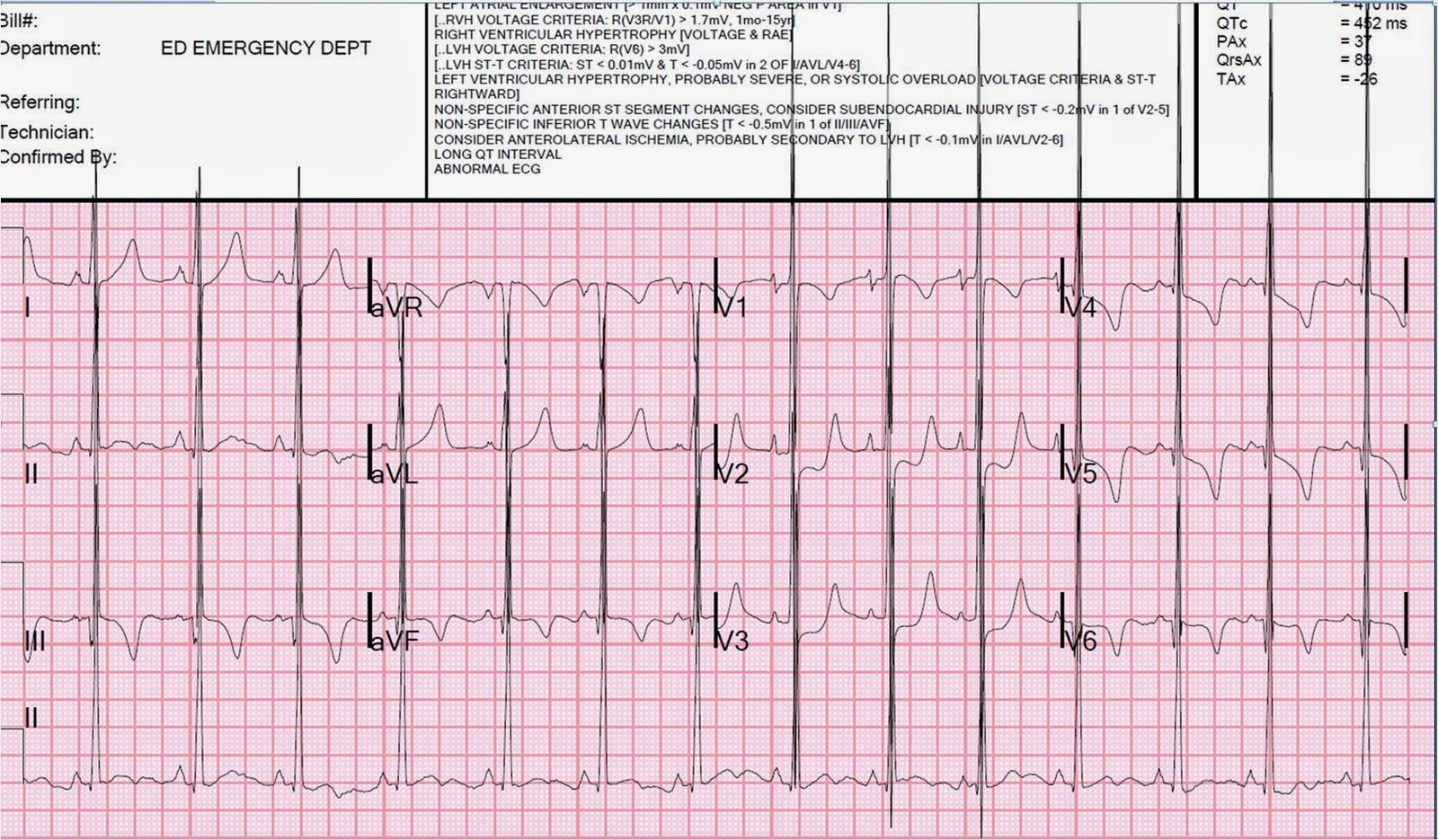
A 41 year old male presented to a clinic with chest pain. Here is the ECG:
 |
|
|
The patient was sent home from the clinic. Days later, the overread by the cardiologist was, appropriately, “ST elevation with hyperacute broad-based T-waves concerning for acute anterior MI.” The clinic physician was notified and the patient was called back to the ED and arrived 4 days later.
