This was sent by an undergraduate (not yet in medical school, but applying now) who works as an ED technician (records all EKGs, helps with procedures, takes vital signs) and who reads this blog regularly.
He also sent me this great case.
Edited by Smith
A
63 year old man with a history of hypertension, hyperlipidemia,
prediabetes, and a family history of CAD developed chest pain, shortness
of breath, and diaphoresis after consuming a large meal at noon.
He
called EMS, who arrived on scene about two hours after the onset of pain
to find him hypertensive at 220 systolic.
He arrived to the ED at 1413,
where his first EKG was taken (BP at this time was about 187/126):
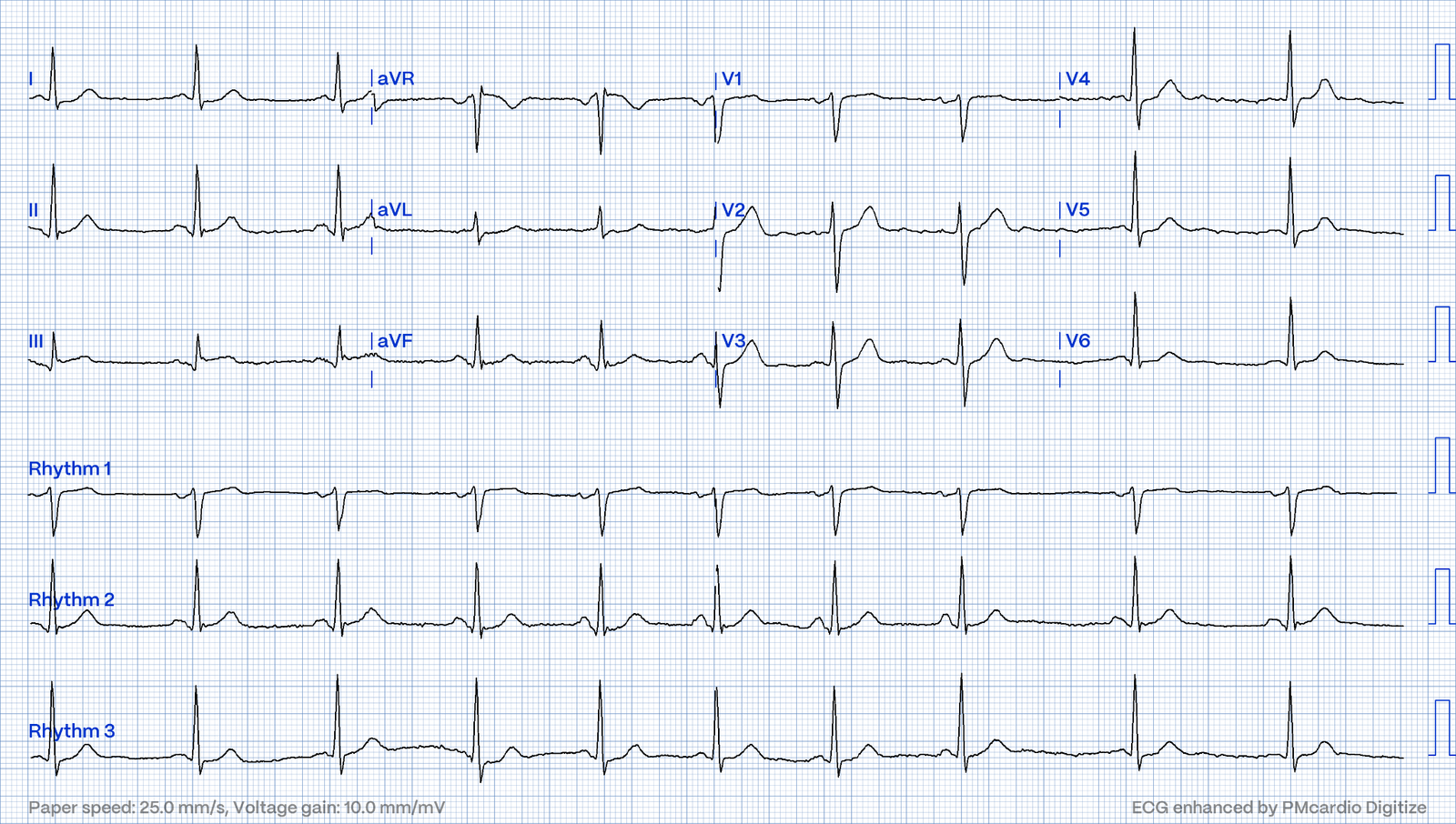
He recorded this ECG at 1413, with a BP of 187/126:
What do you think?
