This case was texted to me by one of our residency graduates, and with the outcome, so I don’t know how I would have interpreted it blindly.
A 50-something male who is healthy and active with no previous medical history presented with 5 hours of continuous worrisome chest pain.
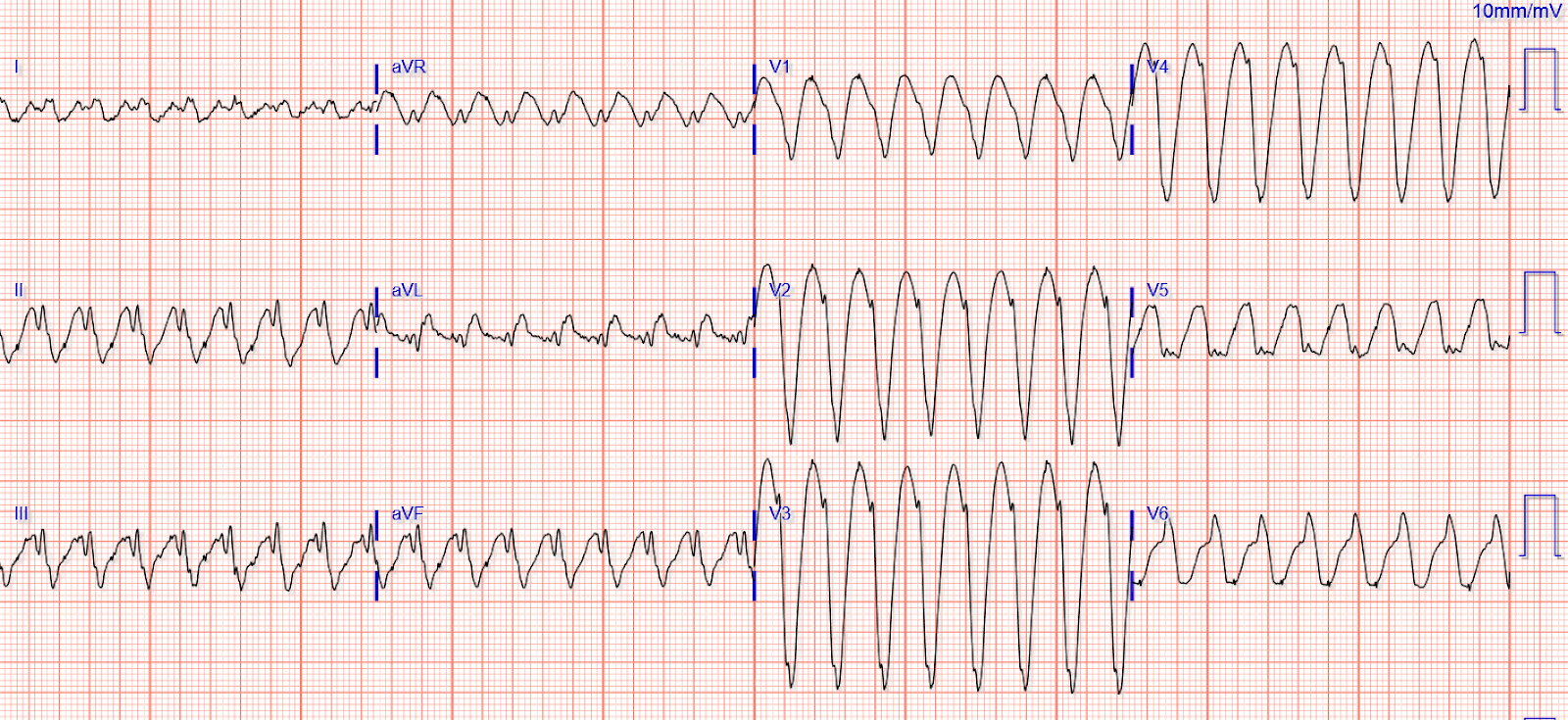
Here is his ECG (there was no previous ECG available):
 |
| What do you think? |
There is sinus rhythm with Left Bundle Branch Block (LBBB). This is presumably and new LBBB, but that is uncertain.
