI criteria, the patient presented with 24 hours of chest pain, and with Q
waves – both of which are often (wrongly) considered outside the window for
treatment. In a study evaluating the reasons why STEMI patients do not receive
reperfusion, patient delay greater than 12 hours from symptom onset was the
most common reason.[2] This despite evidence of myocardial salvage in late
presenters (12-72h) with total occlusion.[3]
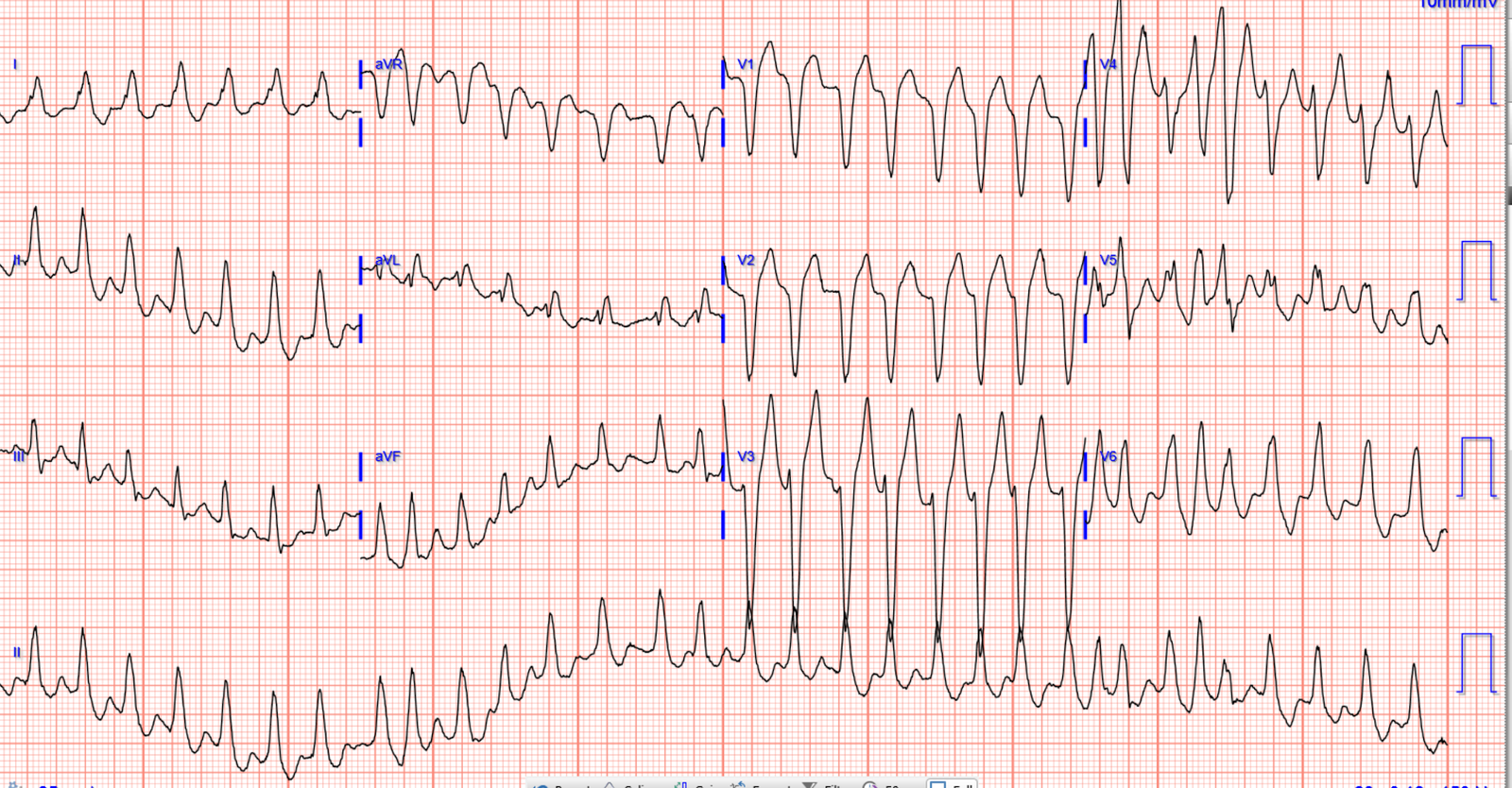
b. transient ST elevation but ongoing
occlusion. Even if the patient had presented acutely with STEMI criteria,
the ST elevation resolved on arrival though the pain continued. Here’s the
first and repeat paramedic ECG:
According to some
interpretations of the literature on “transient STEMI”, this patient doesn’t
need the cath lab because ST segments improved. For example, the TRANSIENT trial randomized patients with transient STEMI to immediate vs delayed invasive strategy and concluded that “infarct size in transient STEMI is small and is not influenced by an
immediate or delayed invasive strategy. In addition, short-term MACE was
low and not different between the treatment groups.”[4] But the inclusion criteria was that patients “must have complete relief of symptoms and complete normalization of ST-segments.” And even then there was a risk of reocclusion with cath lab delay.