The undergraduate’s analysis:
This
EKG shows J point elevation of about 0.5-1 mm and ST segment
straightening in lead III and reciprocal ST depression of about 0.5mm in
aVL with a straight ST segment and a terminally upright T wave. Lead I
also shows reciprocal ST depression. This EKG is diagnostic of
transmural ischemia of the inferior wall. The conventional computer
algorithm read “nonspecific ST-T wave abnormality”.
Smith: note also the terminal QRS distortion in lead III (absence of S-wave without a prominent J-wave).
The Queen of Hearts disagrees with the conventional algorithm, diagnosing OMI with high confidence:
Click here to sign up for Queen of Hearts Access
Case Continued:
The
EKG was not immediately recognized by the emergency provider, who
ordered a CT scan to rule out aortic dissection at 1419.
The scan came back negative for acute aortic syndrome, but showed a “large amount of ingested material in the stomach” (probably the large meal the patient had before the chest pain began). The scan also showed “scattered coronary artery plaques”.
___________
Smith comment 1: the appropriate management at this point is to lower the blood pressure (lower afterload — afterload increases myocardial oxygen demand, and lowering afterload decreases demand). If it is angina, lowering the BP with IV Nitroglycerine may completely alleviate the pain and the (unseen) ECG ischemia. If you are worried about aortic dissection, you also want the BP to be lowered, though you would do it first with esmolol to decrease the dP/dT (change in pressure over change in time).
Smith comment 2: I frequently see failure to control BP in patients with acute chest pain or acute heart failure. In SCAPE (sympathetic crashing acute pulmonary edema), Emergency providers seem now to regularly give high dose NTG, but when the BP is 170/105 in a patient who is not crashing, we often fail to give something to lower afterload.
______________
Here are some Images:
The
red circle shows the LAD coursing down the anterior interventricular
sulcus. There is an area of dense white in the middle of the circle
consistent with atherosclerosis.
The
green circle here shows a small section of the RCA. The blue circle
