This is a 30-something year old male with 1 week of constant left substernal chest pressure. Patient states the pain is non-radiating, it is not worse with breathing. It is not exertional and may have a positional component. He endorses some intermittent shortness of breath during this time and is using his inhaler for asthma as needed.
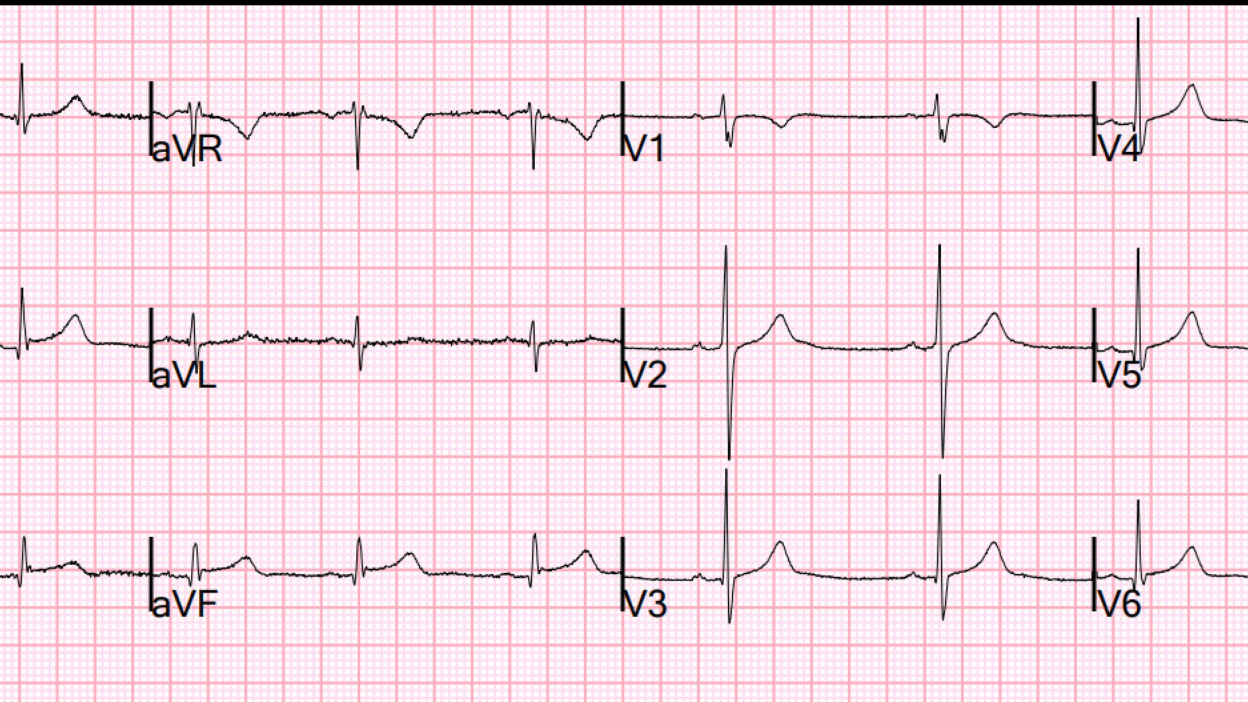
Here is his first ECG:
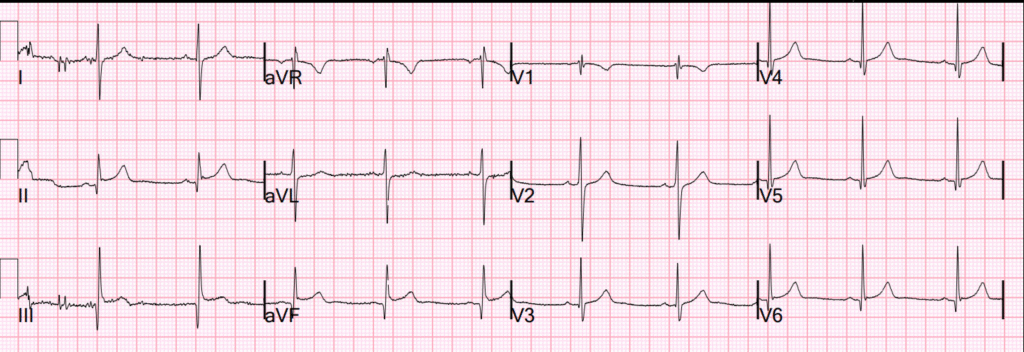
What do you think?
