An 80-something called 911 for chest pain, generalized weakness, and cough.
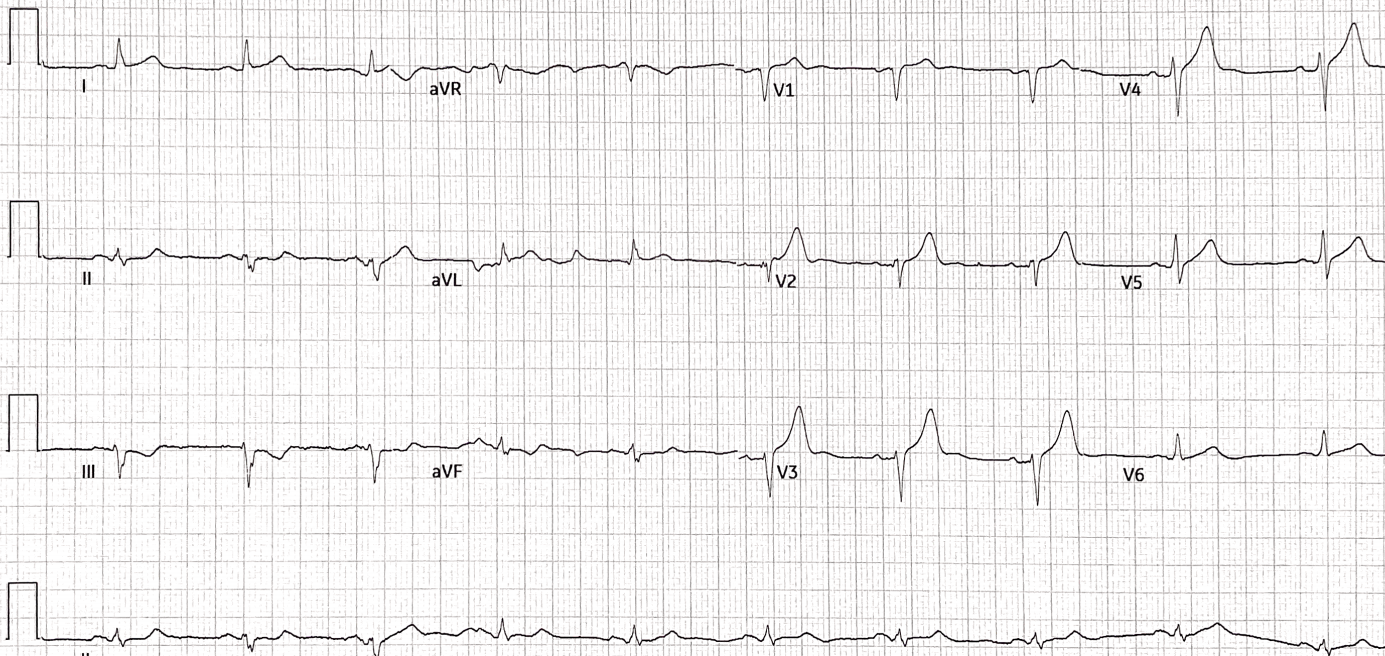
Here is his prehospital ECG:
The medics were worried about this ECG and activated the cath lab
Smith: As in many prehospital ECGs with large voltage, the tracing goes off the image, making assessment of voltage impossible. Thus, it is impossible to assess the ST Segments and T-waves, which should always be assessed in proportion to the size of the QRS. I call this “proportionality” and in a non-ischemic ECG, the repolarization should always be proportional to the depolarization.
Since we can’t see the true size of the QRS, we cannot assess proportionality.
So an ECG like this should not precipitate cath lab activation.
On some machines, one can change the settings of millimeters per millivolt and re-record. Standard measurements are 0.1 mVolt = 1mm (as in this case), but it can be changed on most ECGs to “half standard” which means that 0.1 mV = 0.5 mm and the QRS complexes then are half sized.
