A middle-aged man with h/o asthma presented with SOB, especially with exertion. He also has positional chest pain. This started a few weeks ago and is worsening. Albuterol is not helping. He is a smoker and has a lot of weight loss as well.
By the time I came to the case, the patient had already been worked up for pulmonary embolism and was found to have a large lung mass compressing bronchi and pulmonary arteries, and some “tumor thrombus” (the extension of a solid cancer into blood vessels, creating a blockage composed of cancer cells rather than just blood components).
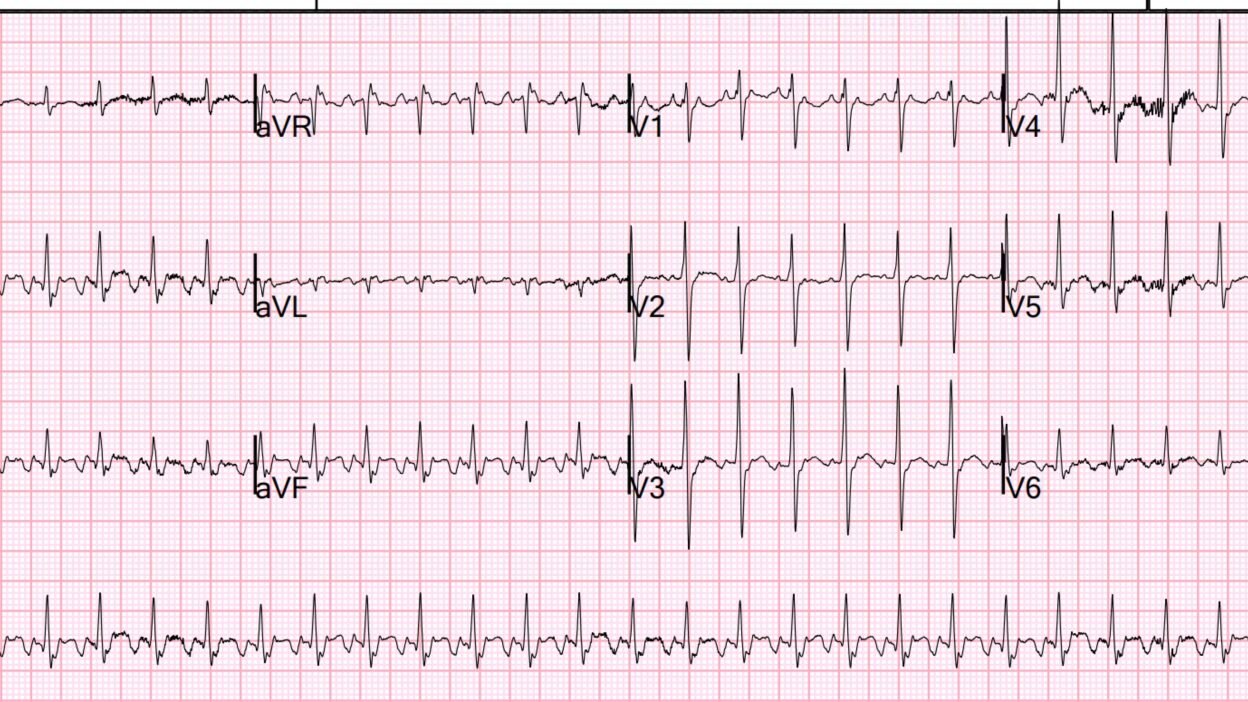
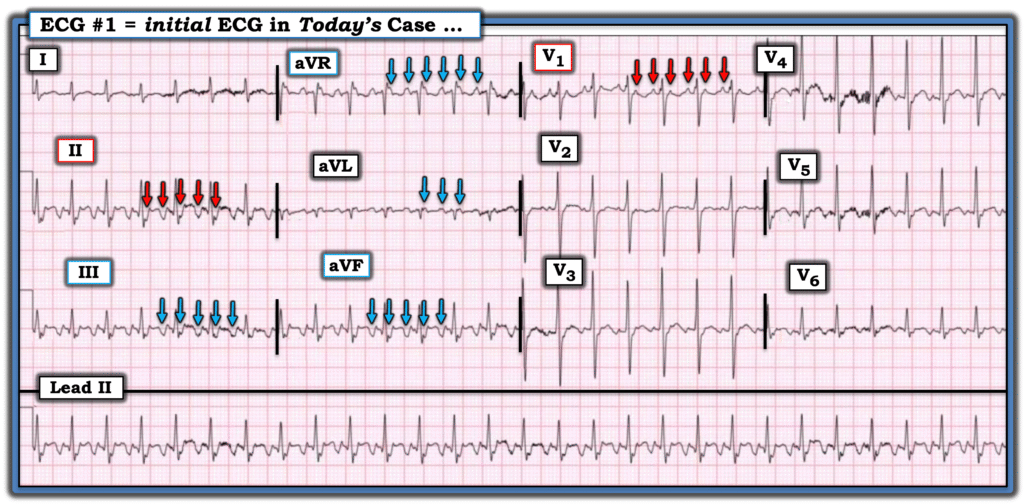
Here is his ECG:
What is the rhythm?