As an analysis of the TRANSIENT trial explained, “there are concerning signals in this
under-powered trial. There were trends toward larger infarct size with
delayed angiography, both by cMR and integral high-sensitivity troponin
concentration, as well as toward higher rate of major adverse
cardiovascular events (MACE) (8.5 vs. 2.9%; P = 0.28) in the
delayed group. This latter figure includes the four patients randomized
to delayed angiography who underwent urgent revascularization for
recurrent ischaemia, and mirrors a trend observed in the ELISA-3 post hoc
analysis of transient STEMI patients. As recurrent ischaemia is the
principle event reduced by early intervention in NSTE-ACS, these are
important endpoint events occurring with delayed angiography and there
is a consistent signal for harm now from two data sources.”[5]
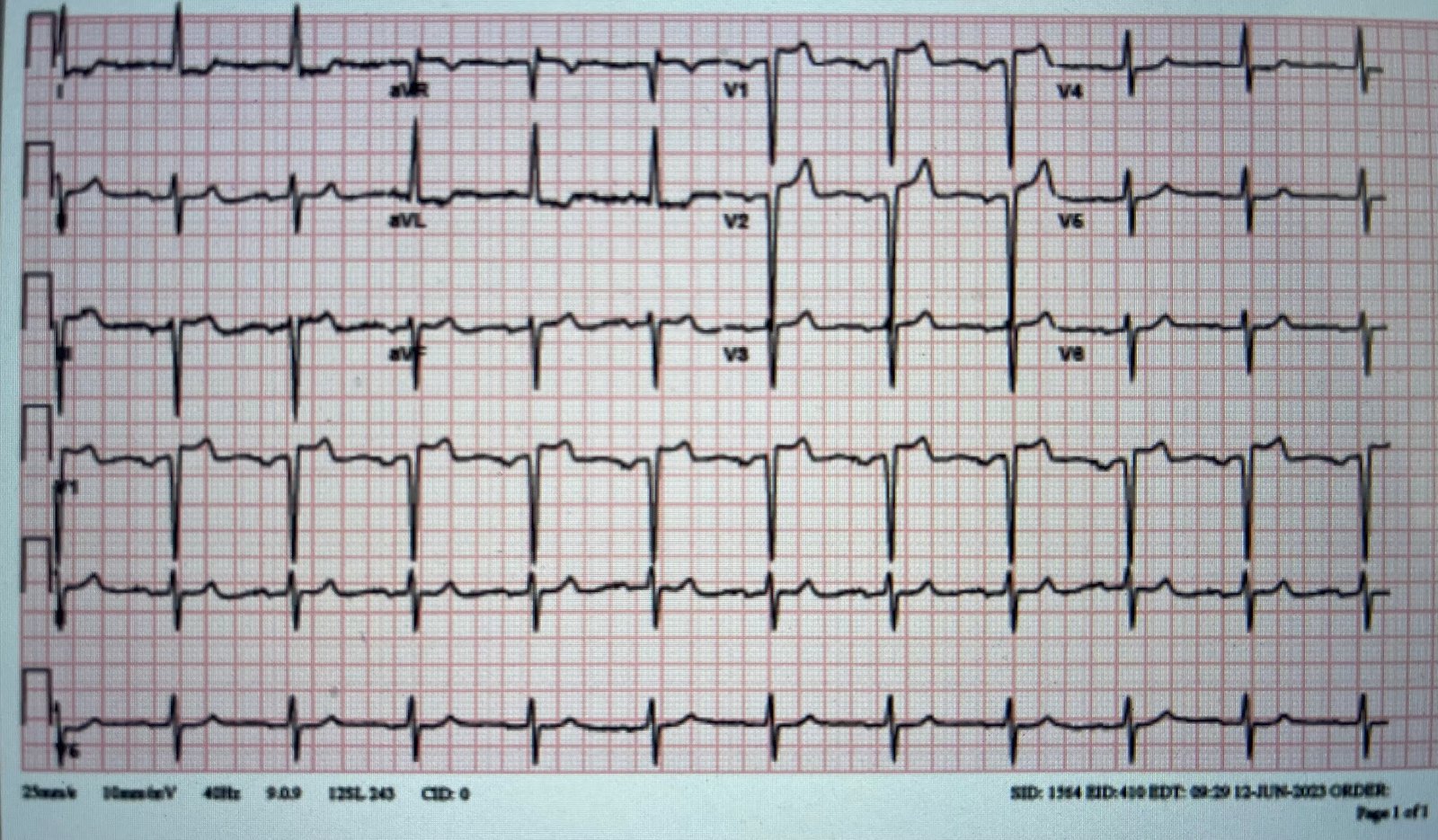
This patient had ongoing chest pain, bradycardia, and no signs of reperfusion T
wave inversion. Repeat ECG in the ED showed a hint of inferior ST elevation:
STEMI vs OMI paradigms
Following the
STEMI paradigm, the most likely evolution of this case would be:
1.
paramedic
transportation to the ED as “chest pain, STEMI negative”
2.
ED
consult for “non-STEMI” when the trop comes back elevated
3.
Cardiology
admit as “non-STEMI” for non-urgent angiogram
4.
Discharged
diagnosis of “Non-STEMI”, regardless of angiographic findings, peak troponin or
echo
But instead,
this patient received excellent care by disregarding the STEMI paradigm and
focusing on the reperfusion of acute coronary occlusion:
1.
Despite
no STEMI criteria, the paramedics advocated for a stat cardiology consult out of
concerns for an acute coronary occlusion—because of high pretest probability
and subtle ECG signs of occlusion. As they documented, “Paramedics noted
patient’s 12 Lead appeared to have 1mm of elevation in III and borderline 1mm
elevation in aVF, with mild depression in I and aVL. Due to these borderline
findings and patient’s cardiac history, cardiac interventionalist was called
for consult.”
2.
Cardiology
documented “late presentation STEMI but likely aborted given resolution
of ST changes from EMS to hospital.” But they still took the patient
immediately to the cath lab, with a door-to-cath time of 45 minutes.