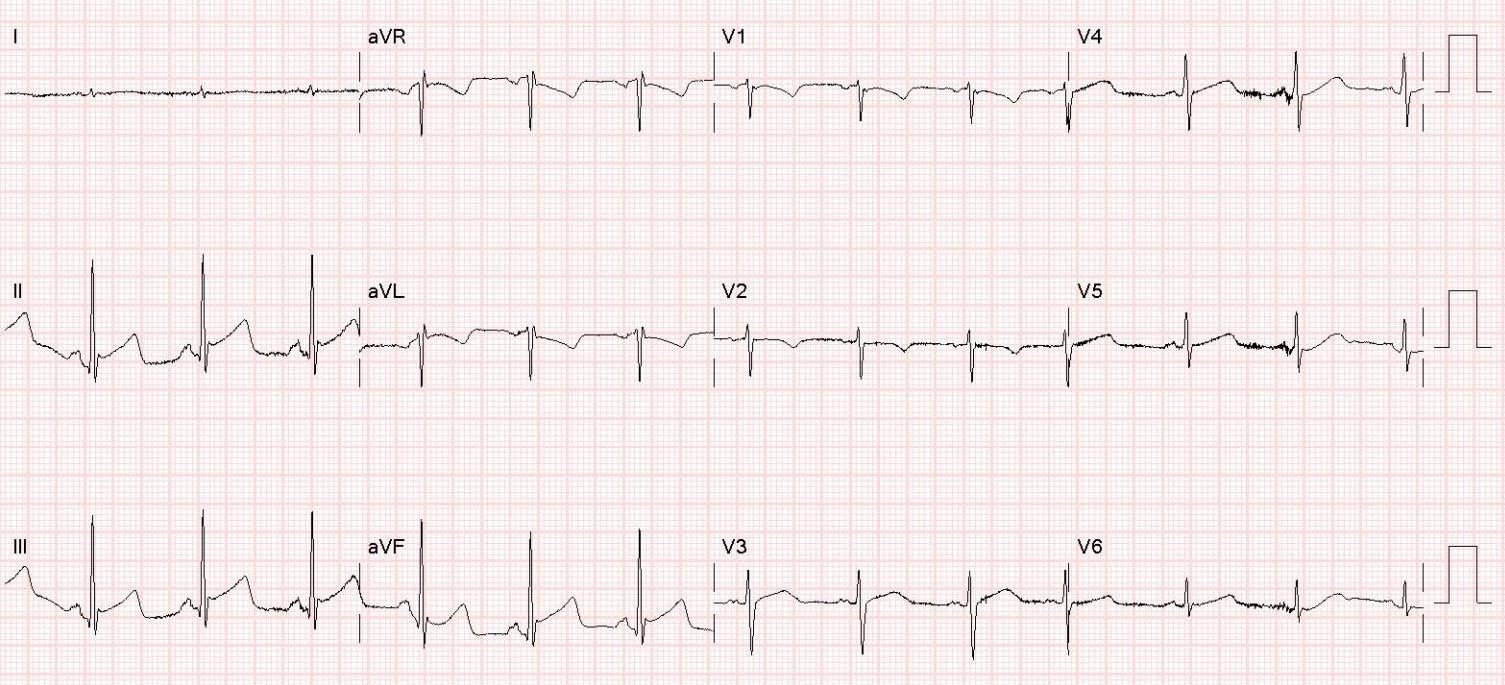
When the patient arrived, an ED ECG was recorded:
Rhythm is uncertain but probably supraventricular at a rate of 100.
There is RBBB and LAFB and Massive LVH.
No ST segments are out of proportion to the QRS.
A bedside cardiac POCUS was done, short axis:
This shows very hypertrophied myocardium
Long axis
Again, very hypertrophied myocardium
There was no previous ECG on file.
