Written by Emily Dawra, one of our superb EM G3 residents, with a few edits by Smith.
Case: A patient presented to the emergency department from a clinic for a “STEMI activation”. He had been having stuttering exertional chest pain and exercise intolerance for nearly 1 week. However, he had been out of the country and told us that he “didn’t want to go to the hospital there,” so he waited until his convenient appointment with his primary doctor in clinic in Minnesota. His physician astutely assessed the concerning history, obtained the initial ECG, which he recognized as very worrisome, and so transferred him to the ED after giving 324mg of aspirin.
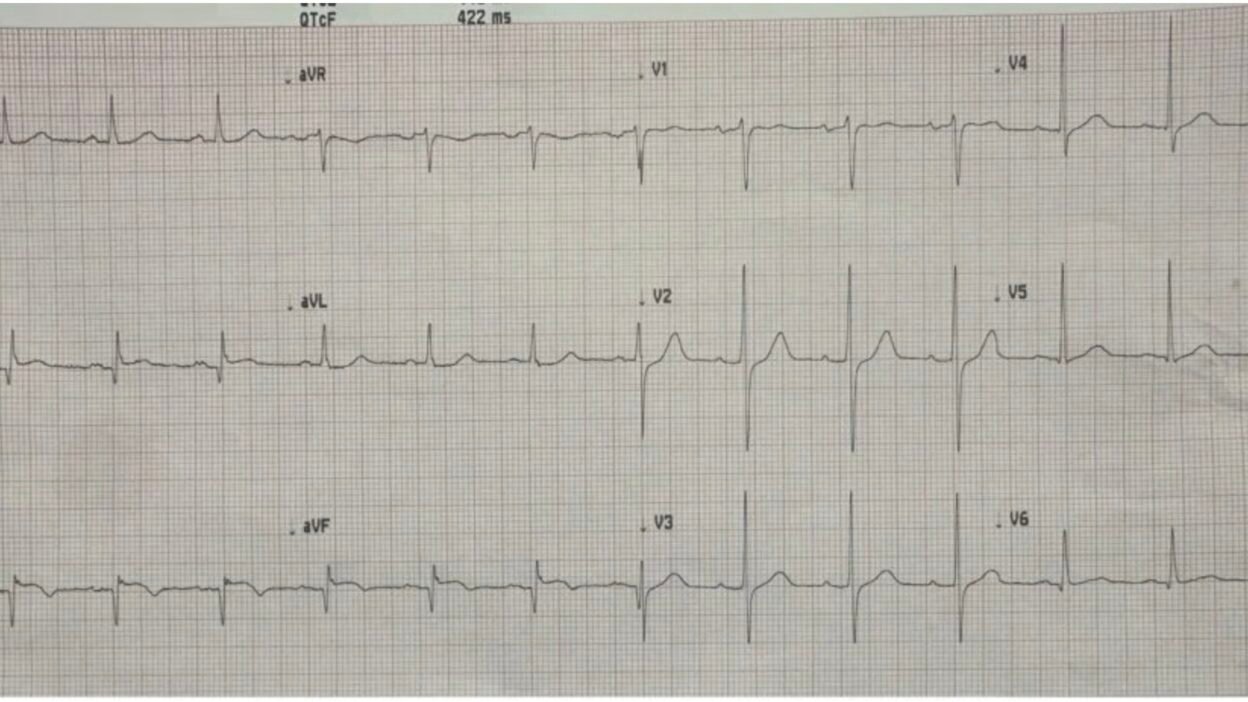
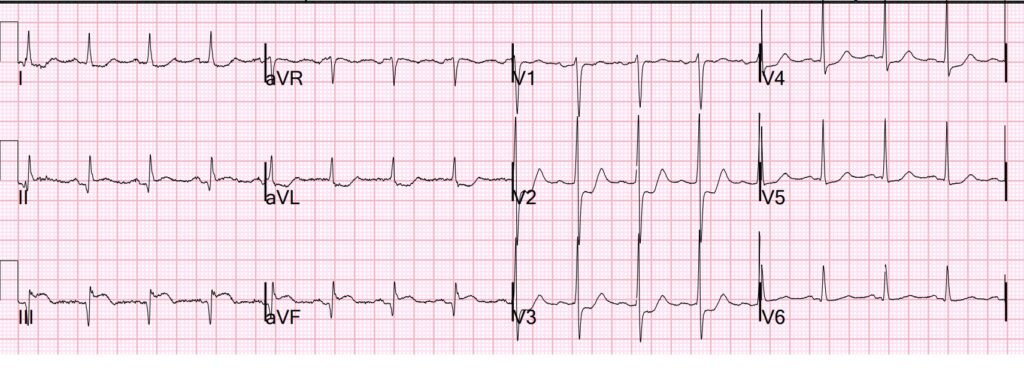
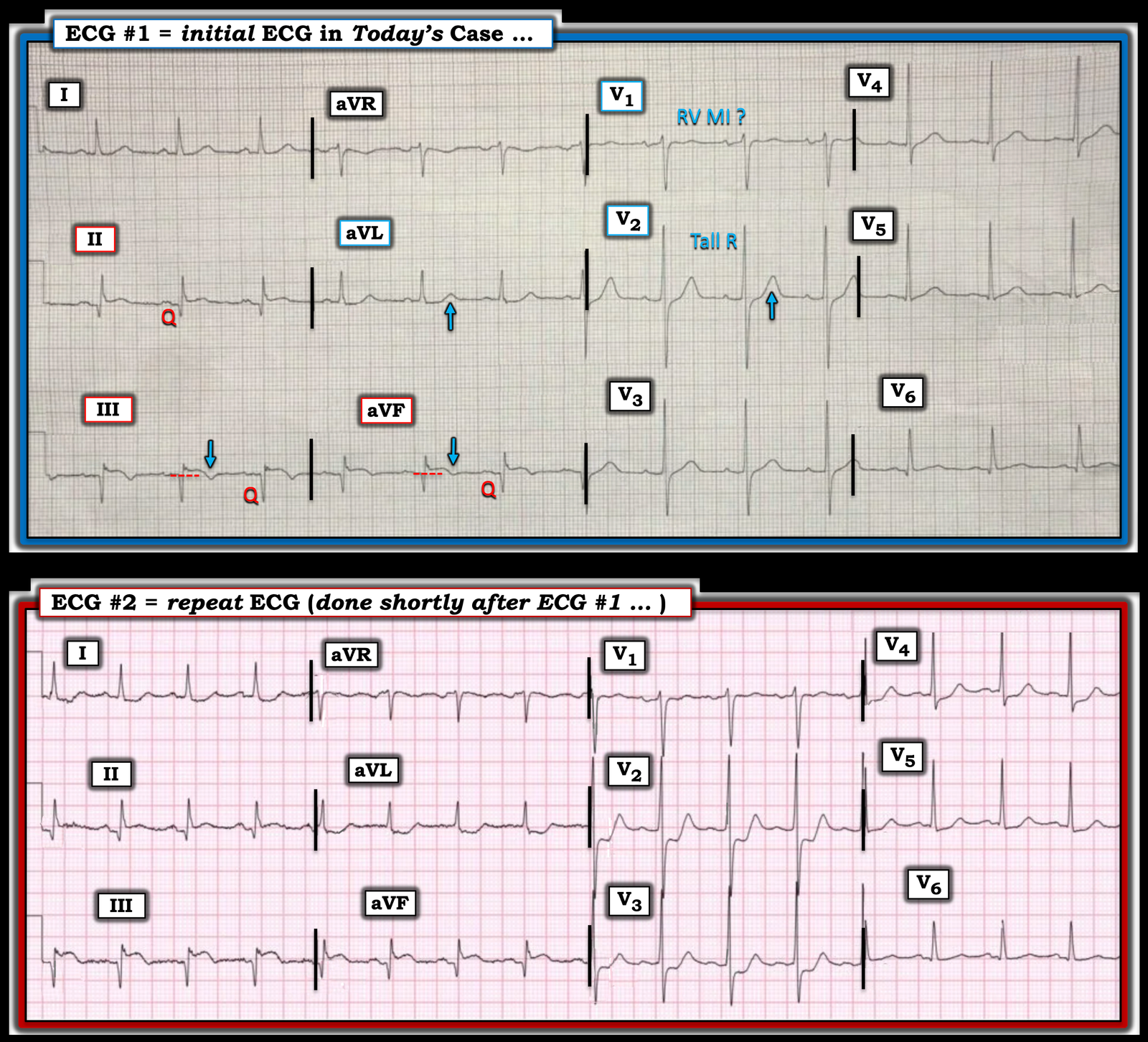
Here is that clinic ECG, recorded while pain-free:
What do you think?