When I saw this I knew instantly that it was atrial flutter, and was a bit surprised that the providers who were caring for the patient did not see it. I always need to be reminded that EKGs are very very difficult for people who don’t yet recognized every pattern instantly.
Why is it atrial flutter:
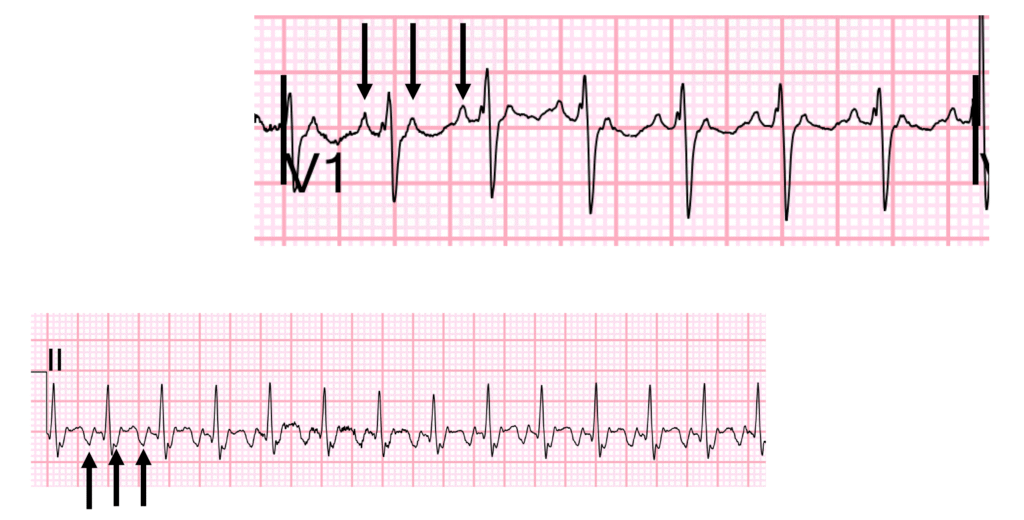
- The best leads to scrutinize are leads II and V1
- Atrial activity, if it is sinus, has an up-down P-wave in V1. Almost always. The initial “up” is the right atrial activity and the 2nd “down” is the left atrium. In this case, there are only fully upright atrial beats (see arrows in V1 below) which are spaced at exactly the same interval and there are 2 for every QRS. So there is 2:1 conduction.
- Look at lead II. You can easily see a sawtooth or undulating pattern, 2 for each QRS.
- The ventricular rate is 160, so the atrial rate is 320.
So how do we manage this patient?
First, you need to know the LV function. A bedside echo was done and showed very poor LV function.
Because of poor LV function, it could be quite hazardous to give beta blockade or calcium channel blockade to slow AV conduction, as these are negative inotropes (reduce contractility).
How about cardioversion?
His symptoms have been going on for weeks, so there is the risk of a thrombus in the atrial appendage which could embolize causing stroke.
The patient was very stable at rest, so there was no need for emergent cardioversion.
Therefore, I tried a digoxin load. (0.5 mg IV for the first dose)
By 3 hours, at which time one might see some effect if it is going to work, there was no change.
I consulted my “EKG Nerdz” text message group, which includes Pendell, Willy Frick, and Mark Hellerman. They recommended a CT scan of the atrial appendage, which I had never heard of. It turns out that this can be very sensitive for thrombus and, if negative, then electrical cardioversion can be safely done. See this article: Conclusions—Cardiac computed tomography, particularly when delayed imaging is performed, is a reliable alternative to TEE for the detection of LA/LAA thrombi/clot, avoiding the discomfort and risks associated with TEE
Unfortunately, the exam was not conclusive.
We admitted the patient. His rate could not be controlled with AV nodal blockers, and, the next day he underwent TEE which ruled out thrombus, followed by successful cardioversion.