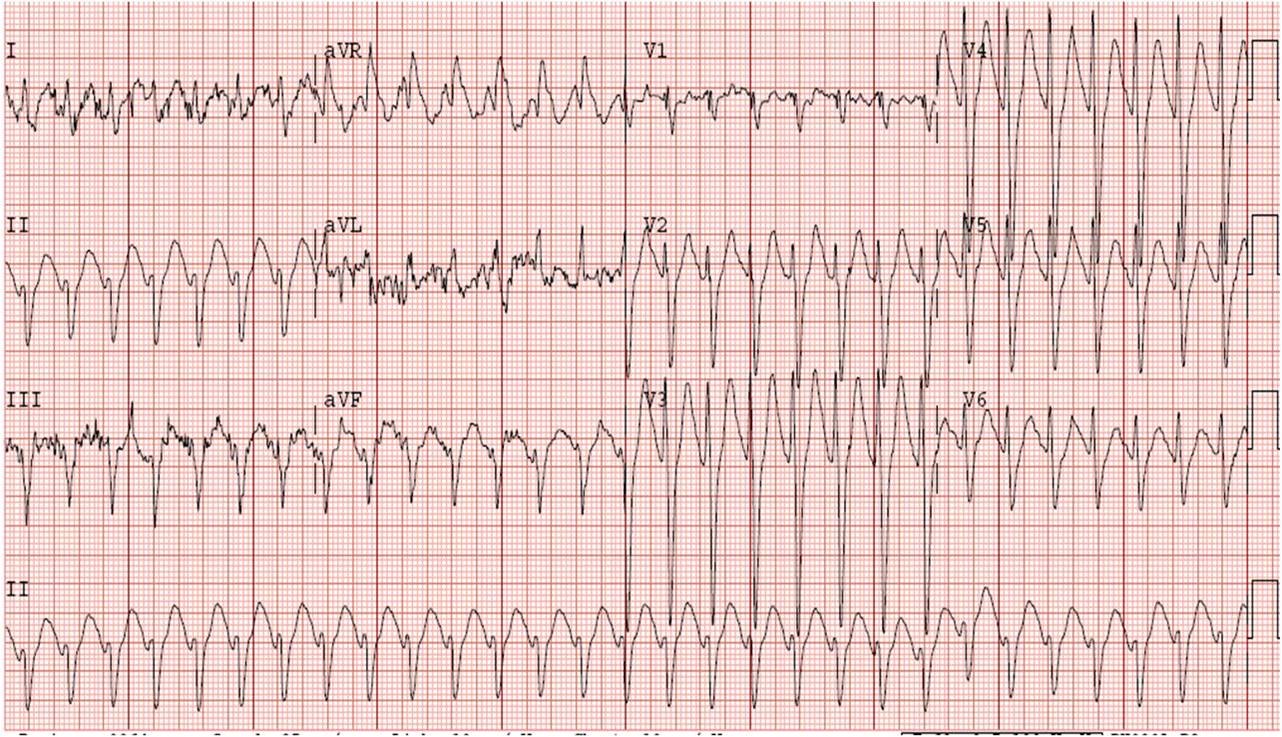
Here was his ED ECG:
 |
||
|
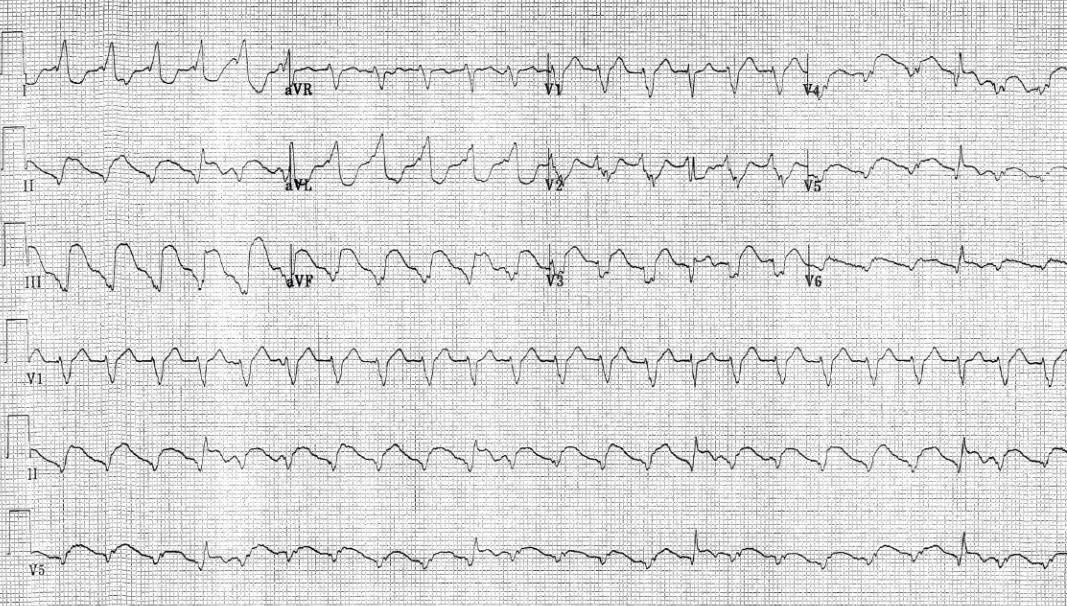
Answer below:
His troponin was normal, as were subsequent serial troponins. An emergent echo was normal.
How does the Smith formula fare on this ECG? (See excel spreadsheet under “rules and equations”at the top of this blog under the heading “The equation for differentiating the ST elevation (STE) of subtle LAD occlusion from early repol”).
Here I use the 3-variable formula. Since this post was written, the 4-variable formula has been derived and validated as more accurate (also under heading above).
The clinicians in the ED calculated the 3-variable value of the first one at 23.31, and the second at 22.8. Both are below the cutoff for anterior STEMI of 23.4.
I calculated them as well:
1. On the first, I get STE60V3= 4 mm, QTc = 398 ms, and R-wave V4 = 16.5 mm.
The calculator comes up with 22.89
2. On the second, I get STE60V3 = 4 mm, QTc = 385 mm, and R-wave V4 = 17 mm.
The calculation comes to 20.98.
Again, both are less than 23.4.
If I saw this patient in the ED, I would be scared by his ECG. But the short QT and the tall R-wave in V4 make it less scary, and thus the equation value is less than 23.4.
4-variable values would be:
ECG 1: QTc = 398 ms, STE60V3 = 4 mm, RAV4 = 16.5, QRSV2 = 19.5.
Value = 17.57 (less than 18.2 is normal)
ECG 2: QTc = 385 ms, STE60V3 = 4 mm, RAV4 = 17, QRSV2 = 17.
Value = 17.145 (less than 18.2 is normal)
Would I then automatically dismiss this and say it is NOT anterior STEMI?
NO! This ECG is scary. The rule is about 90% accurate, but not perfect.
But I would also evaluate the patient more carefully before activating the cath lab. I would probably order (or do myself) an immediate cardiac echo to look for an anterior wall motion abnormality. If none were seen, I would not activate. If an anterior WMA were seen, I would activate the cath lab.