This is diagnostic of acute vs. subacute OMI, almost certainly reperfused. There is inferior ST elevation (II, III, aVF) and anterior precordial ST depression (V2, V3), diagnostic of inferior-posterior occlusive event. But also note the T-wave inversions inferiorly, which strongly suggest some element of reperfusion, especially in the context of resolved chest pain (pain free). There are also well-formed Q-waves that suggest that the infarct was subacute (several hours old) at the time it reperfused.
Here is the PMCardio Queen of Hearts interpretation:
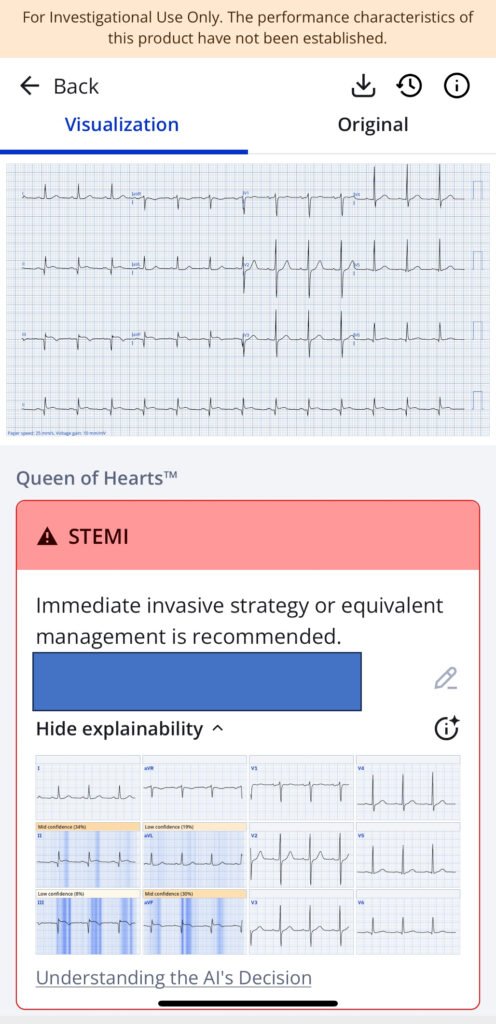
PMCardio for Individuals now includes the latest Queen of Hearts model, AI explainability (blue heatmaps), and %LV Ejection Fraction. Download now for iOS or Android: https://individuals.pmcardio.com/app/promo?code=DRSMITH20. As a member of our community, you can use the code DRSMITH20 to get an exclusive 20% off your first year of the annual subscription. Disclaimer: PMcardio is CE-certified for marketing in the European Union and the United Kingdom. PMcardio technology has not yet been cleared by the US Food and Drug Administration (FDA) for clinical use in the USA.
_______________________________
Smith: I am surprised that she does not say “Repefused OMI”.
The cardiology fellow was in the ED by the time Dr. Smith arrived; he looked at the ECG and said “This is a reperfused OMI. The patient should go to the cath lab now because he is at very high risk of re-occlusion at any moment.”
The fellow talked with the interventionalist, who said: “This is an NSTEMI and the patient can wait for intervention.”
