Case 1:
The outcome of this case is at the far bottom.
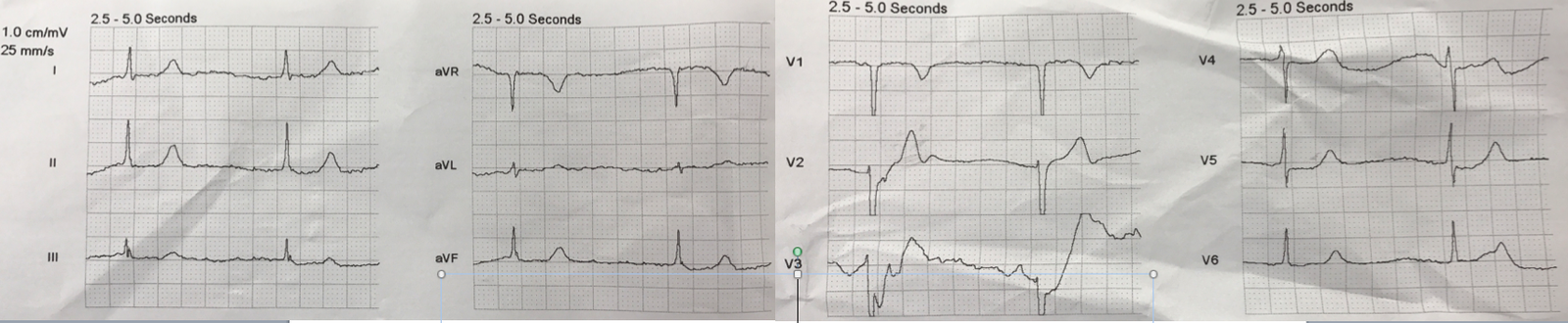
A thin, athletic young African American male presented by private transportation to the ED after use of “ecstasy” and alcohol and other drugs. He complained of severe chest pain and was extremely agitated, so much so that he was throwing chairs in triage. He had an ECG recorded and was brought to a room. Here is the ECG:
Figure 1:
 |
| Sinus rhythm. What do you think? |
Figure 1 shows marked ST Elevation (STE) at the J-point relative to the PQ junction:
1.5 mm in V2
3.0 – 3.5 mm in V3
2.0 mm in V4
The size of the T-wave relative to the QRS in lead V2 is concerning; it is due to very low QRS voltage.
Technically, the STE meets STEMI criteria because there is greater than 2.5 mm STE in V3 and greater than 1 mm in an the adjacent lead V4 (even though V2 does not meet criteria of 2.5 mm).
But this is a thin athletic 20-something and since such STE can occur in this population, it is easy to dismiss it. The normal upper limit for ST Elevation in lead V2 (as measured at the J-point, relative to the PQ junction) in males under 30 years is 3.0 mm and 3.5 mm in 20 year old males.
How about using the LAD-early repol formula to help differentiate normal variant ST elevation from the ischemic ST elevation of LAD occlusion?
The formula comes from this paper:
In this complex paper, we compare Subtle LAD occlusion to early repolarization (now known as “normal variant ST elevation””). All early repolarization ECGs had to have at least 1 mm of ST elevation in V2 and V3 (of 242 cases of early repol, 71 were excluded due to absence of sufficient STE), at the J-point, relative to the PQ junction.
Among LAD occlusions, “Subtle” meant we excluded those ECGs we defined as obvious:
1) greater than 5 mm ST elevation in at lead one lead
2) just a single lead of V2-V5 with a straight or convex ST segment
3) any ST depression (inferior or anterior)
4) any Q-waves in V2-V4.
5) T-wave inversion in any of V2-V6
These ECGs were excluded from the study as “obvious” LAD occlusion, and the formula was not derived or validated on those patients, and therefore should not be applied.
On this blog, the warning is this:
It is critical to use it only when the differential is subtle LAD occlusion vs. early repol. Thus, there must be ST Elevation of at least 1 mm. If there is LVH, it may not apply. If there are features that make LAD occlusion obvious (inferior or anterior ST depression, convexity, terminal QRS distortion, Q-waves), then the equation MAY NOT apply. These kinds of cases were excluded from the study as obvious anterior STEMI.
The formula is also at MDCALC: https://www.mdcalc.com/subtle-anterior-stemi-calculator
iPhone app
There is a free iPhone app called “SubtleSTEMI”. (Sorry, no Android) When you open the app, this caution comes up:
If you click on “show warning,” this comes up:
 |
| You must click this in order to proceed. |
Then you must answer all these questions. If the answer to any is “Yes”, you cannot trust the formula.
 |
| Then you must answer all these questions. If the answer to any is “Yes,” you cannot trust the formula. |
| If the answer to all these is “NO,” then the formula can be applied. But still the formula was not perfect: it was about 90% sensitive (86% actually, at the most accurate cutoff of 23.4) and 90% specific. Because normal variant ST elevation is far more common that LAD occlusion, especially among 20-somethings, the negative predictive value in this population is indeed very high. The NPV is even higher for a young athletic male who presents with drug use and agitation! |
The Fourth Question: Terminal QRS distortion:
Notice the 4th Question: “Is there terminal QRS distortion?”. This is confusing to people, but is very important: 20% of our exclusions were due primarily to terminal QRS distortion.
