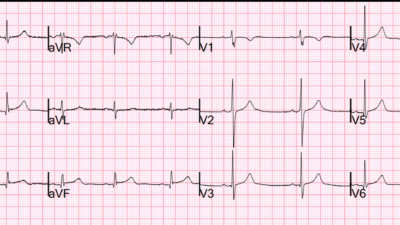
A 60-year-old man presented to the ED with chest pain and this ECG was recorded. Computer read this as normal.
What’s the diagnosis? (See below)
The findings went unnoticed. He subsequently went into V-Fib cardiac arrest. Watch this video breaking down this very important ECG case and see what happened!
When the conventional algorithm diagnoses an ECG as totally “normal”, it is often wrong. These algorithms especially miss specific but subtle findings of Occlusion MI (OMI). They not only miss them by calling “nonspecific ST-T abnormalities”, they miss by calling the ECG totally normal!!
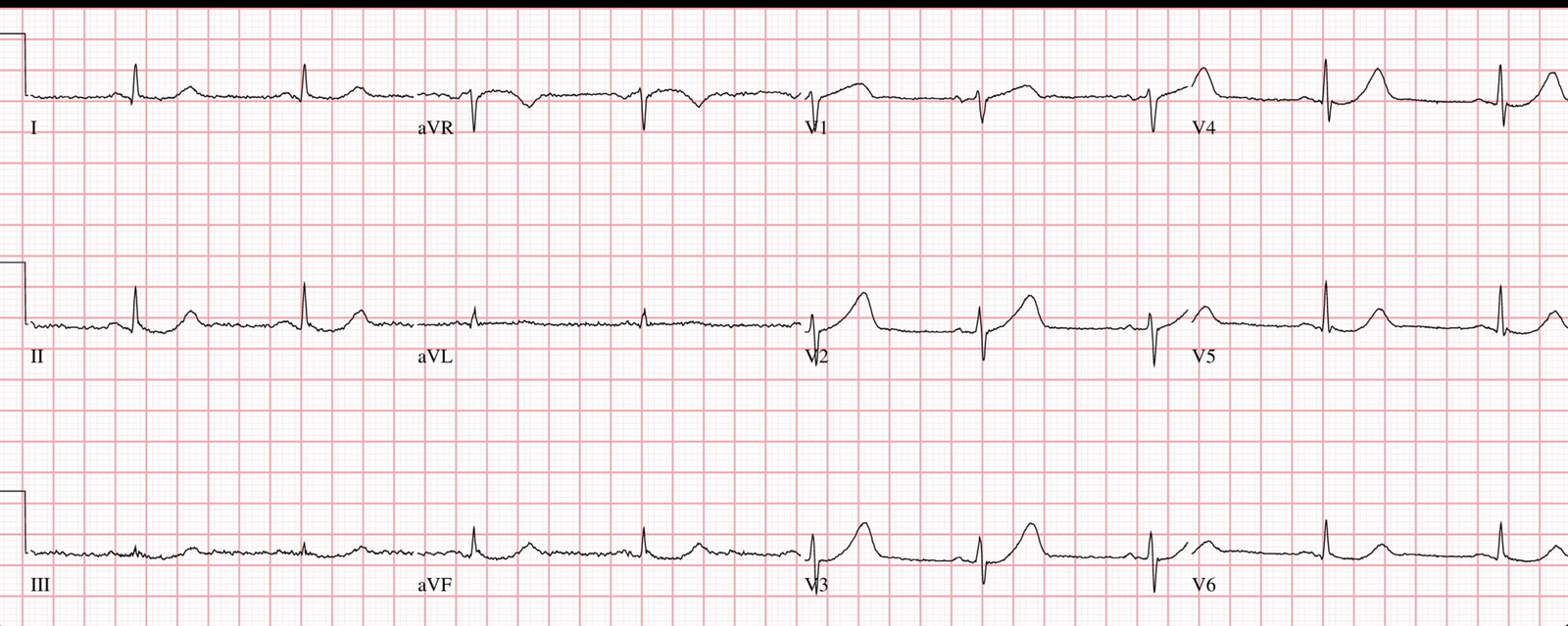
We showed that, among cases that Smith recognizes as OMI but the computer says are totally “normal” (again, not “non-specific ST-T”), and turn out to actually be OMI, the PMCardio Queen of Hearts AI Model not only recognizes that the ECG is abnormal, but diagnoses OMI in 80% of the cases! Full text: Artificial Intelligence Detection of Occlusive Myocardial Infarction from Electrocardiograms Interpreted as “Normal” by Conventional Algorithms
Additionally, we showed that with total LAD Occlusion, 38% (20/53) did not meet STEMI criteria on the first ECG and none ever developed STE. 17/20 had hyperacute T-waves on the first ECG; none ever evolved to STE. The PMCardio Queen of Hearts diagnosed all 53 on the first ECG: Failure of standard contemporary ST-elevation myocardial infarction electrocardiogram criteria to reliably identify acute occlusion of the left anterior descending coronary artery