This was sent to me by text message with the information that the PMCardio Queen of Hearts had already opined that it was Not OMI. Probably because of this, they had waited for a troponin and it was undetectable, so with 7 days of chest pain, that almost rules out acute MI.
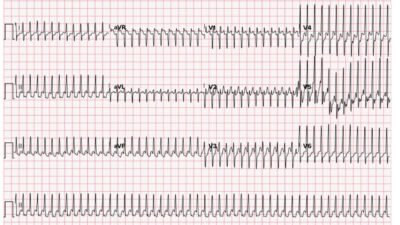
Queen here:

New PMcardio for Individuals App 3.0 now includes the latest Queen of Hearts model and AI explainability (blue heatmaps)! Download now for iOS or Android. https://www.powerfulmedical.com/pmcardio-individuals/ It is not yet FDA approved, but is CE approved in the EU.
The Queen does not explain why she thinks an ECG is NOT OMI.
My response was that it looked pretty scary and that I would be on the fence about activating the cath lab.
Why do I not think it is diagnostic of inferior OMI? In spite of STE meeting STEMI Millimeter criterial, it does not look diagnostic to me due to the very small T wave in lead III and the profound upward concavity in II and aVF. There is no definite ST depression in aVL and none in V2-V4.
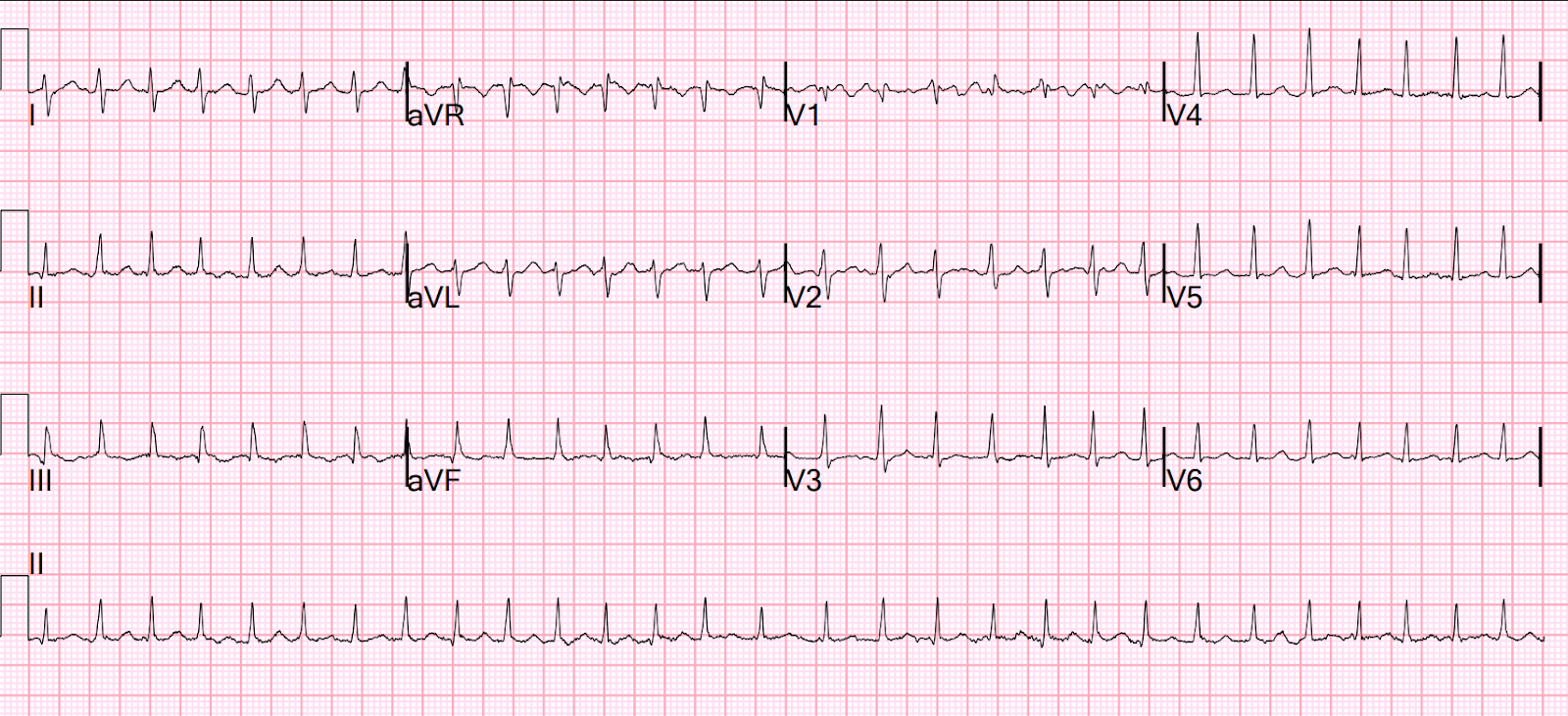
