I have posted on this topic before, but whenever I think that readers completely understand it, I find there are still many who do not. So I think it is worth the repetition. Becoming facile at reading ECGs is a matter of repetition and practice.
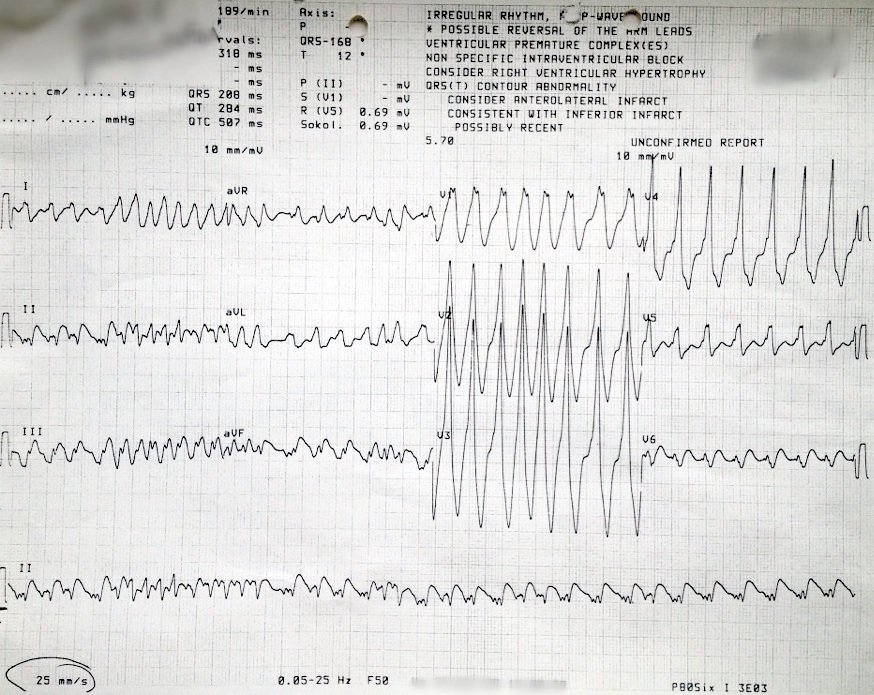
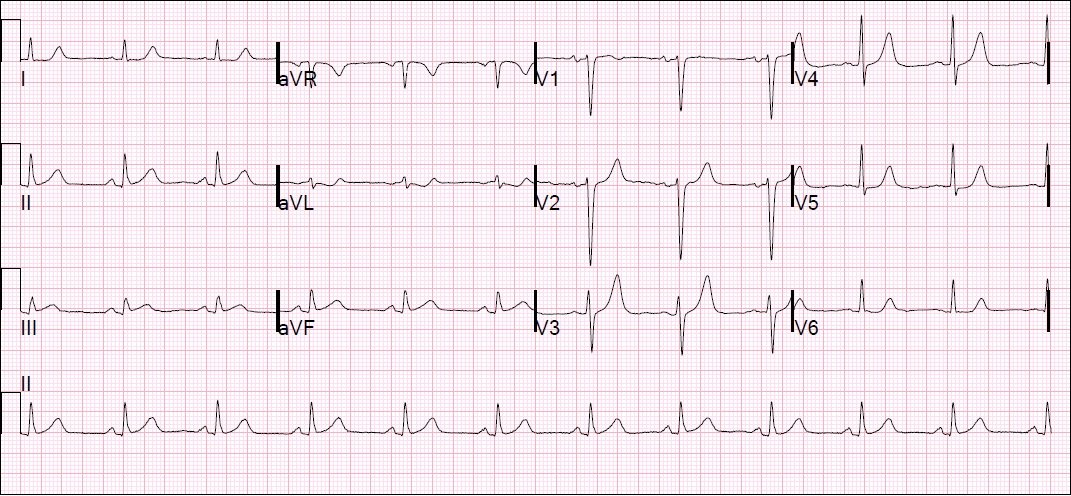
A 20-something calls 911 for palpitations and dizziness, arrives in the ED and has this ECG recorded. What are you going to do?
Below I have put arrows on the R-R interval that is shortest.