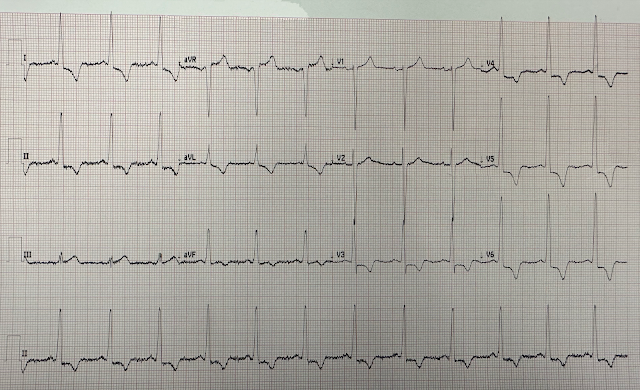
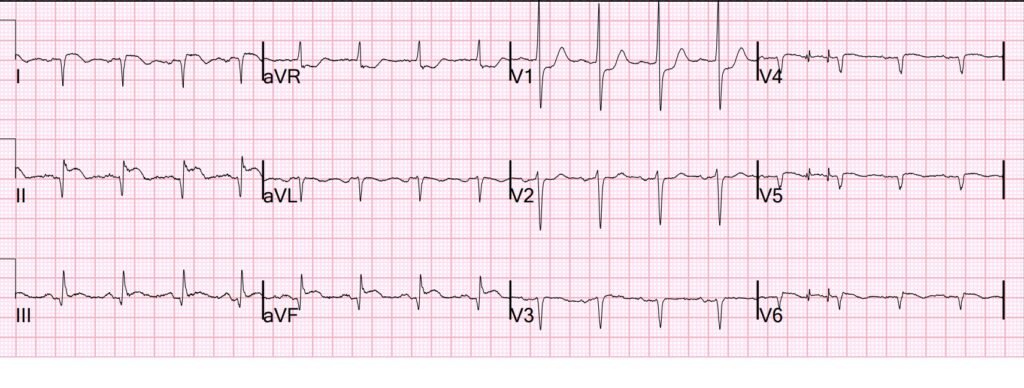
At this moment, while the patient was still completely pain free, we recorded another ECG:
Now there is significant worsening of ST elevation inferiorly and of the ST depression in the precordial leads. Accordingly, there is increased reciprocal ST depression in aVL. This is now clearly a hyperacute Occlusion MI.
The artery is actively re-occluding without any pain!
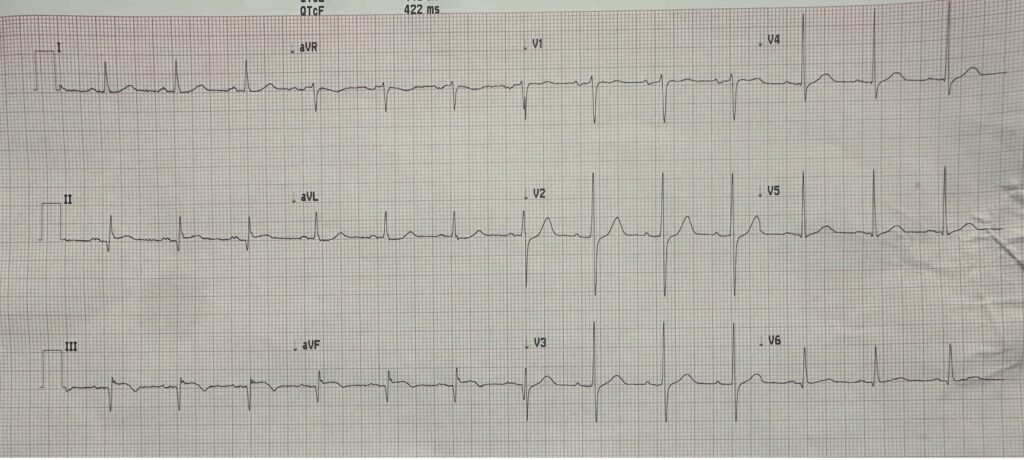
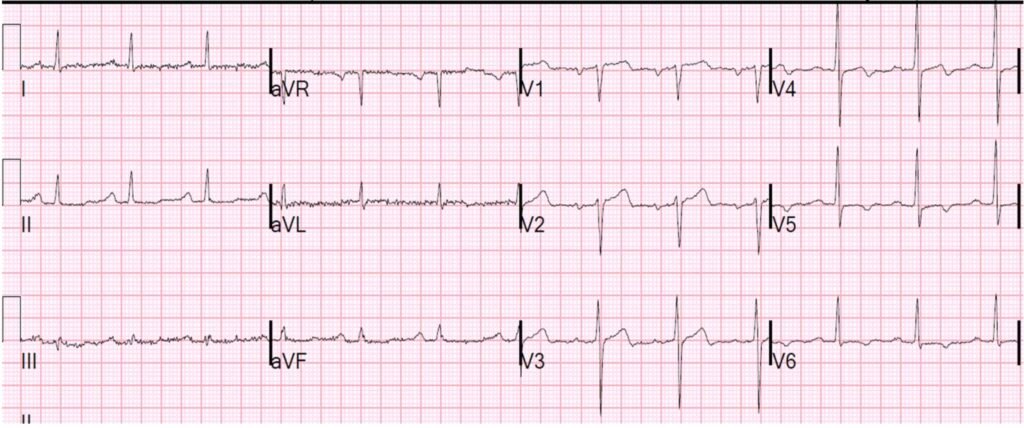
5 minutes later we record a right sided ECG:
Limb leads are not placed differently in a right sided ECG (only precordial leads are reversed). The limb leads now show pseudonormalization of the inferior T-waves [re-occlusion results in the previously inverted reperfusion T-waves becoming upright (“pseudonormalizing”)].
V4-6 are now V4R, V5R, V6R on the right chest.
Comment on right sided ECGs: all leads for Right sided ECG are reversed: [V1 = V2R to the right of the sternum; V2 = V2R to the left of the sternum, etc.] Q-waves are normal in right chest leads because they are opposite of the electrically dominant LV. Note the slight ST elevation in V4R, V5R, and V6R highly suggestive of RV infarction.
With the progression of ECG changes and concerning history, even without chest pain at this moment, patient was fortunately taken to the catheterization lab.
Angiogram:
90% distal LM
90% ostial proximal LAD
Subtotal occlusion of LADD1 and LADD2
Subtotal occlusion of OM-1
70-80% mid and distal RCA
OM-1 was the probable culprit. Since the proximal RCA was not involved, the ST Elevation in right leads is probably a false positive.
Echo:
Estimated LV ejection fraction lower limits of normal-51%. Regional wall motion abnormalities : mid-apical inferior and inferior. Septal walls are dyskinetic, and likely aneurysmal. Normal right ventricular size and function. (This verifies that RV MI is very unlikely).
Management
Due to severe multi-vessel disease including proximal LAD. A temporizing intra-aortic balloon pump was placed while a CABG was planned for the next day to augment coronary perfusion pressure and allow for safer induction of anesthesia the next day.
No percutaneous intervention was done on the OM1 culprit. We see this frequently: when the patient needs CABG, no intervention is done on the culprit, even if there is poor flow. I’m not sure why this is.
First hs troponin I returned at 3443 ng/L. Next trop was not measured until 6 hours later and was 2987 ng/L. I suspect it rose a bit and then fell, the peak occurring sometime in the interval.
Emily’s Reminders & Take-Aways:
- Do not let the resolution of chest pain alone dissuade you from activating Cath Lab–the ECG is crucial! Especially when ECG is concerning or prior history is highly suggestive of coronary occlusion.
- It’s estimated that over 20% of heart attacks are silent [1]. Although a “silent MI” is one that is not discovered until a later physician visit, it highlights the fact that cardiac ischemia can be completely asymptomatic. Waiting for a patient to tell you about their recurrence of chest pain is dangerous.
- Repeat ECGs save lives!
- Queen of Hearts can differentiate active acute occlusive myocardial infarctions from reperfused OMI.
Reference:
[1] Tsao CW, Aday AW, Almarzooq ZI, et al. Heart Disease and Stroke Statistics—2023 Update: A Report From the American Heart Association. Circulation. 2023;147:e93–e621.
More Learning Points from Smith:
- Any patient with OMI that is reperfused can have re-occlusion at any time.
- Re-occlusion is not always accompanied by chest pain
- These patients, in my opinion, should go for emergent angiogram. They are “Transient STEMI” or “Transient OMI“
- Transient STEMI was studied by Lemkes, randomizing to emergent vs. delayed intervention. Mortality was the same, but many patients in the delayed group had re-occlusion and needed to go the the cath lab emergently in the middle of the night.
