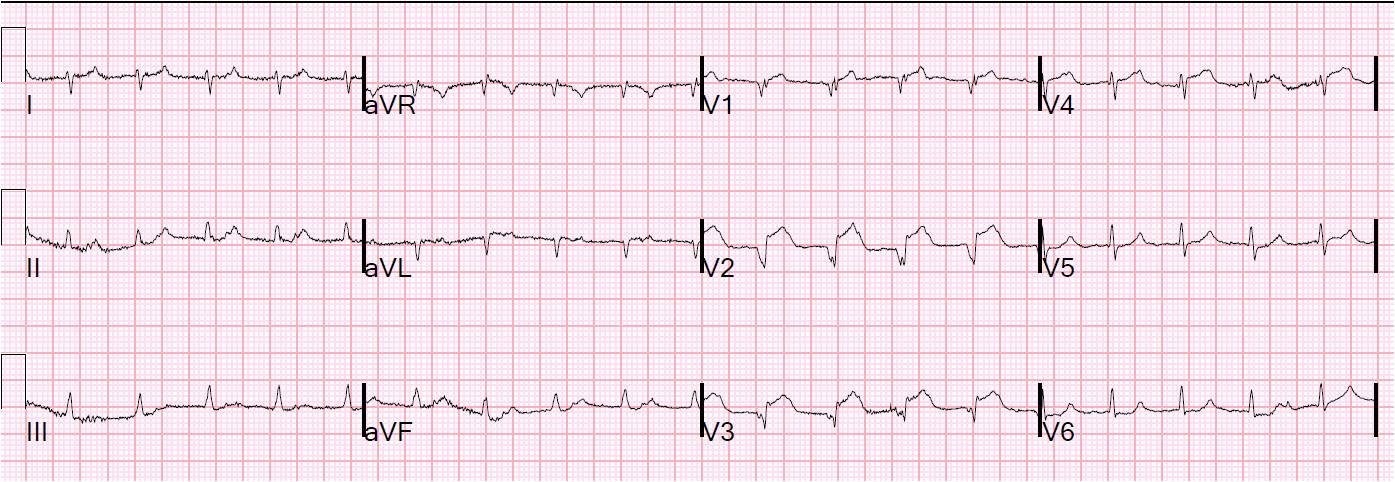
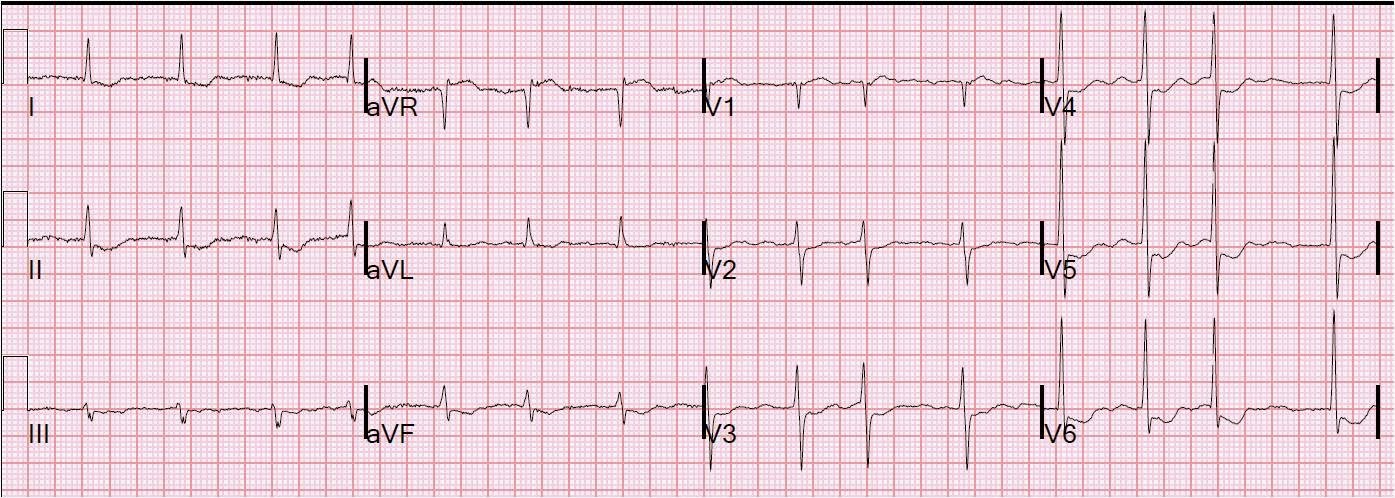
79 yo patient with no known previous history of MI and a history of severe dementia presented with acute dyspnea, pulmonary edema, BP 110/70 and tachycardic, requiring noninvasive ventilatory support. CXR confirmed pulmonary edema. Bedside echo showed severe anterior wall motion abnormality and very poor EF. Here is the ECG:
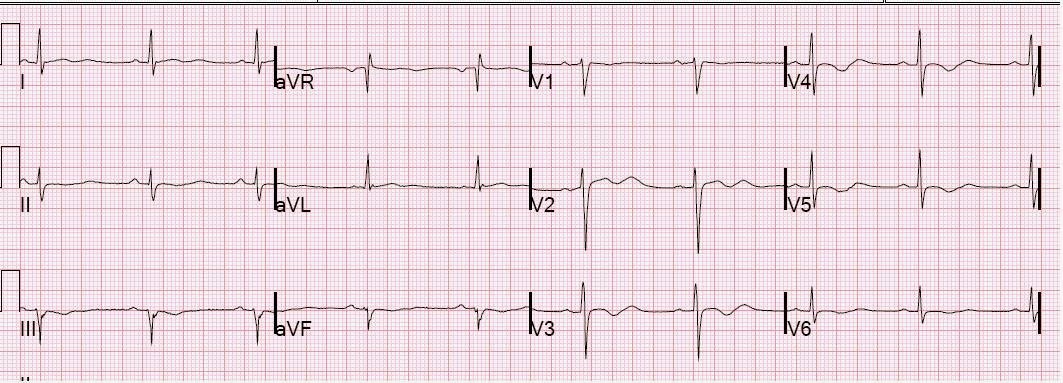
A previous ECG was found from 3 years prior:
 |
| No evidence of anterior MI |
After exhaustive inquiry, it was determined definitively that this patient would not want to be intubated under any circumstances. He could not undergo PCI without intubation and paralysis. We considered fibrinolytic therapy, heparin, GP IIbIIIa inhibitors, but decided to give aspirin alone.
