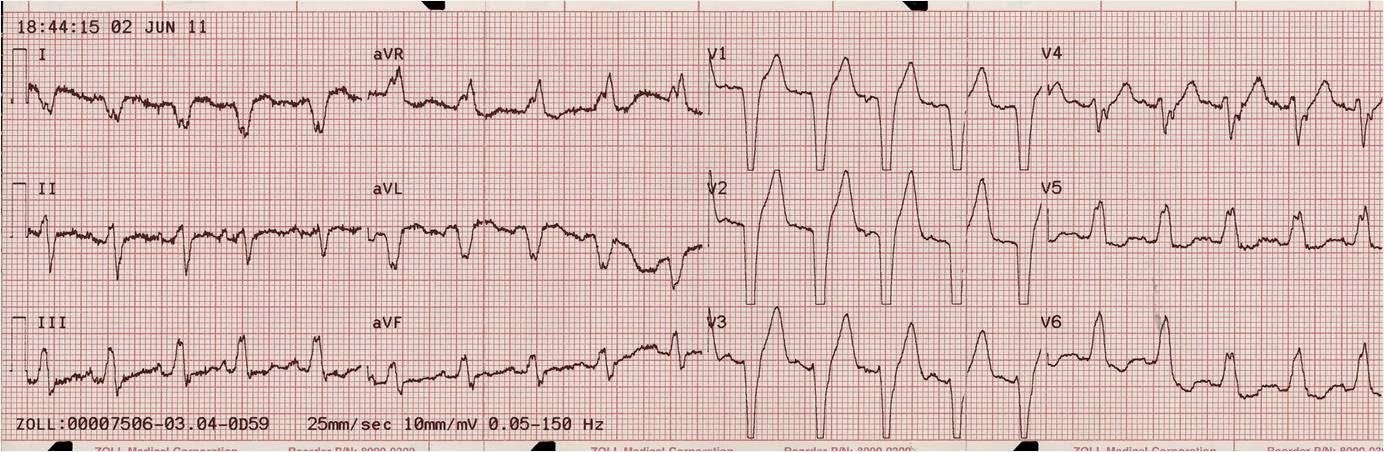
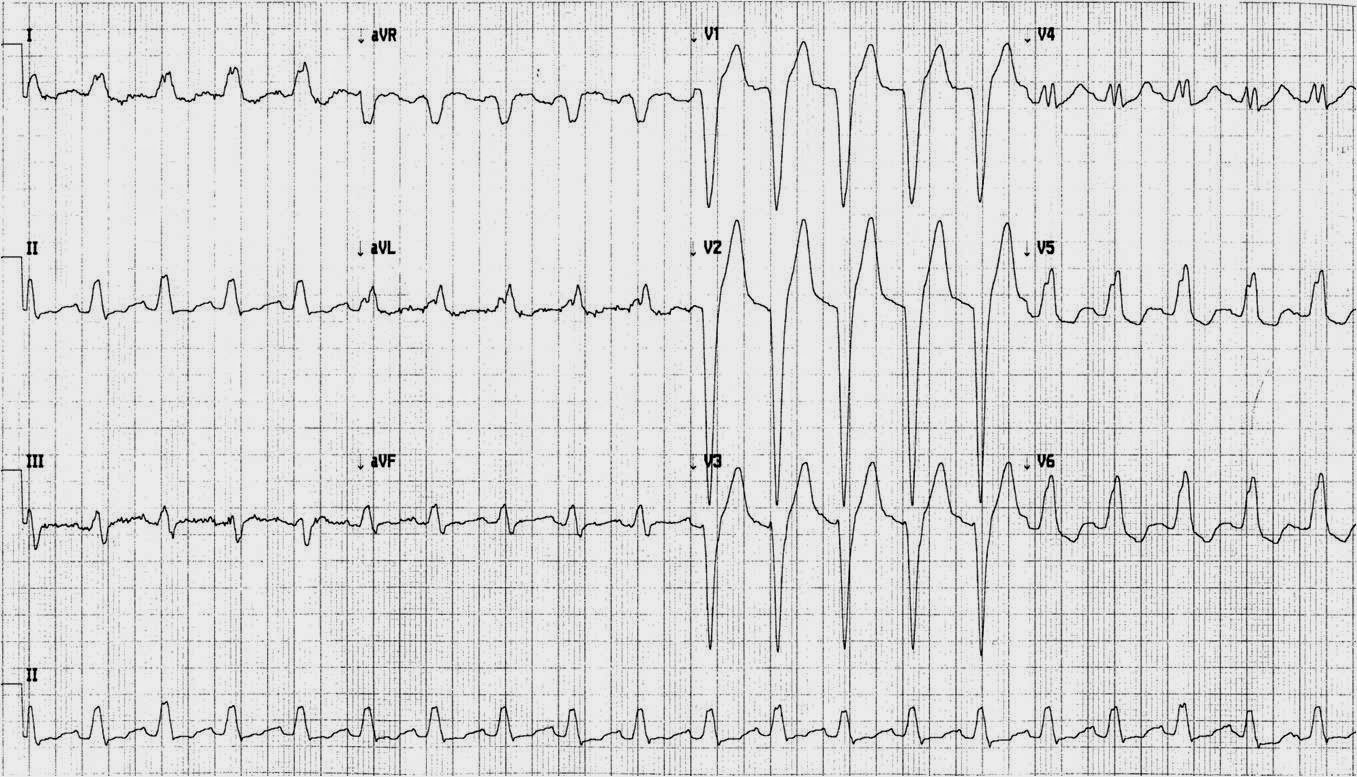
A 59 year old man with no cardiac history was at work when he developed very typical substernal chest pressure. He went to a clinic across the street and had this ECG recorded:
 |
|
|
To learn about appropriate and excessive discordance, please see this post:
https://drsmithsecgblog.com/2011/05/lbbb-is-there-stemi.html
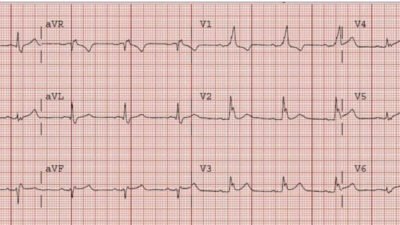
911 was called, the medics arrived, and recorded this ECG:
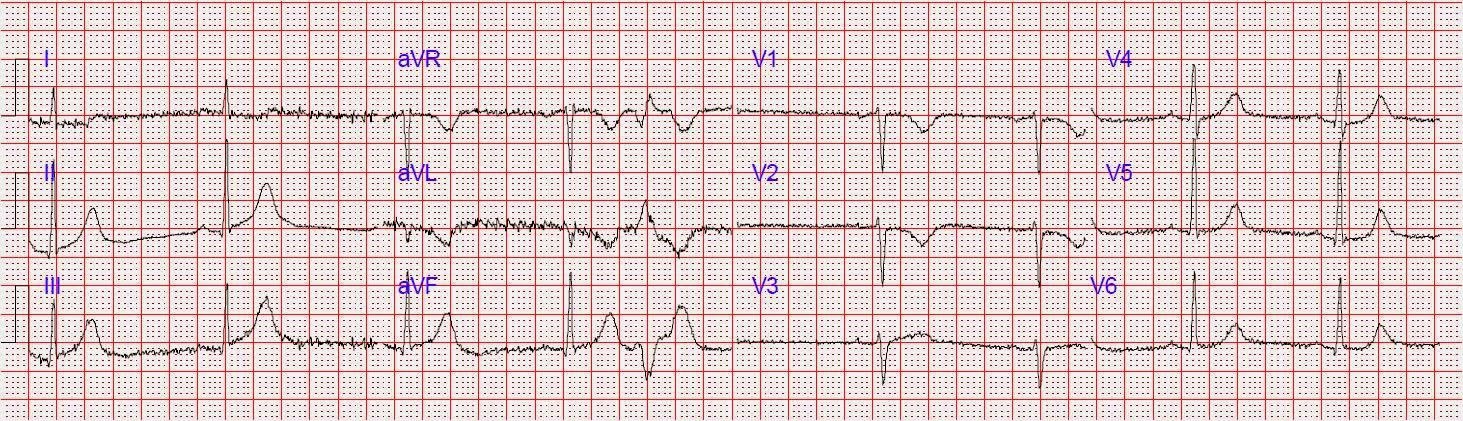
The patient arrived in the ED and had this ECG:
 |
|
|
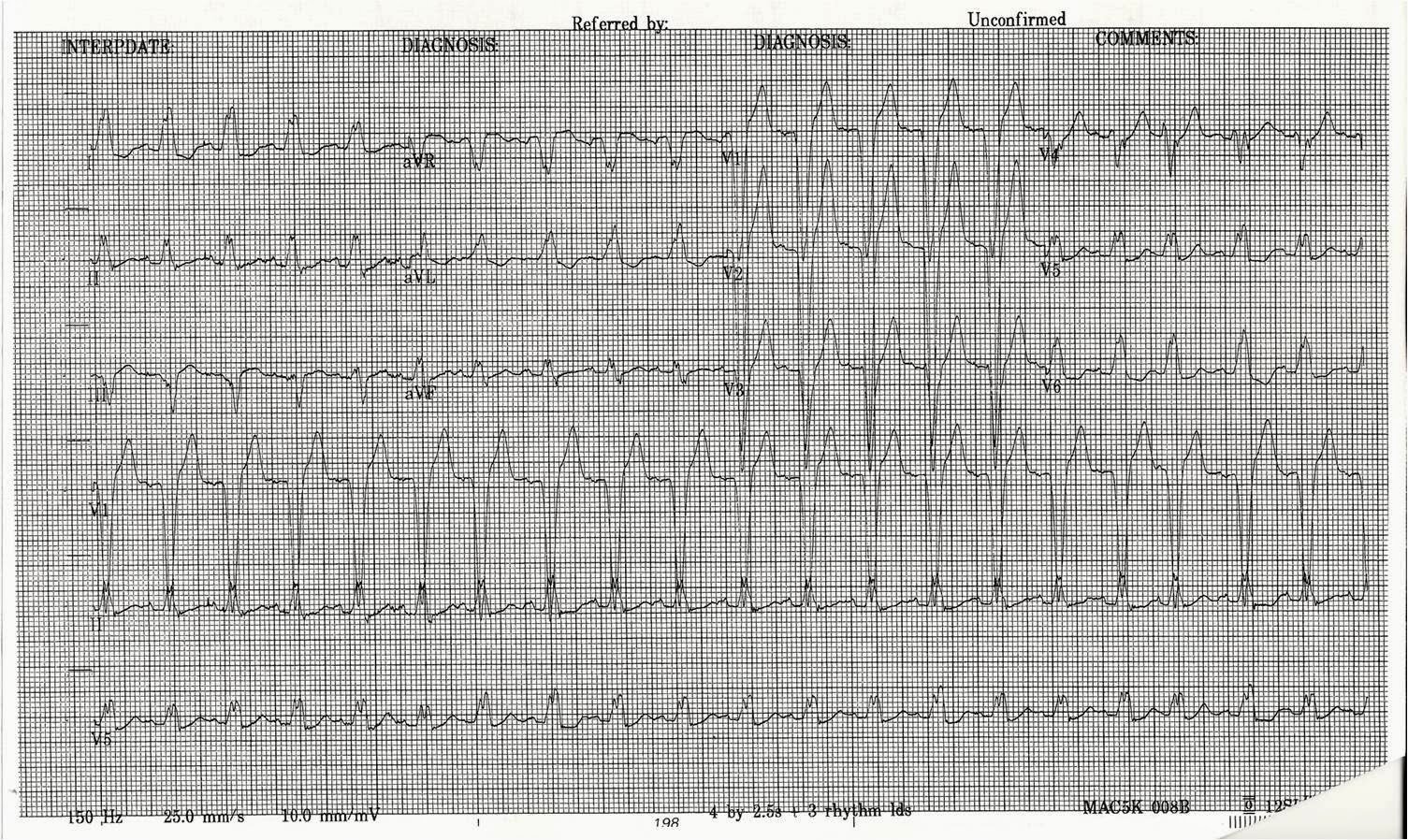
The following ECG was recorded later:
 |
|
|
Is this an anterior STEMI with LBBB? Did the occlusion reperfuse, resolving the LBBB and leaving the patient with reperfusion T-waves (Wellens’ syndrome)?
He was taken to the cath lab. All coronaries were completely normal. All troponins were undetectable.
Explanation:
The patient had a worrisome history: 59 yo with significant substernal chest pressure, so his pretest probability of MI (and even of STEMI) is reasonably high. However, he had a left bundle brach block with normal appropriate discordance on 3 EKGs. Only 5-13% of patients with chest pain and LBBB have MI; many fewer have coronary occlusion. Additionally, appropriate discordance is common in NonSTEMI, but very unusual in coronary occlusion (STEMI).
Moreover, and importantly, there was sinus tach. Whenever you see tachycardia with bundle branch block, you should suspect that it is rate related BBB. Indeed, once the heart rate came down, the BBB resolved.
After resolution, there was T-wave inversion in V1-V3, highly suggestive of ischemia. There are features of the T-wave inversion, however, which argue against ischemia. First, as I have pointed out in posts on pulmonary embolism (see links), T-wave inversion of anterior infarction (Wellens’ syndrome) almost always has an upright T-wave in lead III. Also, anterior ischemia is unlikely to spare lead V4 as in this case.
https://drsmithsecgblog.com/2011/03/chest-pain-sob-anterior-t-wave.html
https://drsmithsecgblog.com/2010/03/anterior-t-wave-inversion-due-to.html
Cardiac Memory
There is another more likely explanation of this T-wave inversion: “Cardiac Memory.” Cardiac Memory (CM) has been described for a couple decades. It is most common after termination of pacing and other etiologies of abnormal depolarization such as Left Bundle Branch Block. After resolution of the abnormal depolarization, there may be transiently inverted T-waves that last for hours to days (these T-waves are the heart’s “memory” of the previous abnormal conduction). This phenomenon is poorly understood, but involves “transient electrical remodeling.”
http://www.heartrhythmjournal.com/article/S1547-5271%2807%2900801-6/abstract
Shvilkin et al. described the way to differentiate CM from ischemia:
http://circ.ahajournals.org/cgi/content/full/111/8/969
In short, the combination of:
(1) positive TaVL (as in this case) and
(2) positive or isoelectric T-wave in lead I (as in this case) and
(3) maximal precordial T-wave inversion greater than the T-wave inversion in lead III (as here: maximal precordial T inversion is in lead V2, at 4.5 mm, and T-wave inversion in lead III is only 2.5 mm) was
92% sensitive and 100% specific for CM, discriminating it from ischemic precordial T-Wave Inversion.
Thus, the very well informed physician could differentiate these ECGs from those of an LBBB patient with MI:
1) no concordance
2) no excessive discordance
3) LBBB with tachycardia, probably rate related
4) subsequent T wave inversion that, according to Shvilkin et al., is diagnostic of cardiac memory. It is NOT Wellens’ syndrome.