The PMCardio Queen of Hearts AI ECG Model of course gets it right:
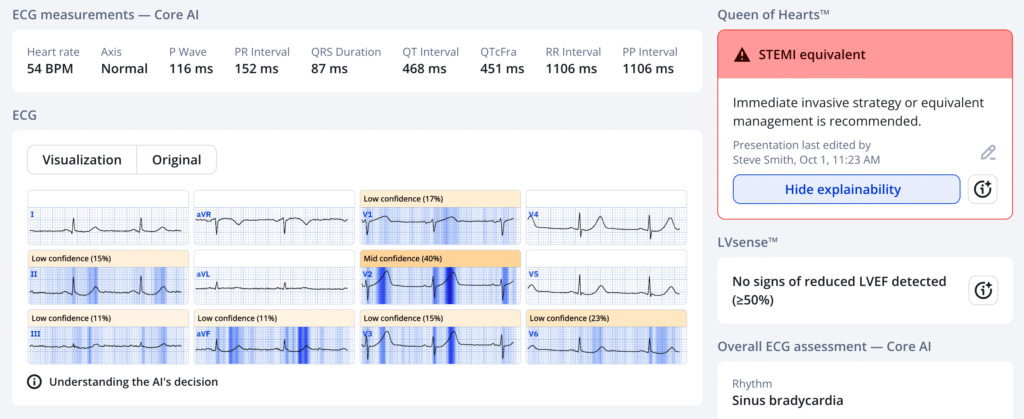
PMcardio for Individuals now includes the latest Queen of Hearts model, AI explainability (blue heatmaps), and %LV Ejection Fraction. Download now for iOS or Android: https://individuals.pmcardio.com/app/promo?code=DRSMITH20. As a member of our community, you can use the code DRSMITH20 to get an exclusive 20% off your first year of the annual subscription. Disclaimer: PMcardio is CE-certified for marketing in the European Union and the United Kingdom. PMcardio technology has not yet been cleared by the US Food and Drug Administration (FDA) for clinical use in the USA.
======================================
MY Comment, by KEN GRAUER, MD (10/4/2025):
Today’s case by Dr. Sam Ghali is notable for a series of oversights. Even without knowing many of the details of this case — the following is apparent.
- In a patient who presents to the ED for new-onset CP (Chest Pain) with the initial ECG shown above by Dr. Ghali — immediate cardiac catheterization is indicated without need for Troponin results, or even for repeat ECGs.
- Providers apparently depended on the computer interpretation and the use of STEMI criteria — thereby ignoring the fact that all 12 leads of the initial ECG are abnormal. And, as is often emphasized in Dr. Smith’s ECG Blog — the only computerized ECG program accurate for detecting an acute OMI in a STEMI-negative tracing is the QOH (Queen Of Hearts) application.
