A 53 year old male with no previous cardiac history presented with sudden substernal chest pain with tingling of bilateral arms and dyspnea.
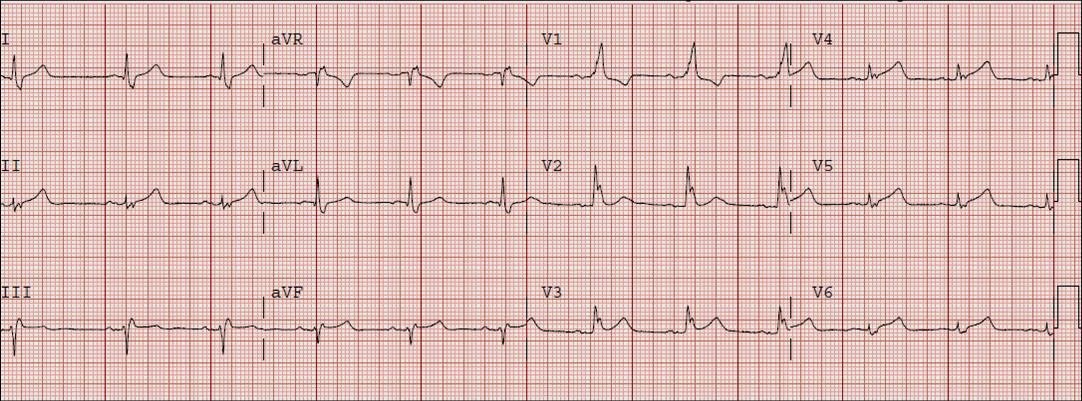
this is the first ECG at 1559:
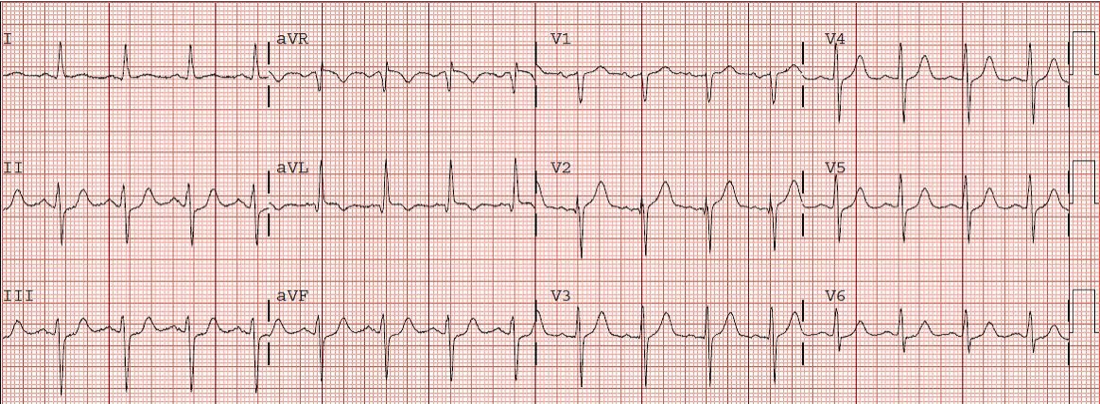
 There is very subtle and < 1 mm ST elevation in II, III, and aVF. The T-waves in these inferior leads are much larger than normal, with almost the same voltage as the QRS, and are “fat”. These are hyperacute T waves. Just as importantly, there is minimal reciprocal ST depression in aVL, with T wave inversion. This is diagnostic for inferior STEMI, even though it doesn’t meet the arbitrary criteria of 1 mm ST elevation in 2 consecutive leads. The cath lab was activated and a distal RCA thrombus with TIMI-0 flow was seen. For technical reasons, it could not be opened. An ECG was repeated, showing the development of the inferior MI without reperfusion:
There is very subtle and < 1 mm ST elevation in II, III, and aVF. The T-waves in these inferior leads are much larger than normal, with almost the same voltage as the QRS, and are “fat”. These are hyperacute T waves. Just as importantly, there is minimal reciprocal ST depression in aVL, with T wave inversion. This is diagnostic for inferior STEMI, even though it doesn’t meet the arbitrary criteria of 1 mm ST elevation in 2 consecutive leads. The cath lab was activated and a distal RCA thrombus with TIMI-0 flow was seen. For technical reasons, it could not be opened. An ECG was repeated, showing the development of the inferior MI without reperfusion: