Written by Magnus Nossen
Today’s patient is an 80-year-old man with stage 5 chronic kidney disease (CKD), but not yet receiving dialysis. His medical history includes hypertension and a prior myocardial infarction, for which he underwent PCI with stenting of a marginal branch of the LCx. He called emergency medical services after developing sudden onset chest pain, rated as 8 out of 10, accompanied by shortness of breath. The following prehospital ECG was obtained 25 minutes after symptom onset.
What do you think about the ECG and the clinical situation — and how would you manage this patient?
Prehospital ECG (ECG #1)

Originally recorded with a paper speed of 50mm/s. The above image has been compressed on the X-axis to look like it was recorded at 25mm/s. Standard lead layout.
Interpretation
The rhythm in ECG #1 is sinus with a heart rate of 67 bpm. The QRS is wide at about 160ms and consistent with LBBB. There is maximal (discordant) ST-elevation in lead V2, which measures 4 mm with a preceeding S wave of 11 mm. There are no concordant ST segments.

A presumed new LBBB does not predict acute coronary occlusion (1) and routine CAG is no longer done for this patient group. The initial ECG in today’s case also does not meet any of the original Sgarbossa criteria developed to detect acute MI in the setting of LBBB. According to the original scoring system, which is weighted (some features have more importance than others), a total of 3 or more points is required for a positive result. Isolated excessive ST elevation in the precordial leads would only score 2 points, which falls short of the threshold. This limitation explains the poor sensitivity of the original criteria, resulting in many missed LAD occlusion myocardial infarctions (OMIs). Even if the ST elevation in lead V2 had exceeded 5 mm, this ECG would still be classified as Sgarbossa negative under the original criteria.
Even if we use an Unweighted Original Sgarbossa Criteria, none of the 3 criteria are met.
The ECG however is diagnostic of acute LAD occlusion in the setting of LBBB. There are prominent hyperacute T-waves in the precordial leads. These findings are appreciable even in the presence of left bundle branch block. Furthermore, several ST segments are proportionally excessively discordant. Applying the Smith-modified Sgarbossa criteria, the S wave in lead V2 measures 11 mm — and the ST-segment elevation in V2 is 4 mm, resulting in an ST/S ratio of 0.36. This exceeds the diagnostic threshold (≥0.25), making it both highly specific and sensitive for identifying occlusion myocardial infarction (OMI) in patients with LBBB.
Smith: Meeting or exceeding the threshold in just one lead is sufficient. Moreover, if we use 20% as the threshold for proportionally excessively discordant STE, the sensitivity is higher and the specificity remains very high. I use 20%. Moreover, any ratio greather than 15% is very abnormal and should not be ignored.
The Queen of Hearts does not use the Smith modified Sgarbossa criteria per se, but as you can be seen below — the AI model correctly identifies the acute OMI in the setting of LBBB.
QoH interpretation

Precordial leads explainability
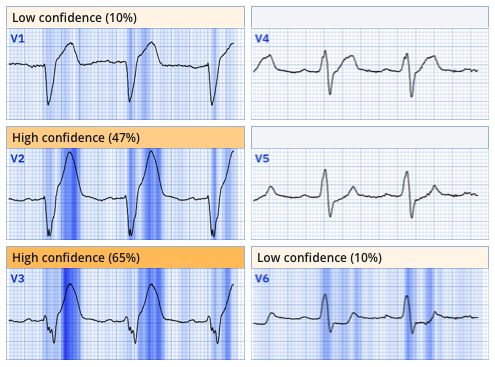
New PMcardio for Individuals App 3.0 now includes the latest Queen of Hearts model and AI explainability (blue heatmaps)! Download now for iOS or Android. https://www.powerfulmedical.com/pmcardio-individuals/ (Drs. Smith and Meyers trained the AI Model and are shareholders in Powerful Medical).
Outcome
I was sent this ECG by EMS and immediately recognized acute LAD occlusion in the setting of LBBB. This patient had a transportation time > 2 hours to the PCI fascility and thus thrombolytics were ordered. Thrombolytic therapy was administered by EMS within 16 minutes after the initial ECG and 41 minutes after the onset of symptoms. Within approximately 5 minutes of receiving fibrinolytic treatment — the patient’s symptoms improved, and the following sequence of ECGs was recorded. These ECGs are particularly interesting, illustrating the resolution of the complete left bundle branch block with reperfusion and demonstrating progressive improvement of the ECG over the next 30 minutes, including the regression of hyperacute T waves and development of TWI (T wave inversion).
Smith: thrombolytics have a significantly higher risk than angiography. First, angio can exclude OMI in cases of uncertainty. Second, if OMI is confirmed, then PCI is far safer than thrombolytics, which have a significant risk of intracranial and other bleeding.
ECG # 2 recorded 11 minutes after fibrinolytic therapy.