- Finally — We are told that “some time after the 1st ECG was recorded — the patient suddenly went into VFib”. Although the time frame between today’s initial ECG and the moment this patient arrested is not revealed — from the description we are told, that time frame during which the patient “flew under the radar” most likely was well over the 15-to-30 minutes maximum that one should wait before repeating the ECG in a patient who presents with new CP and a suspicious ECG.
Today’s 2 ECGs:
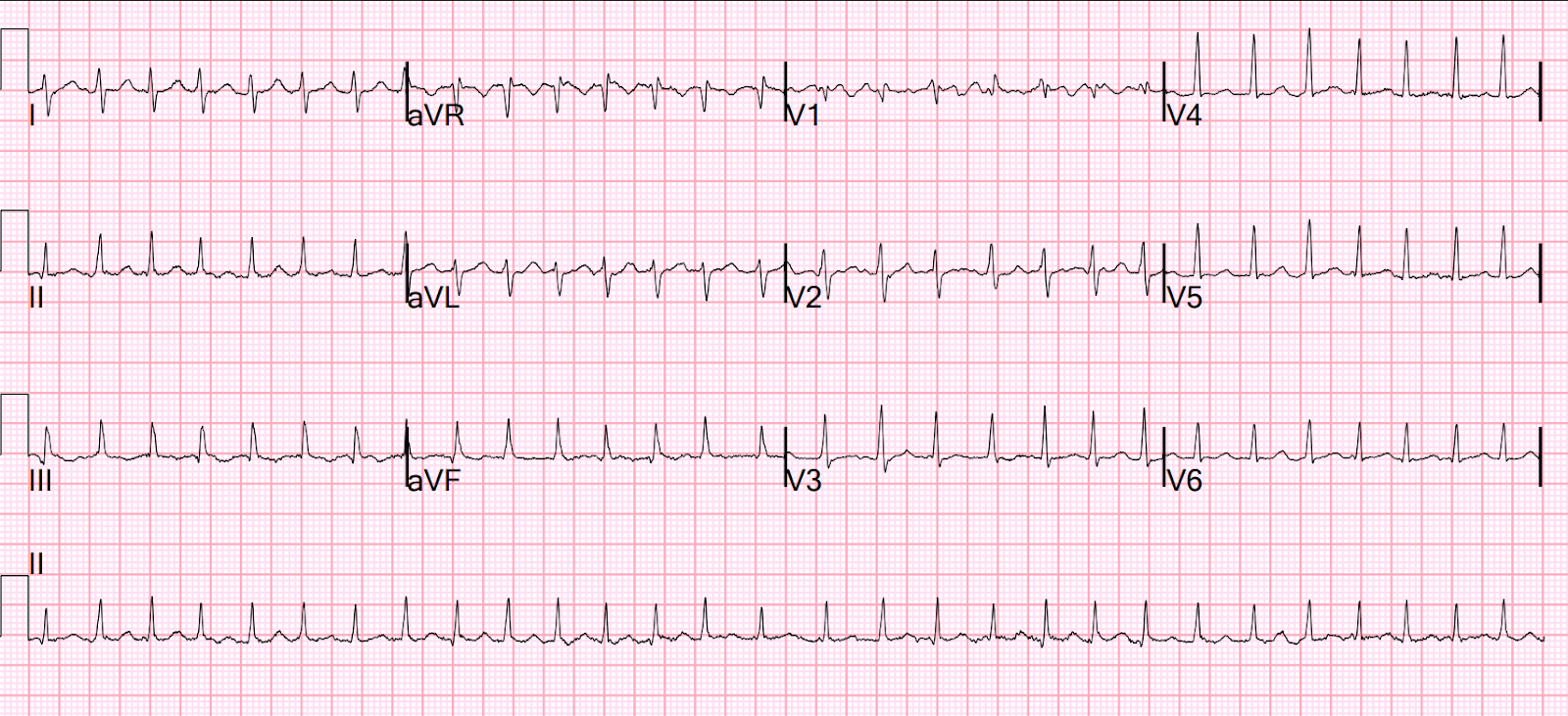
I’ll amplify Dr. Ghali’s excellent presentation with a few comments regarding today’s ECGs. To facilitate comparison of these tracings — I’ve put them together in Figure-1.