They recorded 2 more ECGs over 4 hours. Here is the 4 hour ECG:
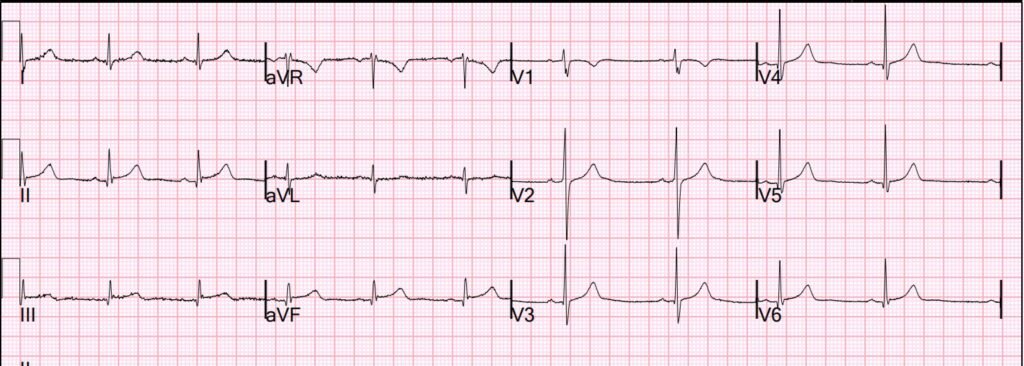
I think this one looks even scarier.
But the Queen is not disturbed:

There were 3 serial troponins and all were undetectable at < 3 ng/L.
With a truly DIAGNOSTIC ECG, do not trust even undetectable troponins. See this case. And other cases of Unstable Angina in the Era of High Sensitivity Troponin.
I trust the undetectable troponins this time because the ECG, though worrisome, is NOT diagnostic.
Does the PMCardio Queen of Hearts decrease False Positive Activations?
We will be presenting 2 studies at the Transcatheter Therapeutics (TCT) conference in San Francisco. Stay tuned for the results and explore the full agenda of OMI sessions and Queen of Hearts validations at TCT 2025 here.
= = =
======================================
MY Comment, by KEN GRAUER, MD (10/6/2025):
As always — I looked at today’s initial ECG before looking at what Dr. Smith and QOH said, as it’s best to be unbiased. My impression was identical to that of Dr. Smith — namely my uncertainty about whether or not this initial ECG represented an acute OMI.