ECG # 3 recorded 15 minuter after fibrinolytic therapy

ECG # 4 recorded 21 minutes after fibrinolytic therapy

ECG # 5 recorded 26 mintues after fibrinolytic therapy

This patient received fibrinolytic therapy promptly after being diagnosed with OMI. Thrombolytics are most effective shortly after symptom onset which coincides with the time period of greatest benefit. As emphasized multiple times by Dr. Smith, Time is muscle! This concept is illustrated in the below graphical representation.
Temporal relationship between time and salvageable myocardium in patients with occlusion myocardial infarction
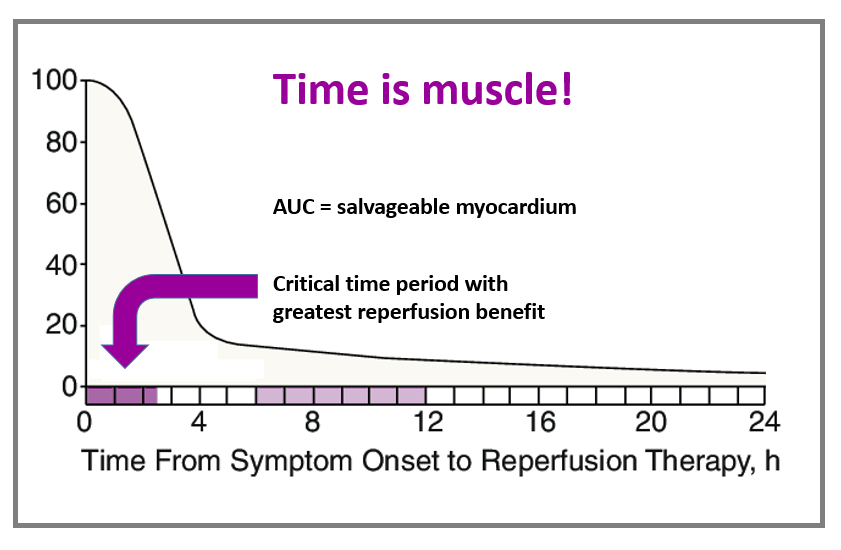
The graph was originally published here:
Gersh BJ, Stone GW, White HD, Holmes DR Jr. Pharmacological facilitation of primary percutaneous coronary intervention for acute myocardial infarction: is the slope of the curve the shape of the future? JAMA [Internet] 2005;293(8):979–86. Available from: http://www.ncbi.nlm.nih.gov/entrez/query.fcgi?cmd=Retrieve&db=PubMed&dopt=Citation&list_uids=15728169The patient became pain free following fibrinolytic therapy. During the hospital stay, the patient underwent coronary angiography, which did not reveal any significant thrombus or stenosis. This finding is not uncommon following timely thrombolytic therapy, as rapid treatment can dissolve thrombi before angiographic imaging is performed.
Intravascular imaging was subsequently used, identifying a culprit lesion with plaque rupture in the proximal wraparound LAD, which was treated with stenting. Troponin T peaked at 8199 ng/L — a markedly elevated value that, in this context, likely reflects rapid reperfusion and rapid “wash-out” of Troponin. Echocardiography demonstrated findings typical of LAD infarction, as shown below.
Focused view of the left ventricle from the apical window
Obvious mid to distal septal and apical hypokinesis of the left ventricle. It remains uncertain how much of the observed hypokinesis represents myocardial stunning (follow-up evaluation by repeat echo should answer this question).
Discussion
Understanding the Smith-Modified Sgarbossa Criteria can greatly assist in making crucial decisions for patients with high-risk ACS. The Queen of Hearts AI algorithm is a powerful tool for ischemia diagnosis, and is not limited by the traditional belief that ischemia cannot be detected in wide complex rhythms. In fact, the Queen of Hearts identified the initial ECG in today’s case as indicative of occlusion myocardial infarction (OMI) with very high confidence.

The AI model gives a reading of active OMI of 0,954 which is very high and corresponds to a specificity for OMI at well above 98%. The Queen of Hearts sees no signs of reperfusion or subendocardial ischemia reflected by outputs of 0,004 and 0,070 respectively.
ECG # 6, recorded the day after PCI

Smith: this shows that, even in LBBB, you get reperfusion T-waves. Wellens’ waves can be seen in both LBBB and Paced rhythm.
The patient in today’s case experienced an uncomplicated hospital course. A follow-up echocardiogram is planned to evaluate the extent to which the hypokinesis is attributable to myocardial stunning.
Learning Points:
- A presumed new LBBB is a poor predictor of acute OMI by itself. The QoH or the Smith-Modified Sgarbossa Criteria will help you evaluate if your patient with chest pain and LBBB might need thrombolysis or primary PCI.
- Thrombolytic therapy is most effective when administered promptly — and should be considered for all patients with OMI who are unable to reach the catheterization lab within 90 minutes.
- Delayed reperfusion usually leads to significant myocardial loss which is why OMI detection needs to be based on ECG (not on troponin)
- Repeat: thrombolytics have a significantly higher risk than angiography. First, angio can exclude OMI in cases of uncertainty. Second, if OMI is confirmed, then PCI is far safer than thrombolytics, which have a significant risk of intracranial and other bleeding.
- Thrombolytics were proven beneficial in patients with suspected MI and LBBB in the FTT collaborative. That was without any specific findings (without using the Modified Sgarbossa criteria (MSC). Here is a case if Intraventricular conduction delay barely meeting MSC that received thrombolytics and reperfused. And here is the ECG in that case:

You can see thant the ST/S ratio in V4 is greater than 25%. Moreover, V5 has as much R-wave as S-wave (an isoelectric QRS), and therefore SHOULD have an isoelectric ST segment (neither STE nor STD). The fact that there is ANY STE is diagnostic of LAD OMI.
Here is the Queen’s interpretation (output is 0.95, which is greater than 98% specific):

References
- Chang, A. M. et.al. (2009). Lack of association between left bundle-branch block and acute myocardial infarction in symptomatic ED patients. The American Journal of Emergency Medicine, 27(8), 916–921. https://doi.org/10.1016/j.ajem.2008.07.007
- Smith, S. W. et. al . Diagnosis of ST-Elevation myocardial infarction in the presence of left bundle branch block with the ST-Elevation to S-Wave ratio in a modified Sgarbossa rule. Annals of Emergency Medicine, 60(6), 766-76. https://doi.org/10.1016/j.annemergmed.2012.07.119
- Neeland, I. J., et. al. (2012). Evolving considerations in the management of patients with left bundle branch block and suspected myocardial infarction. Journal of the American College of Cardiology, 60(2), 96–105. https://doi.org/10.1016/j.jacc.2012.02.054
- Brown, A. J. et. al (2018). Prehospital diagnosis and management of acute myocardial infarction. In Springer eBooks (pp. 15–29). https://doi.org/10.1007/978-981-13-1114-7_2
Meyers HP, Limkakeng AT Jr, Jaffa EJ, et al. Validation of the modified Sgarbossa criteria for acute coronary occlusion in the setting of left bundle branch block: A retrospective case-control study. Am Heart J [Internet] 2015;170(6):1255–64. Available from: http://dx.doi.org/10.1016/j.ahj.2015.09.005Dodd KW, Zvosec DL, Hart MA, et al. Electrocardiographic Diagnosis of Acute Coronary Occlusion Myocardial Infarction in Ventricular Paced Rhythm Using the Modified Sgarbossa Criteria. Ann Emerg Med [Internet] 2021;Available from: http://dx.doi.org/10.1016/j.annemergmed.2021.03.036
= = =
======================================
MY Comment, by KEN GRAUER, MD (9/8/2025):
Today’s post by Dr. Nossen addresses the issue of assessing the patient with new CP (Chest Pain) and LBBB. Dr. Smith’s ECG Blog features many examples of this clinical entity (See My Comments in the January 23, 2025 post — the September 17, 2020 post and the April 7, 2019 post, among others).
The “beauty” of today’s case lies with the expeditious diagnosis and amazingly rapid initiation of thrombolytic therapy within 16 minutes after the initial ECG was recorded! (and within 41 minutes after the onset of symptoms!).
- Attestation to the benefit of such exemplary management was evidenced by: i) Symptom improvement in today’s case within 5 minutes of receiving thrombolytic therapy; and, ii) Ongoing dramatic improvement of acute ST-T wave abnormalities over the next 30 minutes on serial ECGs.
- KEY Point: Today’s case demonstrates that prompt initiation of thrombolytic therapy (especially if administered within the 1st hour after the onset of symptoms) — may result in dramatic clinical improvement with preservation of myocardium and cardiac function.
= = =
Another LOOK at the Initial ECG:
For clarity in Figure-1 — I’ve reproduced and labeled today’s initial ECG. I’ll highlight the following findings:
- The rhythm in ECG #1 is sinus. There is 1st-degree AV block ( = PR interval ~0.22 second). The QRS complex is markedly widened ( = 0.16 second). The axis is leftward (ie, about -30 degrees, as determined by predominant negativity in lead aVF, but an isoelectric complex in lead II).
- QRS morphology is consistent with LBBB (Left Bundle Branch Block) — given the monophasic upright R wave in lateral lead I, with predominant negativity in leads V1-through-V3. Although some might classify this conduction defect as IVCD (IntraVentricular Conduction Defect) instead of LBBB (because of the lack of a monophasic R wave in lateral lead V6) — associated LVH with LBBB rotates the vector of ventricular depolarization to the left and posteriorly, such that the monophasic R wave with LBBB will often be delayed until more posteriorly-lying leads V7 or V8 are recorded.
KEY Point: Sgarbossa Criteria are not needed to recognize the acute, extensive ongoing infarction that is already evident in today’s initial EMS tracing that is shown in Figure-1:
- As per Dr. Nossen — the shape of the ST-T waves in leads V1,V2,V3 (within the RED rectangle in Figure-1) is clearly hyperacute! Although LBBB is normally accompanied by large, upright T waves in anterior leads — such normal T waves should not be nearly as dominant as they are in ECG #1, in which T wave amplitudes in leads V2 and V3 exceed the depth of S waves in these leads. Hyperacuity of these T waves in leads V1,V2,V3 is further evidenced by the exceedingly wide T wave base in these leads.
- Although the T wave in neighboring lead V4 is not nearly as large as the T waves in leads V2,V3 — the overly wide T wave base in this lead suggests that it too is hyperacute (BLUE arrow in lead V4).
- To Emphasize (as per Dr. Nossen) — Smith-Modified Sgarbossa Criteria are satisfied in ECG #1 (especially in leads V2,V3 — with YELLOW arrows highlighting the abnormally elevated J-point in these leads). But in this 80-year old man with new 8/10 CP — the hyperacute anterior lead T waves alone are diagnostic of acute LAD OMI.
- Finally — the “eye-catching” shelf-like ST depression in lead V6 is clearly an unexpected and abnormal finding with LBBB. Together with the anterior lead ST elevation — this ECG picture qualifies as “Precordial Swirl” — which indicates acute proximal LAD occlusion (See the October 15, 2022 post for more on “Swirl”).
P.S: 2 Additional Findings in ECG #1
- Because LBBB alters the initial left-to-right direction of septal depolarization — there should never normally be “septal q waves” in lateral leads when there is LBBB (ie, Septal depolarization moves right-to-left with LBBB — which results in an all-upright R wave in lateral leads). As a result — the small q wave that we see in lead aVL (within the dotted RED circle in this lead) suggests there has been septal infarction at some point in time.
- The last ECG finding that I’ll draw attention to — is fragmentation of the S wave in lead V3 (ie, the jagged outline of the descending S wave — within the dotted BLUE oval in this lead). While not helpful in “dating” infarction — the presence of fragmentation suggests “scarring” (ie, from infarction or cardiomyopathy at some point in time).
Figure-1: I’ve labeled the initial ECG in today’s case. (To improve visualization of this tracing that had originally been recorded at 50 mm/sec. — I’ve digitized this ECG using PMcardio).