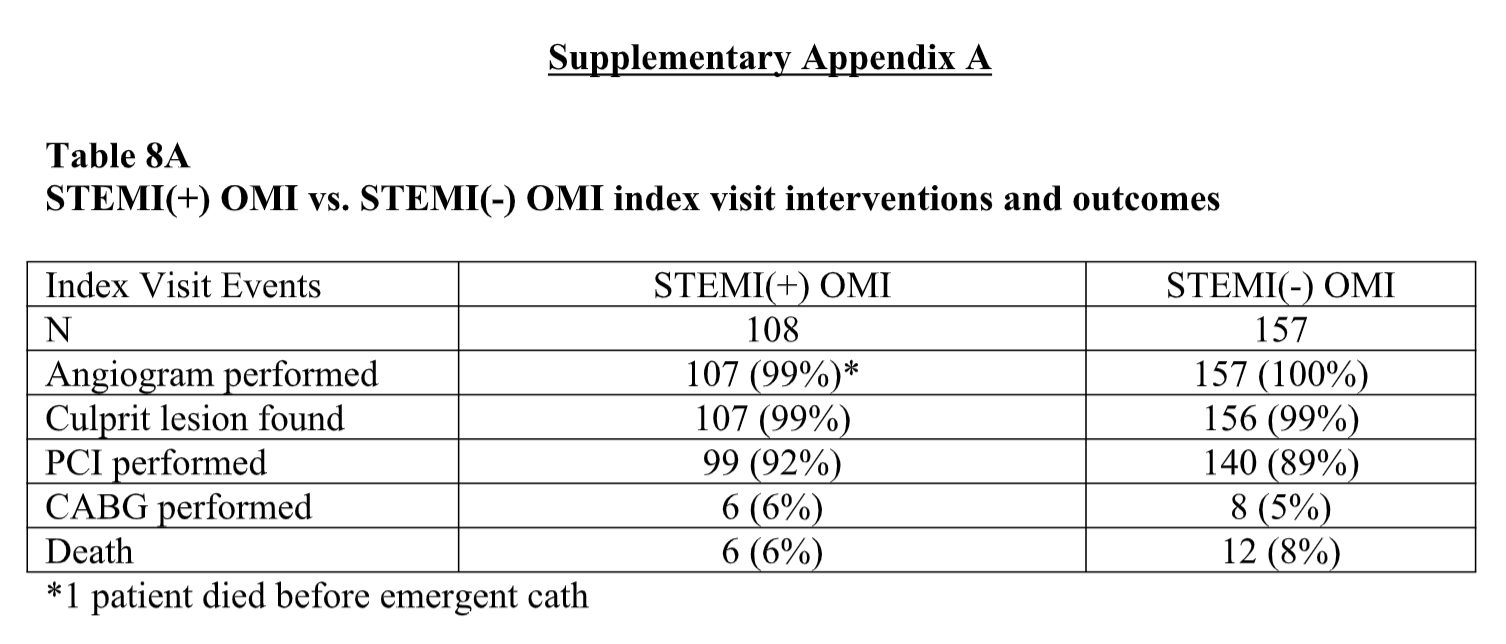
Another ECG was recorded shortly thereafter:
Now P waves are visible in lead V1
(See biphasic wave approximately 200 ms AFTER the QRS.)
Thus, there is very prolonged PR interval, at approximately 400 ms. Then RBBB with LAFB is confirmed.
Thus, this is often called Trifascicular Block. (Bifascicular block PLUS very prolonged PR interval) and it is associated with progression to complete heart block.
Read more about “Trifascicular block” here:
Symptomatic Bradycardia. So-called Trifascicular Block. Occum’s Razor and Hickum’s dictum.
Formal Echo with contrast
–Normal left ventricular systolic function, lower limits of normal; estimated left ventricular ejection fraction is 50%
–Regional wall motion abnormality- mid-inferolateral hypokinesis.
–Marked left ventricular hypertrophy, concentric.
–Normal right ventricular size and function.
The patient turned out to have Covid pneumonia and an elevated hs troponin to 544 ng/L due to type II MI.
The myocardial diagnosis is hypertrophic cardiomyopathy (HOCM).