A very elderly man fell and injured his face. There is always the possibility of syncope as the etiology of a fall, especially in an elderly person.
I was consulted on his ECG.
He had no chest pain, nor chest pain shortly before presentation.
 |
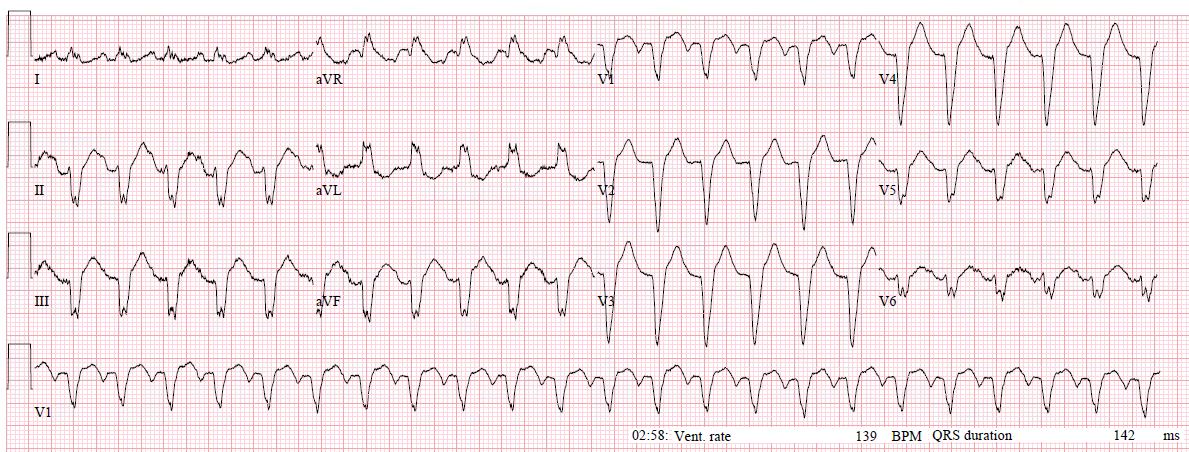
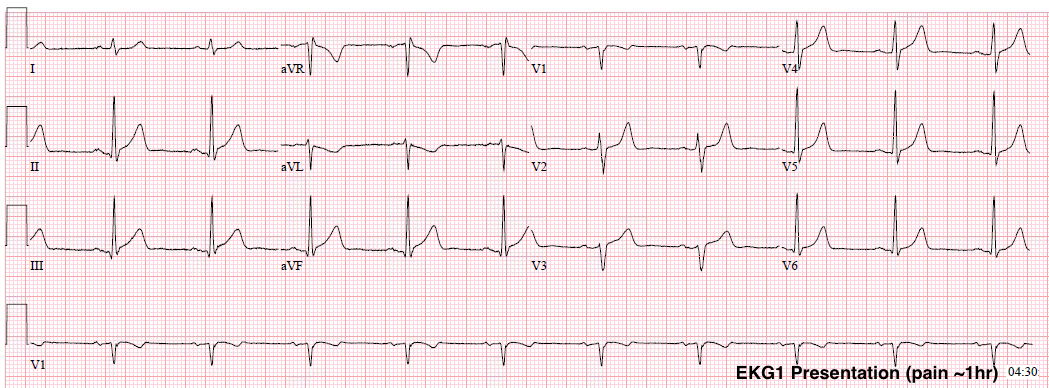
| What do you think? This is what the treating physicians wrote: “Syncope workup notable shows abnormal EKG with Wellens’ waves in V2 and V3.“ |
My opinion was this:
“There are no R-waves in V2 and V3, so it is not Wellens’. Furthermore, it can’t be Wellens’ syndrome even if the ECG is true Wellens’ morphology: Wellens’ syndrome requires that the ECG be recorded after an episode of chest pain that is now resolved. This patient had no pain at any time.”
I asked:
“Is there a previous ECG for comparison?” (No, there was not)
Continued
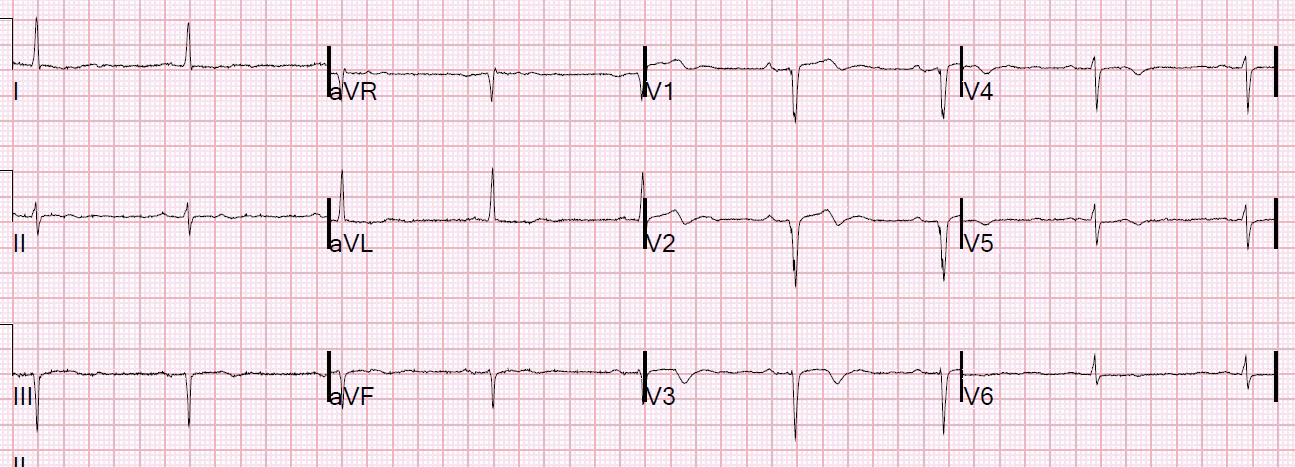
“The QS-waves and shallow T-wave inversion are typical of a dense old transmural anterior MI, and may represent an aneurysm of the LV anterior wall. There could be some acute NonSTEMI superimposed on old MI, but the ECG does not make me worried for LAD acute coronary syndrome and not for acute coronary occlusion. If these T-waves are due to acute ischemia, then the troponin will be positive. So just get serial troponins.”
Outcome
The patient ruled out for MI, with all troponins below the level of detection.
A previous echocardiogram was found, which showed
Regional wall motion abnormality-distal septum, anterior and apex, hypokinetic, large.