- See these cases to illustrate that, if you do not go emergently, the patient may re-occlude painlessly. You should therefore use continuous ST segment monitoring. See this case: Why we need continuous 12-lead ST segment monitoring in Wellens’ syndrome. Here is the initial ECG of this case, recorded after resolution of prehospital chest pain:
More cases discussing Continuous 12-lead ST Segment Monitoring.
= = =
======================================
MY Comment, by KEN GRAUER, MD (12/7/2025):
Dr. Smith asks the important question in today’s case as to whether emergent cardiac catheterization is needed in a patient who has just had an MI — but who is now pain-free and showing reperfusion T waves on ECG?
= = =
How Do You Know?
How do you know if the MI that this patient has just had is “complete” — or, was momentarily complete, but is now ongoing?
- The simple answer to the above question is, You don’t know … which fortunately in today’s case was quickly addressed by repeating the ECG immediately after contacting a naysaying consultant.
- But what if the repeat ECG failed to show any change? The answer is that we simply don’t know if or when a recent OMI may spontaneously reocclude …
- An important hint in today’s history that this acute MI might still be ongoing — is that this patient’s symptoms have been “stuttering” over the past 2 days. This is because a common reason for “stuttering symptoms” are ongoing episodes of spontaneous reperfusion that are punctuated by episodes of transient spontaneous reocclusion. Eventually, the final state of the “culprit” artery will be reached — but we have no idea if this final state will be a patent or totally occluded “culprit” artery.
= = =
What Do Today’s ECGs Show?
For clarity and ease of comparison in Figure-1 — I’ve put the initial ECG and the repeat ECG together.
- ECG #1 — shows sinus rhythm with obvious indication of inferior MI. Each of the 3 inferior leads (II,III,aVF) show large Q waves, but with residual ST elevation — and with terminal T wave inversion in leads III and aVF (BLUE arrows in Figure-1).
- Confirmation of infarction is forthcoming from the ST segment flattening with slight ST depression in lead aVL — with terminal T wave positivity (nearly the mirror-image opposite picture in lead aVL of the ST-T wave in lead III).
- The taller-than-expected T wave in lead V2, and ever-so-slight ST depression in this lead are consistent with posterior MI. As is the case for the 3 limb lead BLUE arrows — this further supports the impression of infero-postero OMI, now with reperfusion T waves.
= = =- PEARL: Note that despite evidence of posterior OMI — the ST segment in lead V1 is not at all depressed. This suggests that “something else” must be attenuating the amount of ST depression that we would normally expect to see in lead V1 as a result of posterior OMI — with this “something else” most likely being acute RV MI (which in association with acute/recent inferior MI, strongly suggests the proximal RCA as the “culprit” artery).
- NOTE: The other possibility for explaining the unanticipated straightening of the ST segment in lead V1 — could be that there is multi-vessel disease with difficult-to-predict collateralization patterns (which we would only be able to verify via cardiac cath) — and which cardiac cath on this patient subsequently showed!
= = =
Figure-1: Comparison between the first 2 ECGs in today’s case.
= = =
What Does ECG #2 Show?
Lead-by-lead comparison in Figure-1 between the repeat ECG and the initial ECG, shows that within the space of a few minutes — there have been “dynamic“ ST-T wave changes.
- The heart rate is faster.
- ST elevation is greater in each of the inferior leads. The ST-T waves in leads III and aVF are now hyperacute!
- Reciprocal ST depression is much more prominent in high-lateral leads I and aVL.
- There has been a dramatic change in shape and increase in the amount of ST segment depression in leads V2,V3,V4.
- Bottom Line: It is likely that the “culprit” artery had spontaneously reopened at the time ECG #1 was recorded — but has now spontaneously reclosed. This patient’s infero-postero MI is ongoing! It is because there is no way to accurately predict if or when spontaneous reclosure might occur — that optimal management of acute OMI most often entails prompt cardiac cath with PCI, even if the patient has become pain-free and reperfusion T waves have developed.
= = =
= = =
= = =