shows the LCx. They too have dense white masses consistent with coronary
atherosclerosis.
Case Continued
The
patient was brought back from the CT scanner with continued pain, and
still appeared to be diaphoretic, short of breath, and in distress.
The
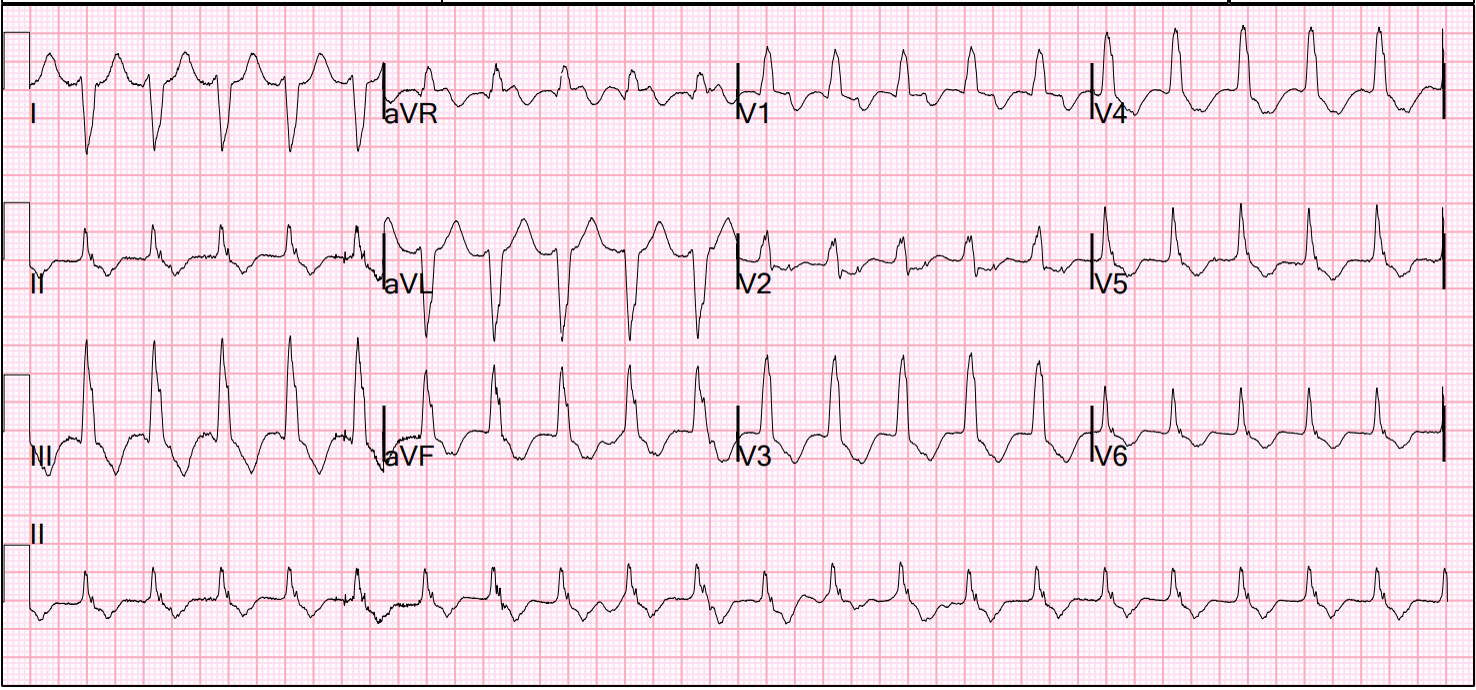
emergency provider ordered another EKG at 1446 (his blood pressure at
this time was about 206/103):
This
EKG shows evolution of continued transmural ischemia of the inferior
wall. The T wave in lead III has increased in size. There is new ST
segment flattening and T wave inflation in II and aVF. The reciprocal
change in aVL has become more pronounced. The T waves in V2 and V3 are
starting to “deflate” suggesting posterior wall involvement.
This time,
the conventional computer algorithm read:
“Normal sinus rhythm, normal
ECG”.
The Queen of Hearts once again diagnoses OMI with high confidence:
Click here to sign up for Queen of Hearts Access
The
ED provider recognized the changes in this EKG and called cardiology
for a STAT consult. The cardiologist recognized that there were EKG
changes, but did not take the patient for emergent catheterization
because the EKG was “not meeting criteria for STEMI”.
At
1502, the first high sensitivity troponin T resulted at 18 ng/L (very
slightly elevated, the URL is 16 ng/L for men in this assay).
The
patient was put on a nitroglycerin drip and his pain improved with his
blood pressure.
At 1554, a third EKG was ordered (At this time, his
blood pressure was around 122/57):
This
EKG shows changes consistent with reperfusion of the inferior wall. The
T waves in leads II and aVF have deflated, and the T wave in lead III
has become terminally negative. The ST depressions in I and aVL have
resolved.
Smith comment: Is the ACS (rupture plaque) with occlusion that is now reperfusing? Or is it a very tight stenosis that does not allow enough flow to perfuse myocardium that has a high oxygen demand from severely elevated BP?
Transmural ischemia (as seen with the OMI findings on ECG) is not very common with demand ischemia, but is possible. The only study I’m aware of that looked at this was mine, in which 4% of Type II MI had New ST Elevation.
