This was sent by an old friend who works at a hospital without PCI capabilities, and far from one that does. So if there is OMI, he gives thrombolytics.
A very elderly patient with previous EF of 60% complained of shortness of breath for 2 weeks, with pleuritic chest pain. There was no pain on arrival. But the pain recurred while in the ED.
His BP was 90 systolic.
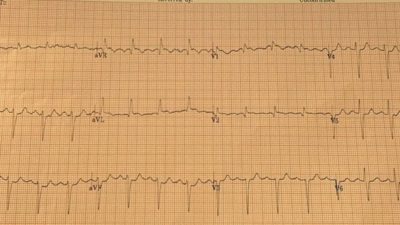
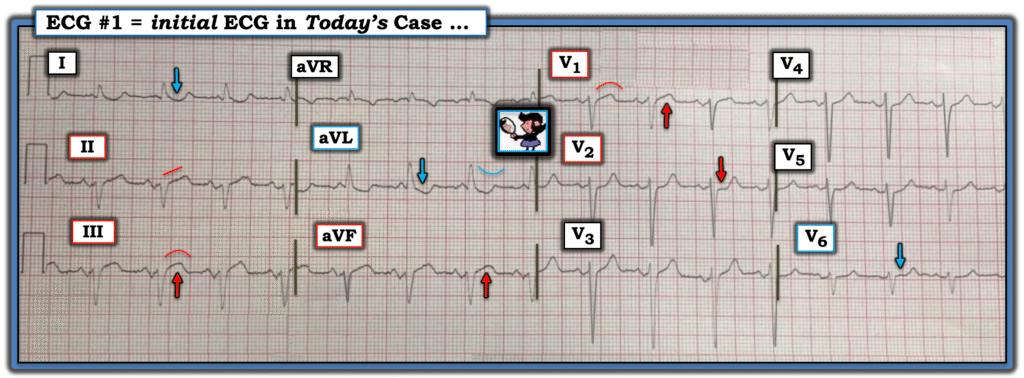
He recorded an initial ECG:
What do you think? Is it “Nonspecific ST abnormality, as the conventional computer algorithm claims?”
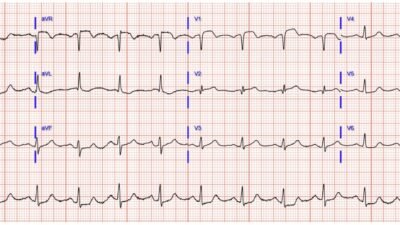
My friend thought there was inferior OMI. He applied the PMCardio Queen of Hearts:
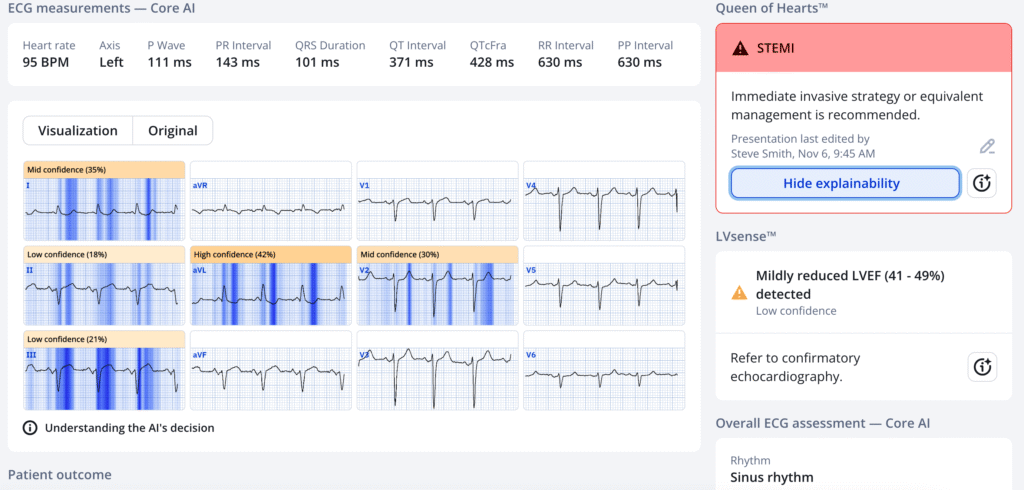
The model output was 0.96, which is nearly 100% certain. (That is found by clicking on the small encircled “i” next to “hide explainability”.)
PMcardio for Individuals now includes the latest Queen of Hearts model, AI explainability (blue heatmaps), and %LV Ejection Fraction. Download now for iOS or Android: https://individuals.pmcardio.com/app/promo?code=DRSMITH20. As a member of our community, you can use the code DRSMITH20 to get an exclusive 20% off your first year of the annual subscription. Disclaimer: PMcardio is CE-certified for marketing in the European Union and the United Kingdom. PMcardio technology has not yet been cleared by the US Food and Drug Administration (FDA) for clinical use in the USA.
So the Queen agrees.
Smith interpretation: Diagnostic of inferor and RV OMI. Inferior STE and hyperacute T-waves, with reciprocally inverted hyperacute T-wave in aVL. There is minimal ST depression in lead V2 (where there should be some STE!), thus highly suggestive of posterior OMI.
Why is there hypotension??
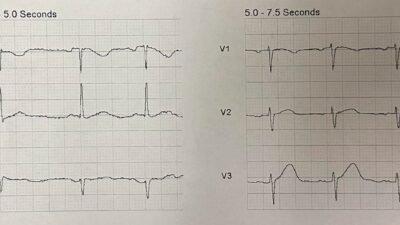
—–Lead V1: There is STE and hyperacute T-wave in V1. We showed that this is ESPECIALLY significant in the setting of the STD in V2, because the posterior wall should be attenuating any STE in V1. This STE in V1 is all but diagnostic of right ventricular OMI (RVMI). This will cause hypotension.
Why does the Queen not highlight lead V1? Answer: we have never coded, or annotated, “RVMI” for the Queen. Every case of RVMI has been in the context of inferior OMI. So every case of inferior OMI has been annotated only as OMI, and only a fraction of those have had STE or HATW in V1. So she does not correlate STE in V1 with OMI, UNLESS there is STD in V5-6 (which is precordial swirl) from LAD OMI. In any case: she recognizes OMI and that is the only output she is allowed to give and the only really critical output.
It is very common for the very elderly to have atypical symptoms of acute MI. Without chest pain, he was not certain enough to act. I think I would have been convinced by the ECG and the Queen’s certainty, but I was not there.
If the question was “Cath Lab activations?”, then the answer would be an unequivocal “YES” because the risk of an angiogram is negligible. But the risks of thrombolytics are real.
Then the first troponin I returned very high at 14 ng/mL (4th generation, not high sensitivity, thus equivalent to 14,000 ng/L).
My friend gave thrombolytics. Then called the cardiologist at the referral center. Response? “Cardiology not impressed with ECG.”
My response: “Definitely an inferior OMI. Nice work! Hardly any cardiologists understand ECGs like this“
There were no subsequent ECGs. The 2nd troponin was lower at 12 ng/mL. The ECG is shows high “Acuteness,” so although there was subacute infarction with falling troponin, the recurrent chest pain and hyperacute T-wave implies re-occlusion.
Follow up:
“Cardiology did not take my guy right to cath. They are concerned he won’t tolerate lying flat, echo shows dilated RV but good LV function so they want to rule out PE first and cath tomorrow. Pain gone now and trops down trending”
Smith: The RV is dilated because of right ventricular MI (RVMI)!! This is clearly not a pulmonary embolism.
Next day angiography showed a 90% proximal RCA culprit that was stented. The RCA was reperfused, almost certainly due to the thrombolytics.
Learning Points:
- Trust the Queen, not the cardiologist.
- Thrombolytics are beneficial in STEMI(-)OMI as long as the clinical and ECG findings are specific for OMI.
- Any amount of STE in V1 in the presence of inferior OMI implies right ventricularl MI (RVMI). RVMI causes poor RV output and hypotension, and is associated with high mortality if not reperfused. It is caused by proximal RCA occlusion (proximal to the RV marginal branch). Not all proximal occlusions cause RVMI because most patients have collaterals to the RV from the LAD.
- See our publication on Bayesian analysis of ACS (pretest probability and post-test probability, how to incorporate all info to make a decision: (Full text)
- Here are many more cases of RVMI.
- When is it too late for thrombolytics? See here for an exhaustinve post on “Acuteness.” In this case, there are hyperacute T-waves and no QS-waves, so there is sufficient “acuteness” for thrombolysis.
= = =
======================================
MY Comment, by KEN GRAUER, MD (11/8/2025):
Today’s case illustrates the slightly different decision-making process when a patient with new atypical symptoms (ie, a 2-week history of dyspnea with pleuritic chest pain) presents for emergency care.
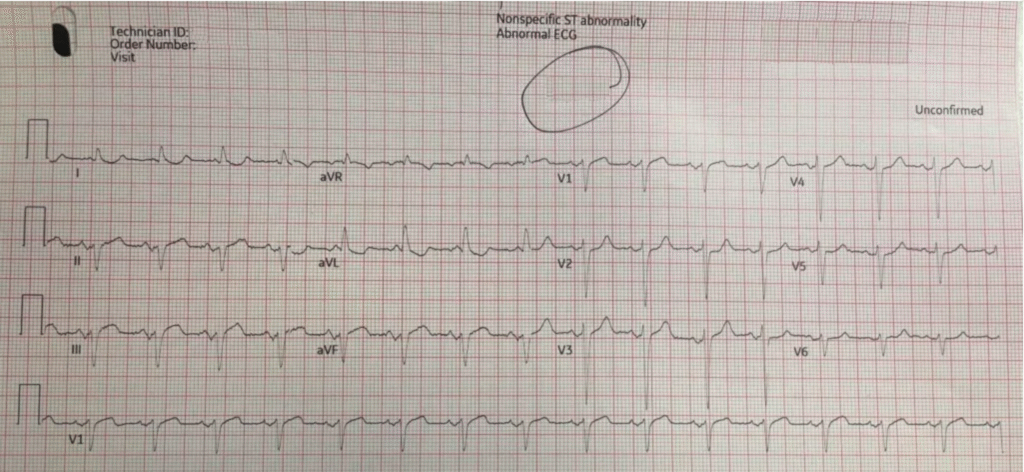
- For clarity in Figure-1 — I’ve labeled today’s initial ECG.
- There are 2 parts to my thoughts: i) What I would do to confirm the diagnosis; — and, ii) What I’d add to the astute interpretation of the initial ECG by the clinician contributing today’s case.
= = =
What I’d Do to Confirm the Diagnosis:
Assessment of today’s case is made challenging, not only by the atypical nature of this patient’s symptoms — but because symptoms occurred over a 2-week period — and the patient was without chest pain on arrival in the ED.
- Finding a previous ECG on this patient would be invaluable for confirming which findings on ECG #1 were “new”.
- Recurrence of pain while in the ED — may prove invaluable for assessing if acute ischemia is ongoing. Although I was suspicious of an acute ongoing event on seeing ECG #1 — I was not certain of this given the 2 week history of shortness of breath with “pleuritic” CP (Chest Pain) as the symptoms that prompted this ED visit.
- That said — given the change in symptoms during observation of the patient in the ED — immediately repeating the ECG (as well as doing an Echo at the bedside during symptoms to look for a localized wall motion abnormality) — might be all that is needed to remove any doubt about an acute evolving process.
- Direct correlation between the presence (and relative severity) of CP and each serial ECG that is done — will often facilitate clinical ECG interpretation (as well as determining if the “culprit” vessel is now open or closed — with reclosure suggested if ST elevation correlates with pain recurrence).
- Realization that a large infarction has occurred over the previous 2 weeks (evident from the very high initial Troponin) — in association with an ongoing change in symptoms (return of CP in the ED) — in association with “dynamic” ST-T wave changes that might be seen on immediately repeating the ECG — would confirm the indication for prompt cath now (rather than the risk inherent in delaying cath until the next morning in a patient with acute reocclusion of the “culprit” artery) — not to mention that the time period for most of the potential benefit that might accrue from timely PCI will be long past by the following morning.
= = =
Today’s Initial ECG:
My thoughts on today’s initial ECG were the following:
- The rhythm is sinus at the fairly rapid rate of 90/minute. The QRS appears slightly widened at 0.10-0.11 second (best seen in the rS complexes in the inferior leads) — with LAHB most likely accounting for this slight QRS widening. There is no chamber enlargement.
- There is poor R wave progression with transition to a dominant R wave never occurring in the chest leads (ie, QRS amplitude decreases in the lateral chest leads — with loss of R wave by lead V6). This may or may not be relevant to today’s clinical presentation (vs a longstanding finding in this older patient).
- My “eye” was initially drawn to the coved ST elevation in the inferior leads (with ST segment straightening in lead II) — with a mirror-image opposite ST-T wave picture in lead aVL (and to a lesser extent in lead I). I was initially uncertain if these limb lead changes were acute or subacute (given the 2-week history of dyspnea) — or possibly even of longer duration.
- I thought the KEY to interpretation of the ECG in Figure-1 — was the definitely abnormal appearance in leads V1 and V2. The ST segment coving with disproportionate ST elevation in lead V1 (given tiny size of the S wave in lead V1) — is clearly abnormal in this lead.
- As per Dr. Smith — we instantly know that the ST-T wave in lead V1 is abnormal — because instead of seeing the normal, slightly elevated upsloping ST segment that is expected in lead V2 — we see ST segment flattening and slight depression in this lead (RED arrow in lead V2). In this patient with new symptoms and the above-described limb lead findings — this contrasting picture of lead V1 ST coving and elevation, but lead V2 ST flattening with depression — has to be assumed due to acute infero-postero OMI with acute RV involvement until proven otherwise.
- Lead V1 is a right-sided lead — and in Figure-1, it shows ST elevation from RV MI that attenuates (opposes) the ST depression that otherwise would have been much greater in leads V2,V3 from the simultaneously occurring posterior OMI.
- Definitive diagnosis of acute RV MI would have been forthcoming by immediately obtaining a right-sided ECG. This would have explained this elderly patient’s acute dyspnea and “inability to lie flat” long before the next morning.
= = =
Figure-1: I’ve labeled today’s initial ECG.
= = =
= = =