There is less than 1 mm of concordant ST Elevation in lead V5. This is pretty specific for OMI but not very sensitive (see table below).
The highest ST/S ratio is in V3, and is 2.5/13 = 0.19. 0.19 is a high ratio, but not the most accurate. The average highest ST/S ratio in V1-V4 for a normal LBBB is about 0.11. 0.20 is about 84% sensitive and 94% specific in our validation study. So 0.19 is worrisome!
Chest pain with New LBBB: It helps to actually measure the ST/S ratio
A Fascinating Demonstration of ST/S Ratio in LBBB and Resolving LAD Ischemia
The cath lab was activated. Shortly thereafter, the first troponin I returned at 0.689 ng/mL (URL = 0.034), all but diagnostic of acute MI.
The LAD was 100% occluded. It was opened and stented.
Subsequent Peak cTnI was 46.84 ng/mL (consistent with LAD occlusion).
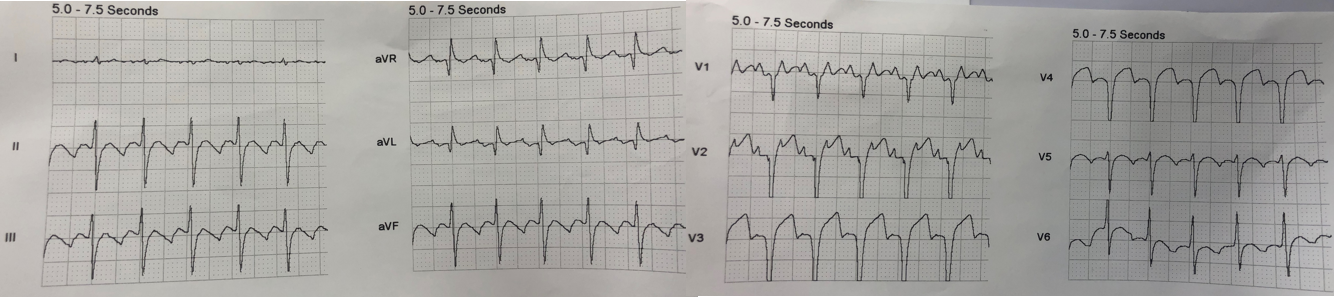
There was an ECG recorded the next AM:
 |
| It does not appear much different! But there are subtle differences: 1. The T-wave is not as tall. 2. There is the beginning of terminal T-wave inversion in V1-V3. |
Here they are, side by side for comparison:
The provider, and former HCMC EM resident, was exceedingly perceptive and able to accurately diagnose LAD occlusion from this very subtle ECG.
Comment
The doctor saw this ECG and had a sense, in combination with the worrisome clinical presentation, that this was an ischemic LBBB. But it is by no means obvious, and does not strictly meet the Modified Sgarbossa Criteria, which require (in at least one lead):
1. 1 mm of concordant STE or
2. 1 mm of concordant STD in V1, V2, or V3
3. Excessively discordant STE, as defined by at least 1 mm and with an ST/S ratio of 25% or more.
How about “New (or presumably new) Left Bundle Branch Block”? This was formerly an indication for cath lab activation, but was abandoned in the 2013 guidelines because of poor specificity. The best study was an ED study that showed that about 7% of patients with chest pain and new LBBB in the ED were diagnosed with acute MI. The number with Occlusion MI (OMI) would be far fewer, in the range of 2-3%. This is why the Modified Sgarbossa Criteria, and use of troponin and the following algorithm are so important.
Chang et al. Lack of association between LBBB and Acute MI in symptomatic ED patients. https://www.sciencedirect.com/science/article/abs/pii/S0735675708005299
Interestingly, the rate of OMI among ALL patients with ischemic symptoms in the ED is only 1-5%, no matter whether there is LBBB or not!
