This case was written up by one of our fantastic 3rd year residents, Michael Fischer. Edits by Smith.
A
mid 60s male with past history of 2 prior STEMI(+) OMIs s/p stenting (most
recently ~2 years ago) had onset of substernal chest pain after he came inside from smoking a cigarette. He reported becoming diaphoretic and also having pain in his L hand.
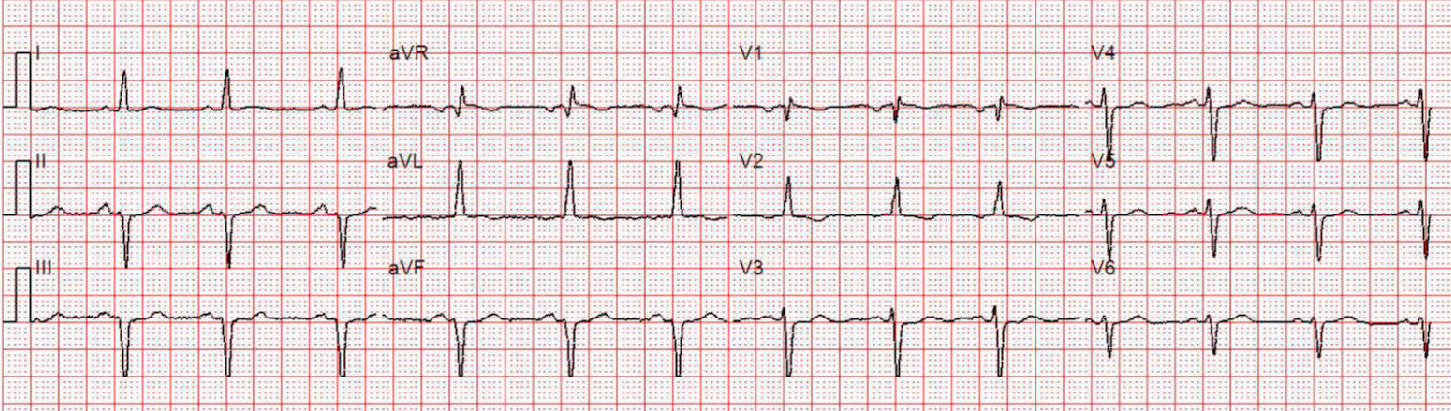
After approximately one hour, he called 911. Medics arrived and recorded a prehospital ECG:
Sinus rhythm. Deep QS-waves in inferior leads. Tall R-wave in V2, but no definite ST shifts or hyperacute T-waves.
He was given aspirin and sublingual nitroglycerin.
He arrived at the emergency
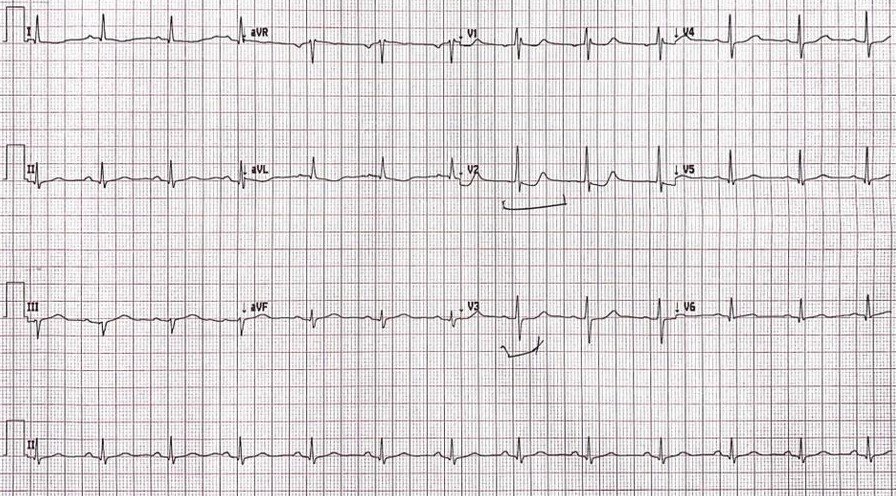
department by ambulance with continued chest pain. His initial ED ECG was as
follows:
–The most glaring abnormality in this ECG is the new ST depression in lead V2.
–However, there is also STD in V3.
–There is nearly 1 mm STD in both leads.
–There are also inferior QS-waves, consistent with his previous MIs with stenting of the RCA.