- Point #1: I thought today’s initial tracing was non-diagnostic, in that I felt unable to rule out an OMI on the basis of ECG #1 without additional evaluation. And, this patient did present to the ED because of 1 week of constant left substernal chest pressure — so in addition to ruling out an acute event, priority should be given to figuring out why this patient’s CP (Chest Pain) has persisted for this duration of time.
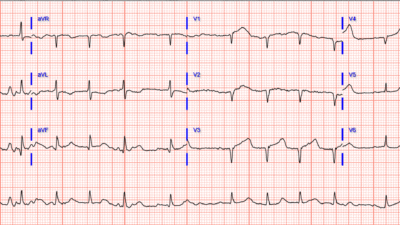
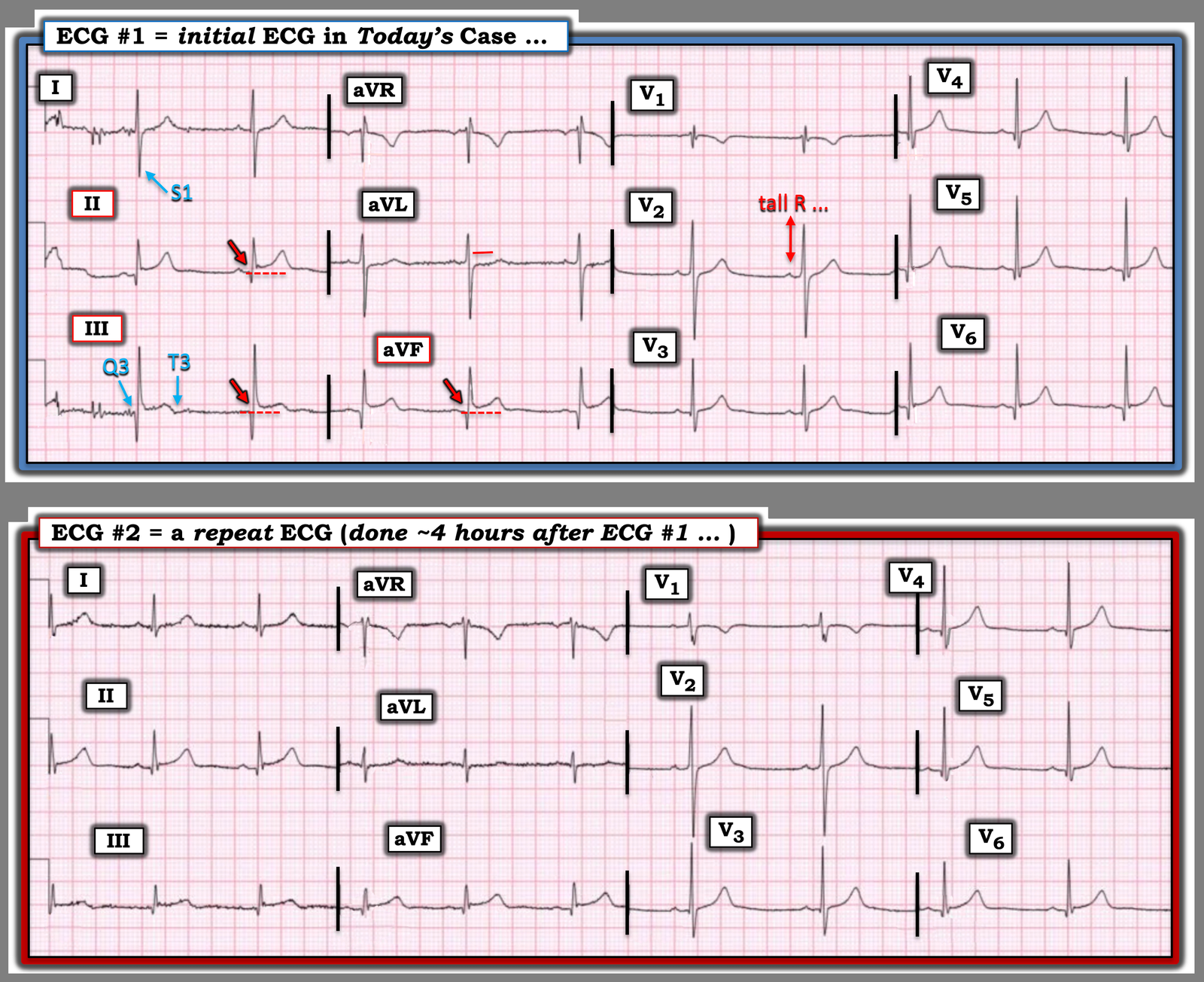
For clarity in Figure-1 — I’ve reproduced and labeled today’s initial ECG, together with a repeat tracing done ~4 hours later.