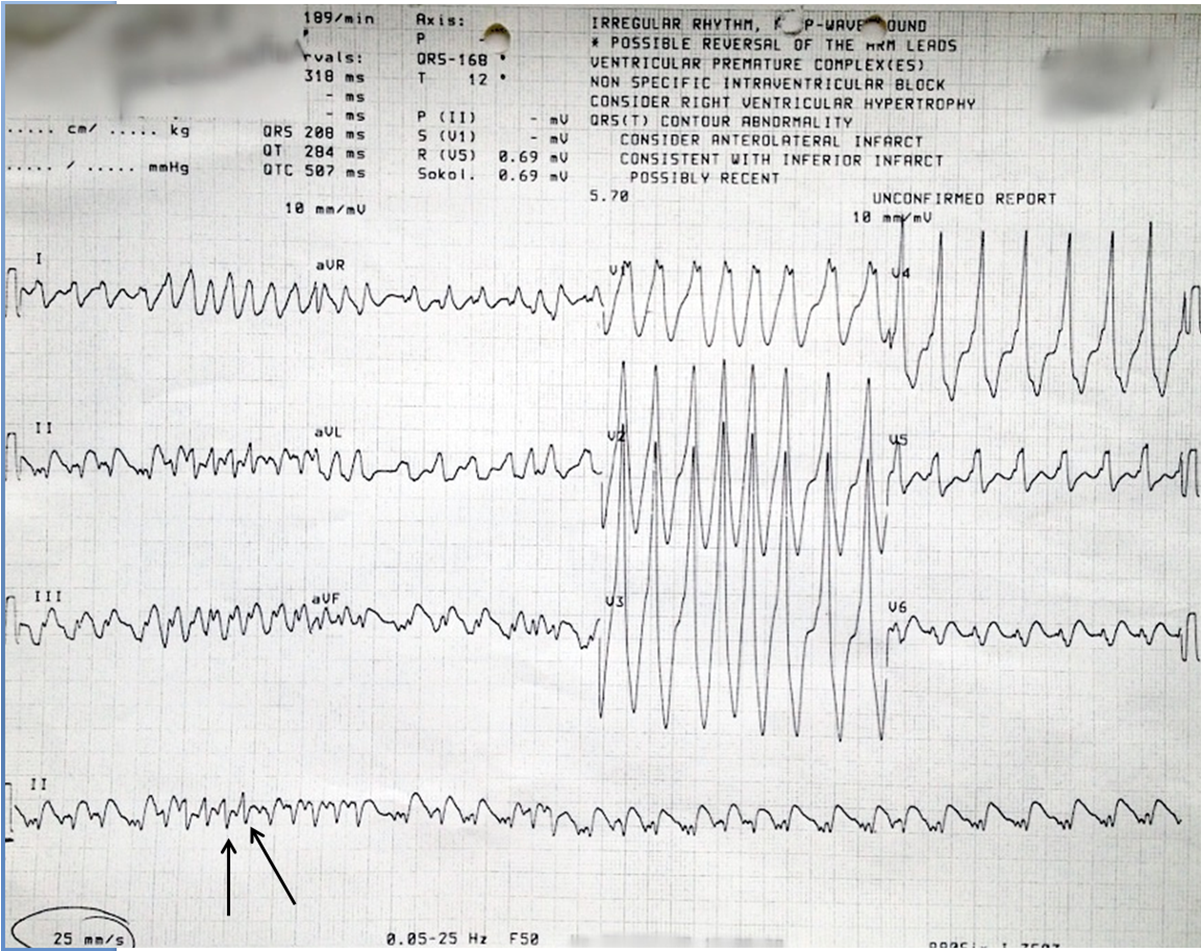 |
| This very short R-R interval is approximately 160 ms! |
1. What are you going to do?
2. (Less important) What is the diagnosis?
3. What are you definitely not going to do?
Answers
1. Cardiovert. Cardioversion will treat it effectively, whatever the etiology. This is so fast that it needs rather urgent therapy. Any medication could be ineffective or, worse, dangerous. (It may be reasonable, but much less preferable, to treat with procainamide or another Type 1 antiarrhythmic if for some reason cardioversion cannot be done).
2. The rate is fast and the rhythm is irregularly irregular, so this is Atrial fibrillation. With the very fast ventricular response and the bizarre, polymorphic QRS, it is nearly pathognomonic for atrial fibrillation in the setting of WPW. The impulses conduct variably and very fast down the accessory pathway because it has a very short refractory period. Whenever the shortest R-R interval is less than 240 ms, there is a high risk of degeneration into ventricular tachycardia or fibrillation, especially if AV nodal blockers are given. In fact, the morphologies during this 1.6 seconds of extremely fast rate
are so different that they may, in fact, be a short run of polymorphic
ventricular tachycardia, though this is impossible to know.
3. You are not going to give any AV nodal blockers (no Digoxin, Adenosine, Calcium Channel Blocker, or even Beta Blocker)
Finally, this prohibition against AV nodal blockers only applies to Atrial Fibrillation with WPW. It does not apply to:
1. WPW with a regular tachycardia, even if wide (Patients with AV reciprocating tachycardia (antidromic reciprocating tachycardia) respond to AV nodal blockers. They are not dangerous and are very helpful
2. Atrial fibrillation with a monomorphic wide complex, and no very short R-R intervals, is not WPW. It is atrial fibrillation with aberrancy, usually RBBB or LBBB, and these may be safely slowed with AV nodal blockers such as Diltiazem or a Beta Blocker.
I do not have followup on this case.
For more on this topic and more interesting cases, see this post, and this post.