Terminal QRS distortion (TQRSD) is something I noticed long ago in LAD occlusions, and did not see in normal variant ST elevation. That is why we excluded patients with this finding.
Definition of TQRSD: Absence of S-wave and J-wave in either of leads V2 and V3.
Last year, we studied it among the 171 patients with proven Normal Variant ST Elevation:
Thus, if there is TQRSD, assume LAD occlusion until proven otherwise.
What is a J-wave?
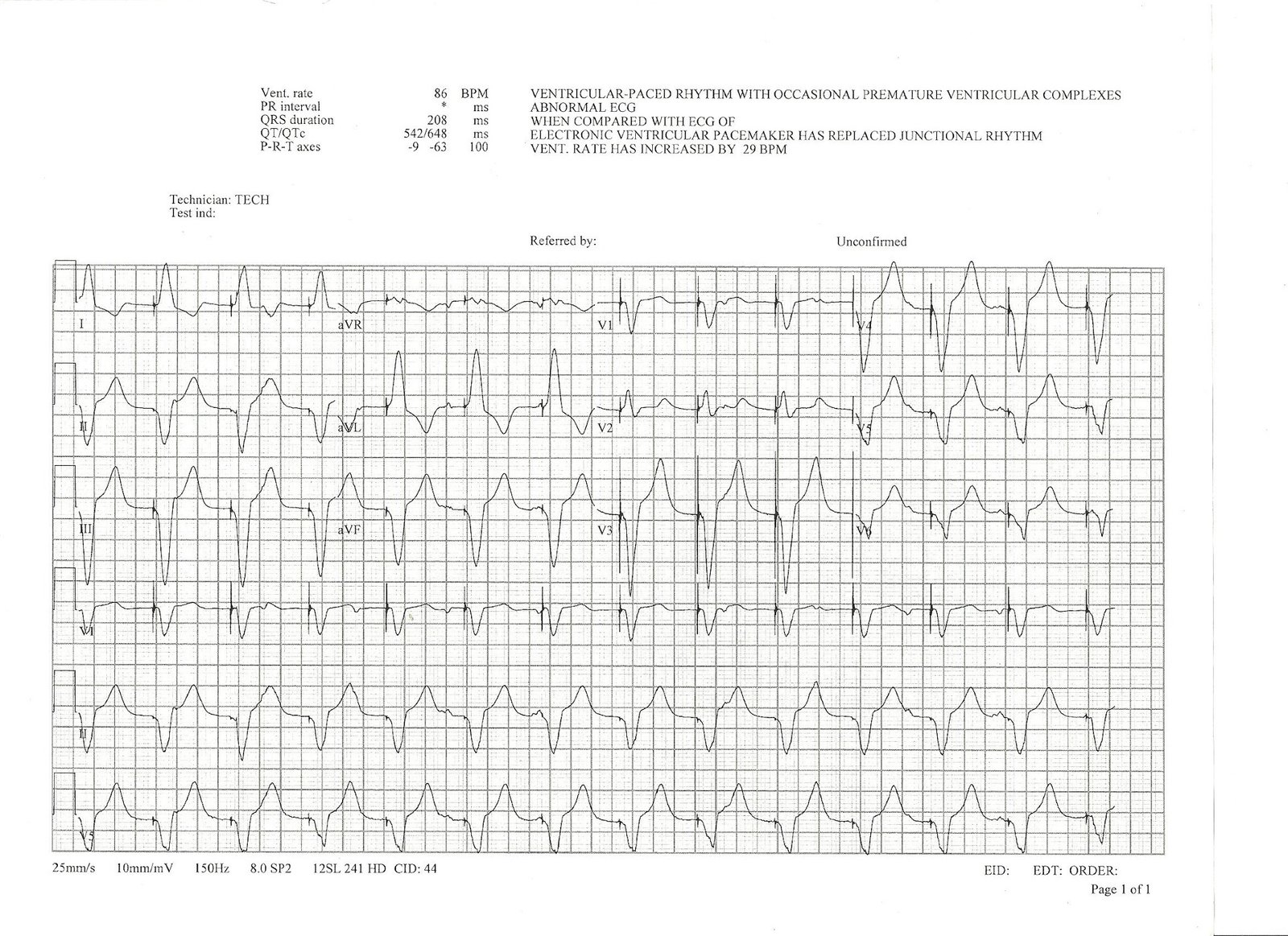
Figure 2.
In the Figure 2 ECG, there is also:
1) Upward concavity in all of V2-V6
2) No inferior ST depression (it is important to note that inferior ST depression is absent in 50% of acute LAD occlusion).
Reference: [Walsh BM. Smith SW. Differences in electrocardiographic Findings
Between Acute Isolated Right Ventricular Myocardial Infarction and Acute
Anterior Myocardial Infarction. JAMA
Internal Med 2016 Dec 1.; 176(12)1875-1876.]
3) no STE of at least 5 mm
4) no T-wave inversion
5) No Q-waves in V2-V4
Thus, the formula may be used in the Figure 2 ECG.