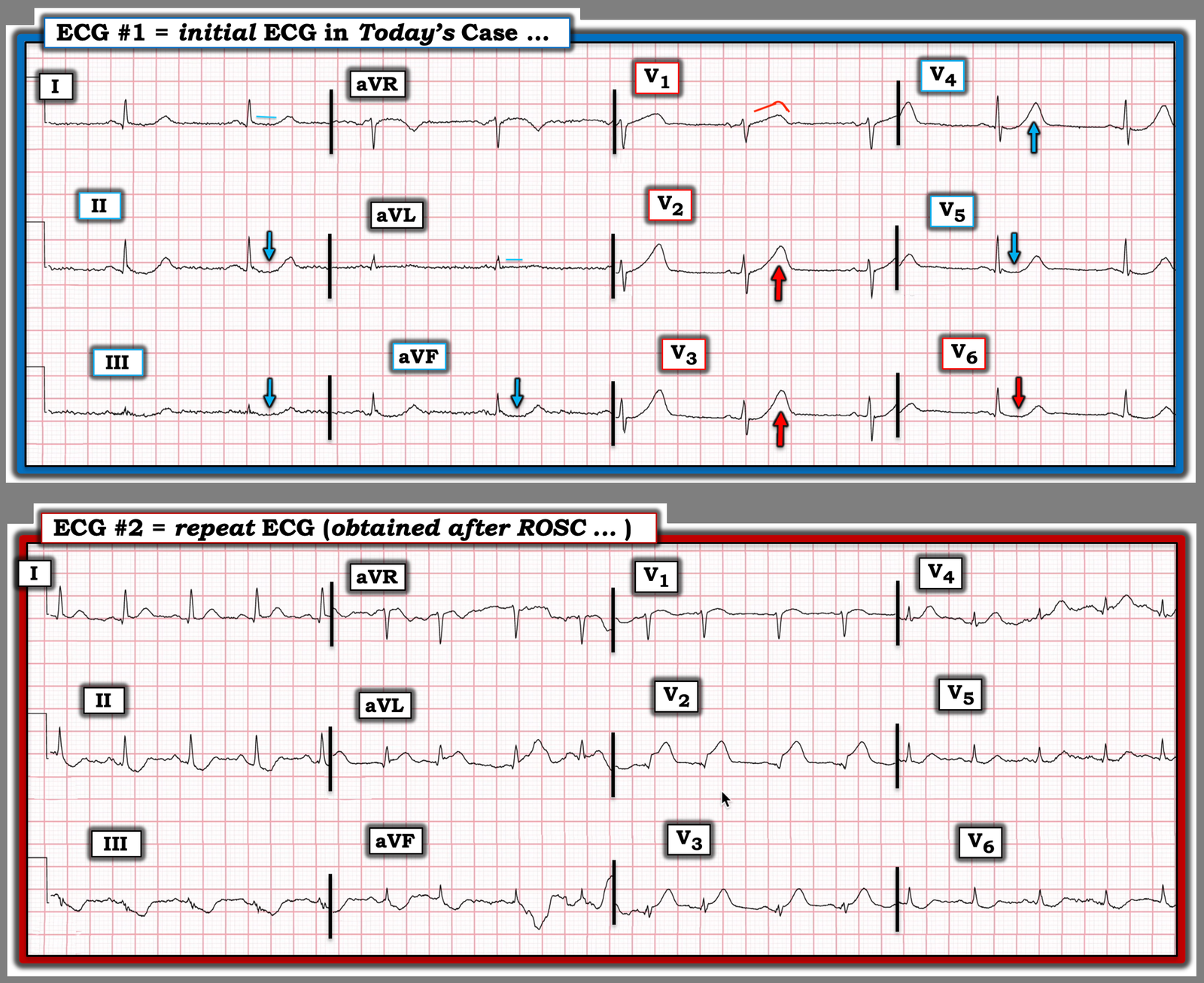
Figure-1: The 2 ECGs in today’s case.