____________________________
Amazingly, the Queen of Hearts still diagnoses OMI, although
this time with low confidence:
Case Continued by the Undergraduate:
The
cardiology fellow wrote in their note: “With initial troponin just
minimally elevated and resolution of chest pain as well as EKG changes
with normalization of blood pressure, we have lower suspicion for an
acute ischemic event. However, in light of risk factors for
atherosclerotic disease and dynamic EKG changes today, we will pursue a
CTCA tomorrow for further evaluation of coronaries.
It does appear more
likely that his chest pain was GI in nature (possibly esophageal spasm
and/or GERD) given his large meal preceding onset of chest pain, as well
as CT findings consistent with large amount of ingested material in
stomach.”
Smith: What???!!!
So
the patient was admitted to the hospital with no plan for an angiogram.
Then at 1935 when a 2nd troponin resulted at 211 ng/L, and the
patient received a diagnosis of “NSTEMI.” At 0635 the next day, a third
troponin resulted at 899 ng/L. At 1041 a formal echo showed an EF of 71% and
the note stated that the “basal posterior segment and and basal inferior
segment are abnormal”.
The
cardiology fellow wrote in their note “unclear etiology of troponin
elevation at this time, but hypertensive emergency, underlying CAD with
demand ischemia, or NSTEMI all remain on the differential… In light of
his risk factors, concerning clinical presentation and troponin trend —
we favor coronary angiogram over CTCA at this time.”
Of
course, writing “hypertensive emergency, underlying CAD with demand
ischemia, or NSTEMI all remain on the differential” makes no sense.
Troponin was elevated and no “STEMI” was seen on the EKG, so if it is acute MI, then “NSTEMI” is
the diagnosis (however flawed), not a pathology on the differential. It
is instead most likely that the patient has severe stenosis of the RCA
(or possibly the LCx) and experienced such drastic hypertension that the
demand could not be supplied by a severely stenosed artery, and resulted in findigs of transmural ischemia rather than subendocardial ischemia.
Smith:
After the blood
pressure was controlled with nitroglycerin, the patient’s pain subsided
and the EKG showed reperfusion.