= = =
======================================
MY Comment, by KEN GRAUER, MD (2/22/2026):
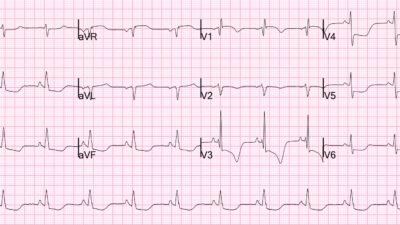
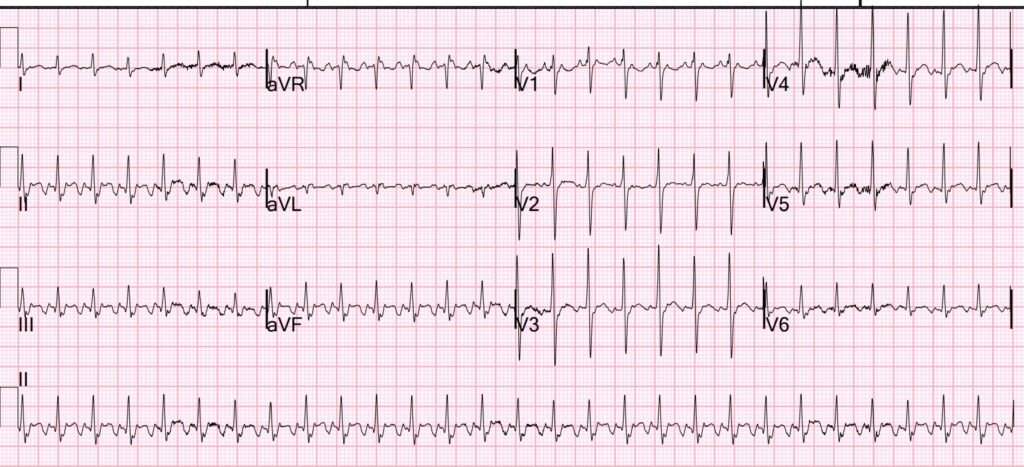
The ECG in today’s case shows AFlutter (Atrial Flutter) — Yet this diagnosis was overlooked by providers caring for the patient. I focus my comment on a few additional points to those emphasized by Dr. Smith. For clarity in Figure-1 — I’ve reproduced and labeled today’s ECG.
- In my experience — the most common oversight in arrhythmia interpretation committed by even experienced clinicians is “premature closure”. The tendency is to jump to a specific rhythm diagnosis to the exclusion of proceding in a systematic manner.
- As always — the 1st priority is to ensure that the patient in front of you is hemodynamically stable. Today’s patient was stable — so by definition, this meant that there is at least a moment in time to proceed systematically.
- As I review and work through in the November 12, 2019 post — By the P‘s, Q‘s, 3R Approach, the ECG in Figure-1 shows a regular SVT (SupraVentricular Tachycardia) at a rate of ~160-170/minute.
- This rhythm is not sinus tachycardia — simply because there is no upright P wave in lead II. Instead, there is a deep negative deflection in lead II — which by definition means that unless there is lead reversal or dextrocardia, the rhythm is not sinus tachycardia.
- While not impossible — a rate close to 170/minute is a bit fast for sinus tachycardia in an adult. Instead — awareness that the most commonly overlooked sustained arrhythmia is AFlutter — and — the realization that in the absence of sinus P waves, whenever we see a regular SVT at a rate close to 150/minute — this should immediately suggest the possibility of AFlutter.
- Untreated AFlutter most often presents with 2:1 AV conduction — which means that when looking for AFlutter, we are looking for leads that manifest 2 flutter waves for each QRS complex. As per Dr. Smith — leads II and V1 are generally the best leads for finding 2:1 flutter waves (RED arrows in Figure-1). But I always focus on 3 additional leads when looking for flutter waves = leads III, aVF and aVR (BLUE arrows in Figure-1). Other leads may also at times show 2:1 AV activity (as in lead aVL in Figure-1) — but leads II,III,aVF; lead aVR; and lead V1 are my “GO TO” leads for identifying underlying atrial activity when obvious P waves are not evident.
- BOTTOM Line: The easiest way to avoid overlooking the diagnosis of AFlutter — is simply to think of AFlutter whenever you see a regular SVT at a ventricular rate close to 150/minute in the absence of sinus P waves.
= = =
P.S.: A Final Observation …
Over the years — I’ve been impressed by how often I’ve seen atrial arrhythmias in association with longterm pulmonary disease. Most emergency providers are aware of the close association between MAT (Multifocal Atrial Tachycardia) and patients with COPD (See My Comment at the bottom of the page in the January 5, 2020 post) — but AFlutter is also surprisingly common in this clinical setting, as well as in association with other forms of longterm, severe pulmonary disease.
- The literature supports this frequent association of atrial arrhythmias with severe pulmonary disease — perhaps through the mechanism of chronic hypoxia with resultant right atrial pressure overload leading to atrial distention and right atrial fibrotic remodeling (Vahdatpour et al — Pulm Circ 10(1):1-13, 2020).
- Given today’s patient’s known history of asthma, smoking and now discovery of a large lung mass — the history presented yet one more reason to consider AFlutter as the etiology for the regular SVT that this patient presented with.
= = =
Figure-1: I’ve reproduced and labeled today’s ECG.
NOTE: I have been adding selected short ECG Videos on arrhythmia interpretation — that can be found in the TOP Menu on any page in Dr. Smith’s ECG Blog — CLICK HERE — if interested — 🙂
= = =
= = =
= = =