All 12 leads in ECG #1 manifest at least some abnormality.
- As per Dr. Ghali (in this patient who presents with new CP) — my “eye” was immediately captured by lead V1. You virtually never normally see ST segment straightening with the degree of disproportionate “bulkiness” present in this lead (ie, with the T wave in V1 almost large enough to swallow the diminutive QRS that precedes it).
- As per Dr. Ghali — the concept of proportionality is KEY for assessing this initial ECG. Thus, the hyperacute T waves in leads V2 and V3 are not only “fatter”-at-their-peak and wider-at-their-base than expected — but these T waves are taller than the R waves in these leads.
- Neighboring lead V4 reflects an extension of these hyperacute T waves (albeit the R wave in V4 finally becomes a little taller than the T wave before it).
- We see something different in lateral chest leads V5,V6 — in that rather than hypervoluminous T waves — there is coved ST depression.
My Thought: I interpreted the overall ST-T wave picture in the chest leads of ECG #1 as consistent with the Precordial “Swirl” pattern that we often highlight on Dr. Smith’s ECG Blog (See the October 15, 2022 post — in which Dr. Meyers shows 20 cases of Swirl or Swirl Look-Alikes — and in which My Comment at the bottom of the page suggests the KEY findings to look for in leads V1 and V6).
- The clinical significance of recognizing “Swirl” — is that this pattern strongly suggests a very proximal site of LAD occlusion (usually proximal to the 1st septal perforator — with resultant septal ischemia in addition to anterior wall and apical involvement).
- The KEY to recognition of Swirl is the hyperacute and unusual ST-T wave appearance in lead V1, often with surprising ST elevation in this lead that looks different than the shape of the hyperacute ST-T wave in lead V2 — and — flattened or scooped ST depression in lead V6 (and sometimes also in lead V5).
Continuing with the limb leads in ECG #1:
- As per Dr. Ghali — reciprocal changes are seen in each of the inferior leads. The shape of these changes is similar to the scooped ST depression with terminal positivity that we see in leads V5,V6.
- Leads I and aVL manifest the subtle abnormalities of ST segment flattening.
- Completing the series of ST-T wave abnormalities in each of the 12 leads in ECG #1 — is the coved ST elevation in lead aVR, which itself is a reciprocal change that manifests a mirror-image opposite picture to the scooped ST depression seen in the infero-lateral leads (most probably reflecting diffuse subendocardial ischemia from the very proximal LAD occlusion).
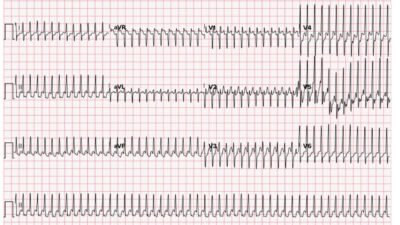
It’s easiest to appreciate evolution of today’s case by direct comparison of today’s 2 tracings in Figure-1:
- Note the increased heart rate in ECG #2 — in association with not only marked ST elevation now in leads aVL,V2,V3 — but also with loss of r wave from V1-to-V2, with a Q wave in lead V2 — and further loss of QRS amplitude in the chest leads (with this sinus tachycardia and marked low voltage in the chest leads of the post-resuscitation tracing consistent with cardiac stunning following cardiac arrest).
In Conclusion — Today’s patient was lucky to survive. One wonders how much myocardium was lost by the delay in recognizing his acute proximal LAD occlusion that was not optimally treated until cardiac arrest finally caught the attention of caretakers.
= = =