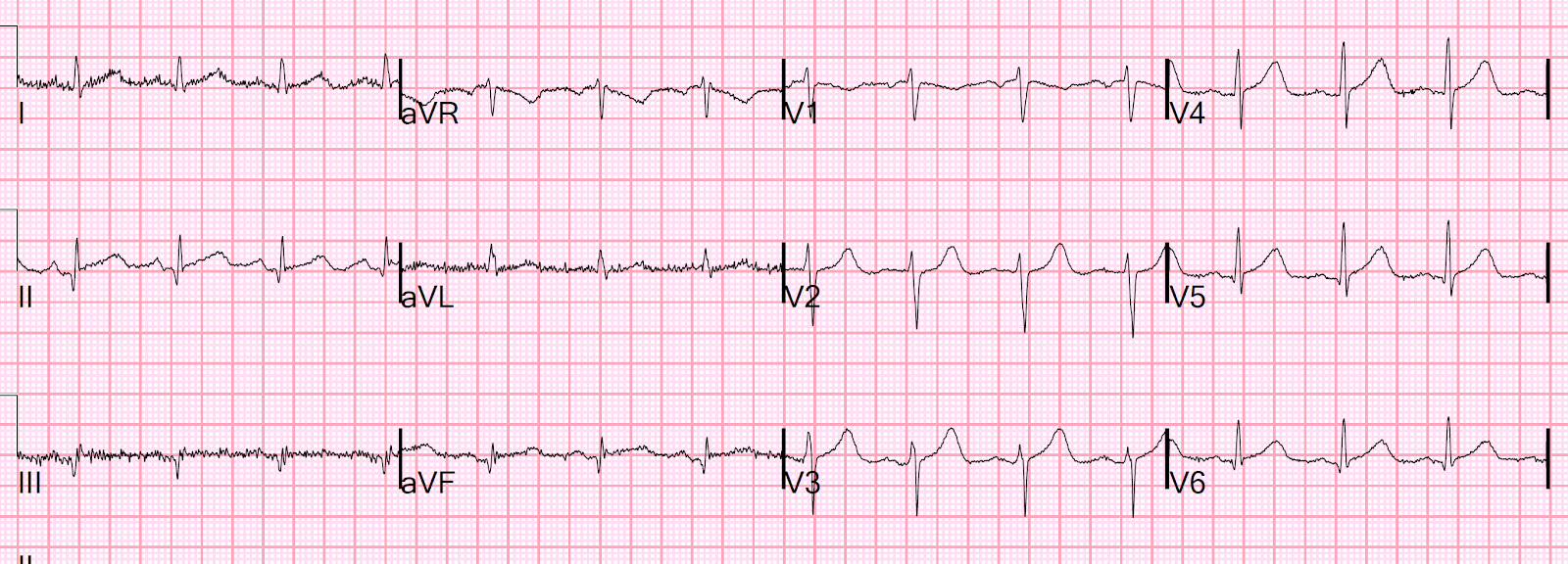
There was a previous ECG from 2 years prior, recorded the day after his previous stent:
This shows subacute inferior MI, and looks to be nearly complete (transmural completed infarct. (QS-waves and slight STE with shallow T-wave inversion.)
Smith comment: seeing this made me curious as to whether it was indeed a very large infarct. In fact, there had been 2 previous inferoposterior infarcts, and the patient presented rather late for the 2nd one, resulting in very large infarct with troponin I peaking at over 55 ng/mL (~55,000 ng/L for hs assay).
Although we recognized the ST depression as present in only a single lead, immediate concern was warranted and an additional nitroglycerin sublingual tab was ordered. Prior to its administration an additional ECG was obtained.
Not much changed. ST Depression continues. He had continued chest pain at this time and the sublingual nitro tab was given. Heparin was ordered.
Cardiology was consulted, and prior to their callback a third ECG was obtained.
This
shows improving ST depression in V2 and V3. His pain was still present
but improved after the additional nitro
tab was given. Cardiology evaluated the patient in the emergency
department shortly after this third ECG and were appropriately
concerned. A nitroglycerin drip was started and the patient was taken to
the catheterization lab.
Angiogram
His
coronary angiography revealed 90% stenosis of the proximal 1st obtuse
marginal branch (OM1), with suspected recent
plaque rupture. A drug eluting stent was deployed and he was discharged
to home the following day on dual antiplatelet therapy.
Peak troponin was over 50,000 ng/L (very large OMI)
Echocardiogram
The estimated left ventricular ejection fraction is 46%.
Regional wall motion abnormality-inferior.
Regional wall motion abnormality-inferolateral.
The previous Echo had an EF of 60% and only a “probable” inferolateral wall motion abnormality.
Remember: “lateral” often includes the posterior wall in echocardiography. In this case, the ECG proves that the affected part of the lateral wall includes the “posterior” wall: the part of the heart facing the posterior chest wall.
Learning points
1. In the right clinical context, ST depression maximal in leads V1-V4, even if less than 1 mm, and even if not obviously present in more than 1 lead, is Occlusion MI (OMI) until proven otherwise.
2. Transient STD in V1-V4 should be assumed to be Transient OMI (just as there is transient STEMI [see cases of transient STEMI here]). Just because the ST depression is transient, and seemed to resolve after nitroglycerine, does not mean that it is due to subendocardial ischemia. This anterior STD was reciprocal to a POSTERIOR ST vector, due to Occlusion of a large branch of the Circumflex (the Obtuse Marginal, or OM) which supplied a very large posterior myocardial territory. The peak troponin was over 50,000 (we do not know exactly how high), a very large MI.
3. In such cases, your degree of clinical suspicion must remain high.
4. It is good to have cardiologists who recognize and respond to Occlusion MI, and do not demand that the ECG meet STEMI criteria.