- Of note — there is an S1Q3T3 pattern in ECG #1. This is marked by an unusually deep S wave in lead I — with an almost equally deep (albeit narrow) Q wave in lead III — with subtle-but-present terminal T wave negativity in lead III. To Emphasize — There is no indication of pulmonary embolism in today’s case. The subtle rSr’s’ pattern in lead V1 lacks the terminal s wave in lead V6 for incomplete rbbb — and the rest of this ECG is not suggestive of PE (no RAA or RV strain). This highlights that the simple presence of an S1Q3T3 pattern is not indicative of acute PE in the absence of a suggestive clinical history and other ECG signs.
- That said — I interpreted the subtle terminal T wave negativity in lead III — together with the subtle ST segment flattening with ever-so-slight ST depression in lead aVL of ECG #1 as the main reasons for my uncertainty about this initial tracing.
- Q waves are present in each of the 3 inferior leads of ECG #1 — albeit despite their size, these Q waves are extremely narrow.
- ST segments are elevated in the inferior leads — although (as per Dr. Smith) with an upward concavity that is more often associated with a repolarization variant. Typically when there is acute infarction — a more comparable amount of ST depression will be seen in oppositely positioned lead aVL than the trivial amount of ST depression we see in ECG #1.
- Finally — there is no clear sign of posterior infarction. While transition is early (ie, the already tall R wave by lead V2) — the ST segments in leads V2,V3 are upward sloping and isoelectric instead of straightened and at least slightly depressed as they usually are when there is posterior involvement.
- BOTTOM Line: I was not prepared to rule out the possibility of an inferior OMI having occurred at some time during the 1-week course of this patient’s symptoms on the sole basis of this initial ECG.
Did you notice the axis shift in ECG #2?
- Whereas the nearly isoelectric QRS complex in lead I of ECG #1 suggests a vertical frontal plane axis — predominant positivity in lead I with equal positivity in leads I and II in the repeat tracing indicates an axis much closer to +30 degrees.
- While we don’t know the reason for this difference in axis in the repeat tracing — the point is that assessment for any changes in ST-T wave appearance between ECG #1 and ECG #2 must take into account this axis shift with resultant marked change in QRS morphology between the 2 tracings. That said — I did not think there was significant change between the 2 tracings.
= = =
Troponins ruled out an acute OMI …
- As per Dr. Smith — the finding of 3 negative serial Troponins ruled out an acute event, supported by a lack of significant change on serial ECGs (an earlier repeat tracing was also done, although not shown in this case). But does this rule out the possibility of underlying coronary disease in this patient whose ECG is non-diagnostic but not “normal”?
- Final Thought: We are not advised about further assessment of this patient’s symptoms. Given the presence of “constant substernal chest pressure” for a 1-week period, severe enough to prompt ED evaluation and this patient’s non-diagnostic but not “normal” ECGs — I would have considered CCTA (Chest CT Angiography) as a non-invasive test that could have been completed during the time this patient spent in the ED getting serial ECGs and Troponins. Doing so would have more definitively ruled out underlying coronary disease (and if nothing else — would have made it less likely that this patient would return to the ED if his “constant substernal chest pressure” continued). If his symptoms did continue — additional evaluation could then be safely pursued on an outpatient basis.
= = =
Figure-1: Comparison between today’s initial ECG — and the repeat ECG done ~4 hours later.
= = =
= = =