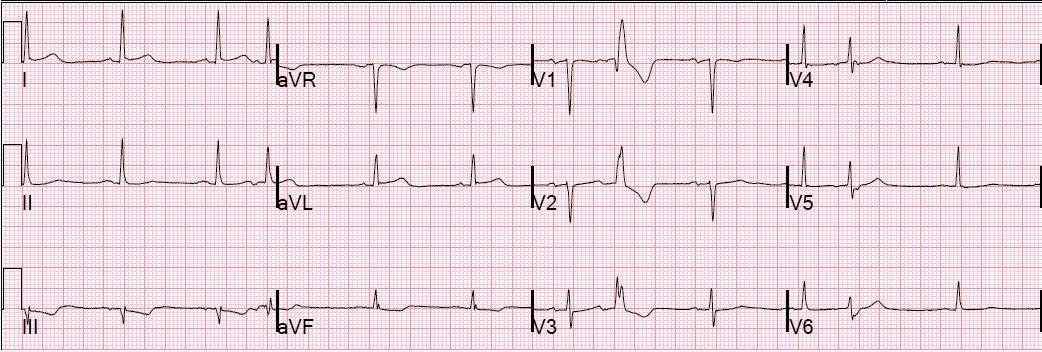
Interestingly, the next AM he was much better, he was no longer SOB, his troponin peaked at only 2.7 ng/ml. A formal echo showed severe anterior wall motion abnormality with dyskinesis and EF of 15%. Dyskinesis usually implies LV aneurysm and is unusual in acute STEMI, so it is quite possible that he had a previous undiagnosed anterior MI since 2008, and that he now has a superimposed STEMI.
He never had a subsequent ECG, but I can only surmise that he had spontaneous reperfusion (this occurs in up to 25% of STEMI). If he indeed underwent reperfusion, and does not re-occlude, his ejection fraction will mostly recover.
When we are certain that our therapy saved the patient, cases like this should give us a bit of humility!