Was this resolution of demand ischemia? Or was it spontaneous lysis of thrombus co-incidental with the lowering of the BP?
Probably the latter.
In any case, the appropriate intervention in this case begins with nitroglycerine, at whatever dose that it takes to lower the BP substantially.
If the pain and ECG findings do not resolve, then the cath lab is indicated.
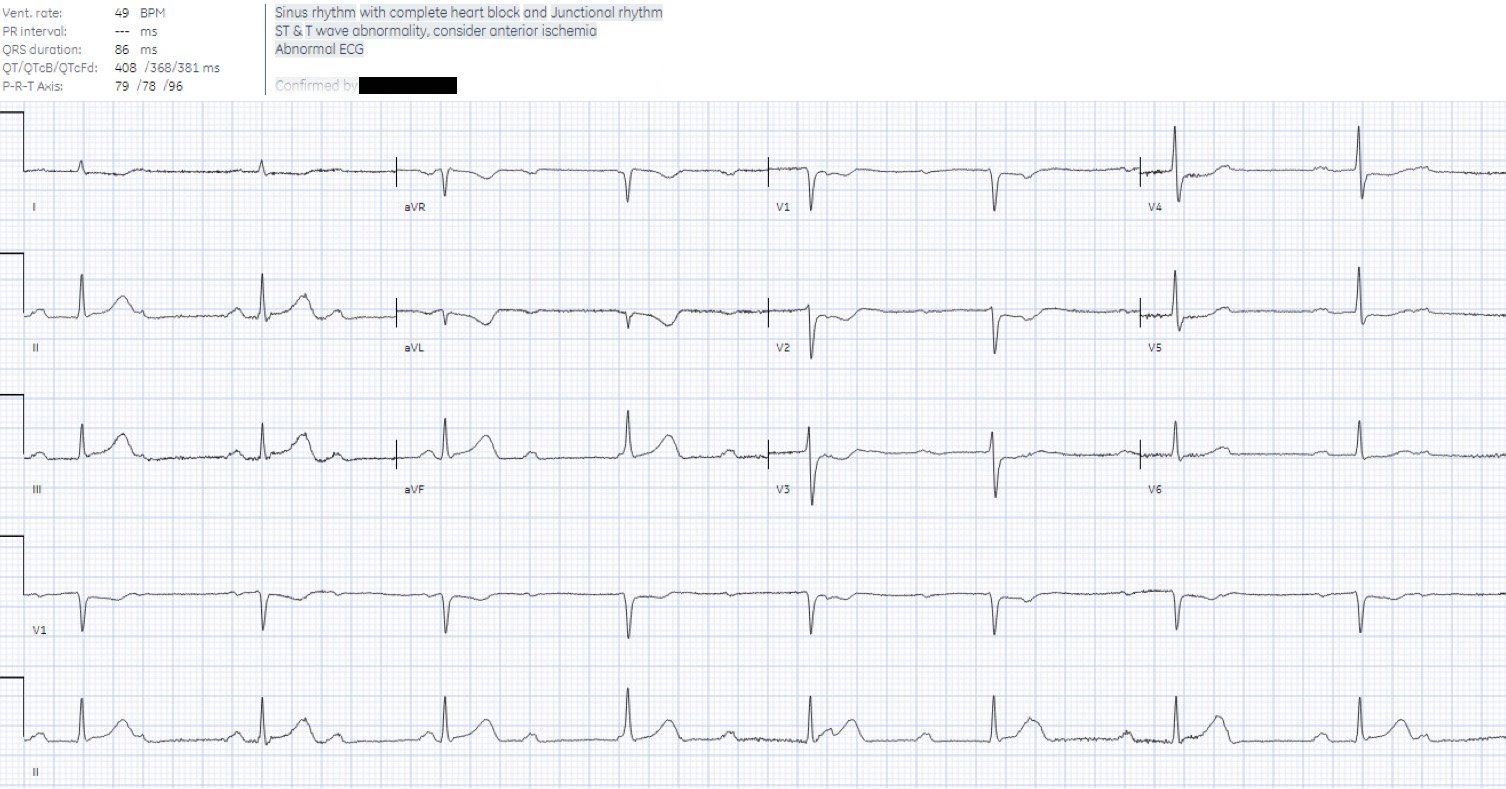
Another EKG was taken at 1304:
This
shows continued reperfusion and the development of large Q waves in
lead III.
The Queen of Hearts now sees no OMI with low confidence:
The
patient did not receive an angiogram on day two of his hospitalization
because the cath lab was too busy. Instead he had an angiogram at 0800
on day 3.
The angiogram showed scattered mild luminal irregularities
of the LAD, the LCx, and the RCA and a 95% distal RCA occlusion in a
right dominant system.
This was a presumed culprit and a stent was placed. Assuming that was indeed a culprit, then this was ACS. And angiographers tell me that it is sometimes difficult to say for certain based on angiogram alone, without intravascular ultrasound or, better yet, optical coherence tomography.
Read more about optical coherence tomography here.
A post-cath EKG was taken:
 This
This
EKG shows inferior Q-waves and T wave inversion in the inferior leads consistent with infarction and reperfusion of the inferior wall. The T waves in the anterior leads have
become a bit “peaked” and symmetrical as well, which is a sign of
reperfusion of the posterior wall.
The
patient re-presented to the ED a few days after his discharge with
syncope. Notably, he had a troponin T drawn at 1,524 ng/L, which is consistent with a large MI. Most STEMI have peak troponin I over 1000 ng/L and most NSTEMI below that level. Of course NSTEMI is a rather worthless diagnosis because it includes both OMI (very large MI) and Non-OMI (much smaller usually)
He also had an echo done which showed
persistent hypokinesis of the basal inferior wall segment and an EF of
60-65%. This suggests that during the time he spent in the hospital
awaiting catheterization, he lost about 5-10% of his ejection fraction, though much of that may recover in the convalescent phase, which takes up to 8 weeks.