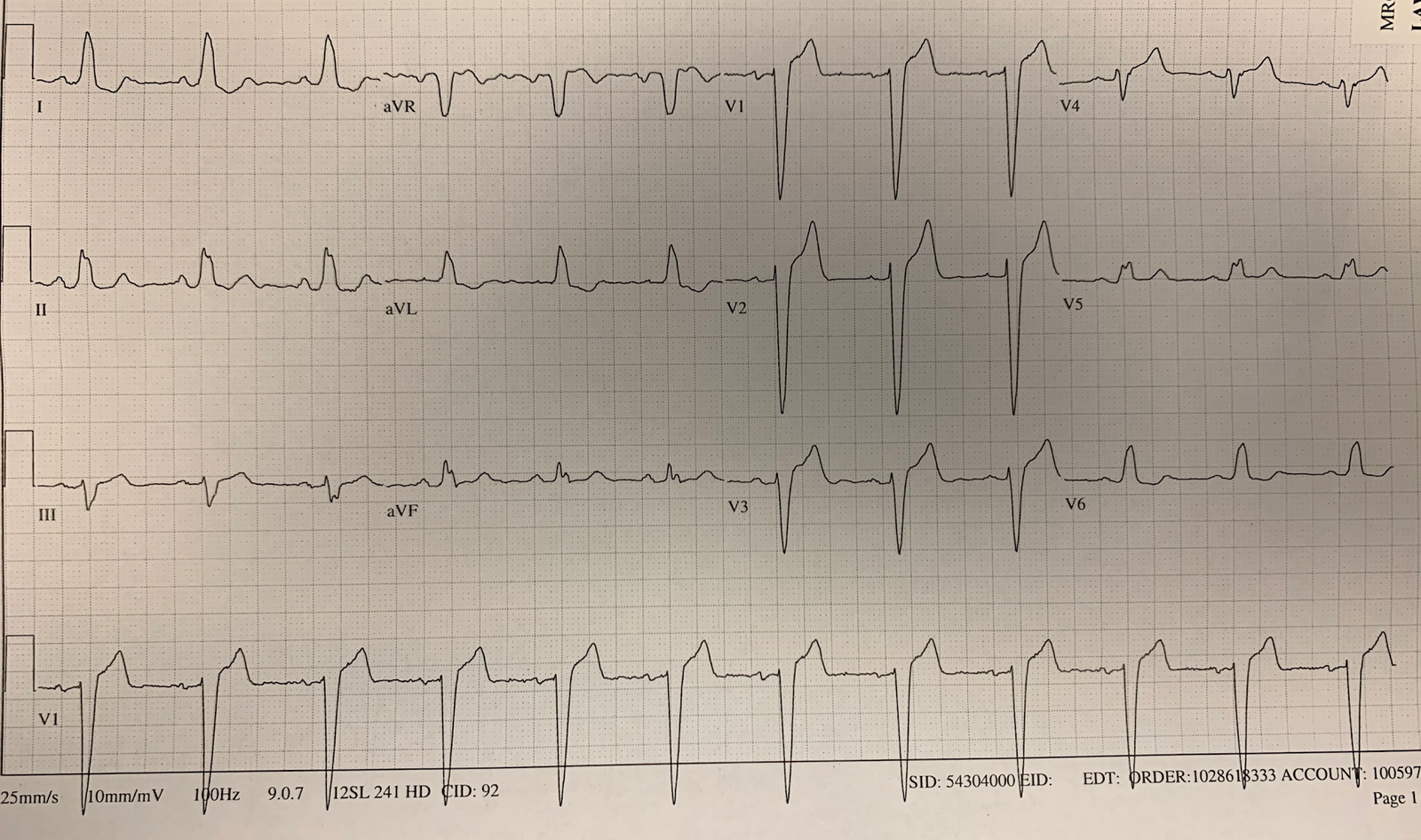
Here is an algorithm that is very useful in such cases, published by Cai and Sgarbossa in 2013.
 |
| Algorithm for LBBB (also good for managing OMI in paced rhythm) |
So in this case, if the provider had not been certain of the ECG, he could have waited for the troponin. Since the pain had been constant for 5 hours, it would be unlikely to be negative in the presence of acute OMI. Then, after a short wait for the troponin which was indeed elevated, cath lab activation is indicated regardless of the ECG.
This is also true in normal conduction, not just LBBB!
If a patient has symptoms of ACS, and they are persistent, and a diagnostic troponin, then cath lab activation is indicated.
Here is a paper we published on other measurements and their diagnostic utility for occlusion (see Table):