The patient had a 100% occlusion of the RCA graft. Initial
troponin I was 4,000 ng/L (normal <26 in males and <16 in females) and
rose to 14,000 (confirming it was not a ‘missed STEMI’ with peak troponin on
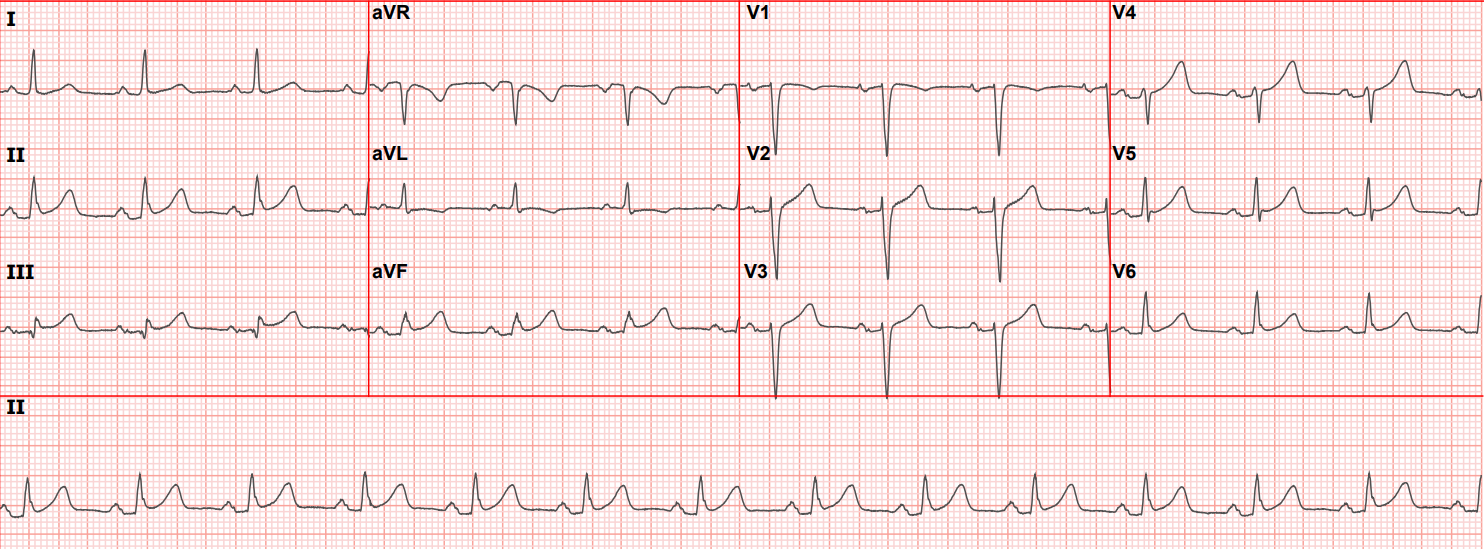
presentation, despite the 24 hours of pain). Follow up ECGs showed inferior
reperfusion T wave inversion:
The only problem
is that the discharge diagnosis was “STEMI” even though no ECG ever met STEMI
criteria. So this rapidly treated STEMI(-)OMI will be included in the STEMI
database showing the benefits of rapid reperfusion for “STEMI”, rather than being
recognized as one of many “non-STEMI” with occlusion that are at risk for delayed
reperfusion but that would do better with rapid reperfusion.
Take home
1.
STEMI
criteria, and automated interpretations based on it, will miss acute coronary
occlusion. But emergency providers including paramedics can learn signs of OMI,
which can be accelerated by expert-trained AI
2.
Prolonged
symptoms doesn’t mean completed infarct, and is not a reason to withhold
reperfusion
3.
Transient
ST elevation with ongoing symptoms still needs the cath lab
4.
The
OMI paradigm shift can begin locally, but databases should accurately classify
patients as OMI/NOMI rather than STEMI/Non-STEMI – both to identify preventable
delays to reperfusion, and to highlight successes like this case
References
1.
Kontos
et al. 2022 ACC Expert Consensus Decision Pathway on the Evaluation
and Disposition of Acute Chest Pain in the Emergency Department: A Report of
the American College of Cardiology Solution Set Oversight Committee. J Am Coll
Cardiol 2022 Nov 15;80(20):1925-1960
2.
Welsh
et al. Evaluating clinical reasons and rationale for not delivering reperfusion
therapy in ST elevation myocardial infarction patients: insights from a
comprehensive cohort. Int J Cardiol 2016
3.
Busk
et al. Infarct size and myocardial salvage after primary angioplasty in
patients presenting with symptoms for <12h vs 12-72h. Eur Heart J 2009
4 Lemkes et al. Timing of revascularization in patients with transient ST-segment elevation myocardial infarction: a randomized clinical trial. Eur Heart J 2019
5.
Bergmark BA, Faxxon DP. Transient
ST-segment myocardial infarction: a new category of high risk acute coronary
syndrome? Eur Heart J 2019;40:292-294