A woman in her 40’s was involved in a head-on motor vehicle collision. EMS noted a facial droop. On arrival she was hypertensive but other vitals were normal. She did complain of back and neck pain, chest pain, and SOB. She also had a facial droop as noted by medics. This droop was apparently new.
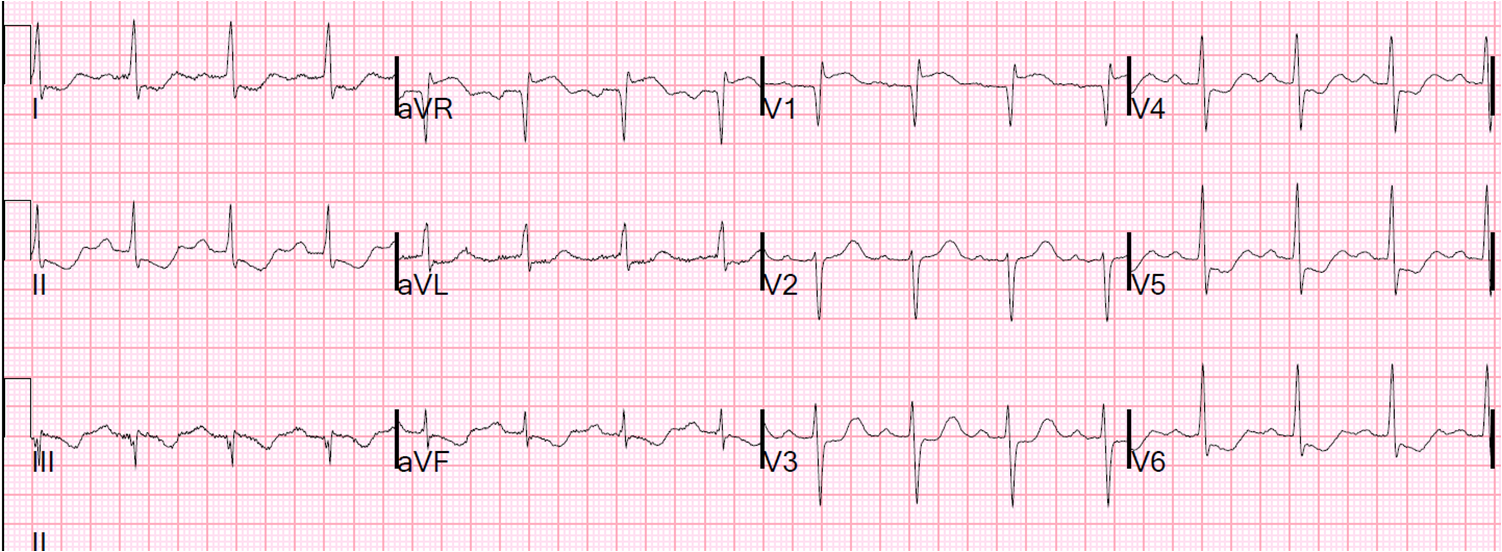
An ECG was recorded:
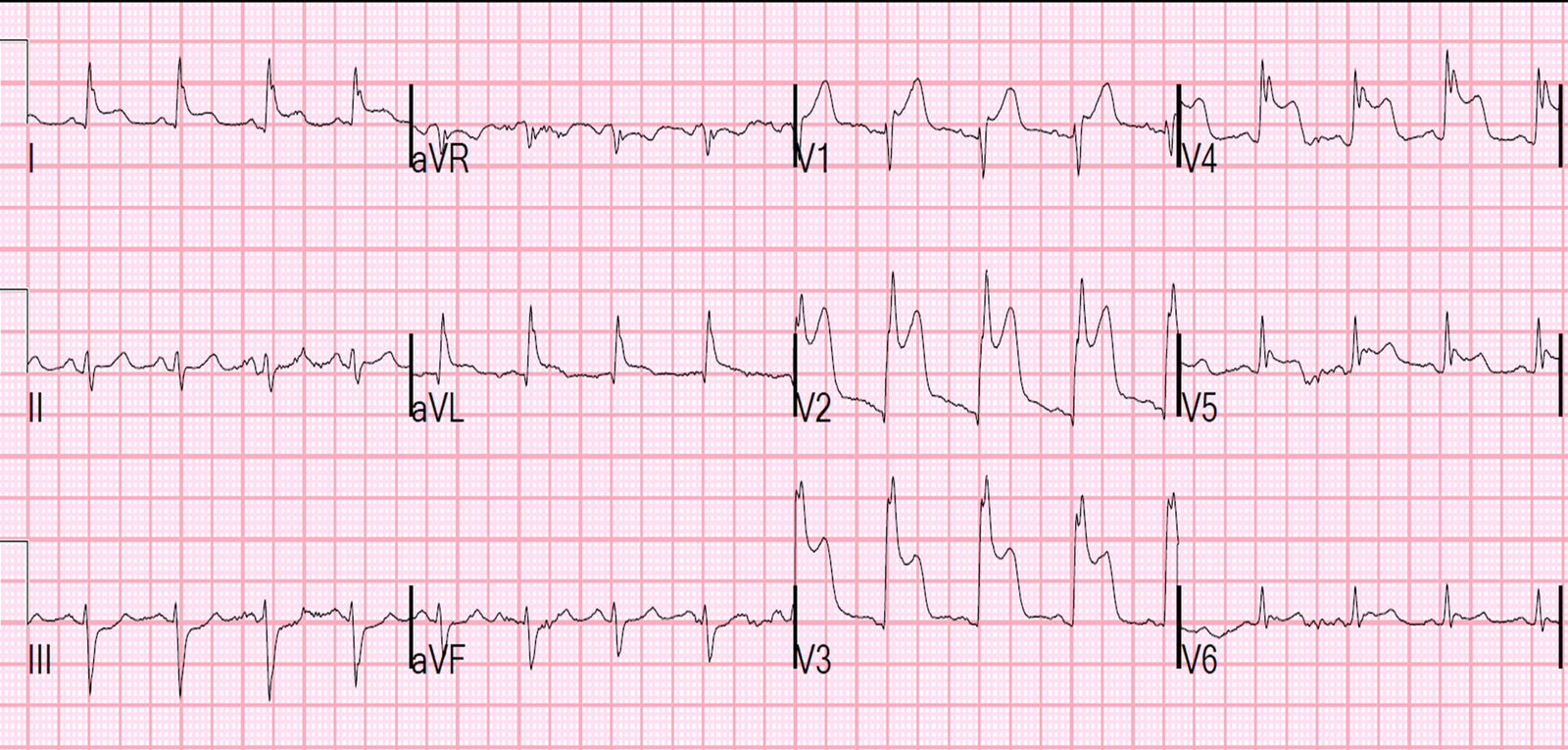
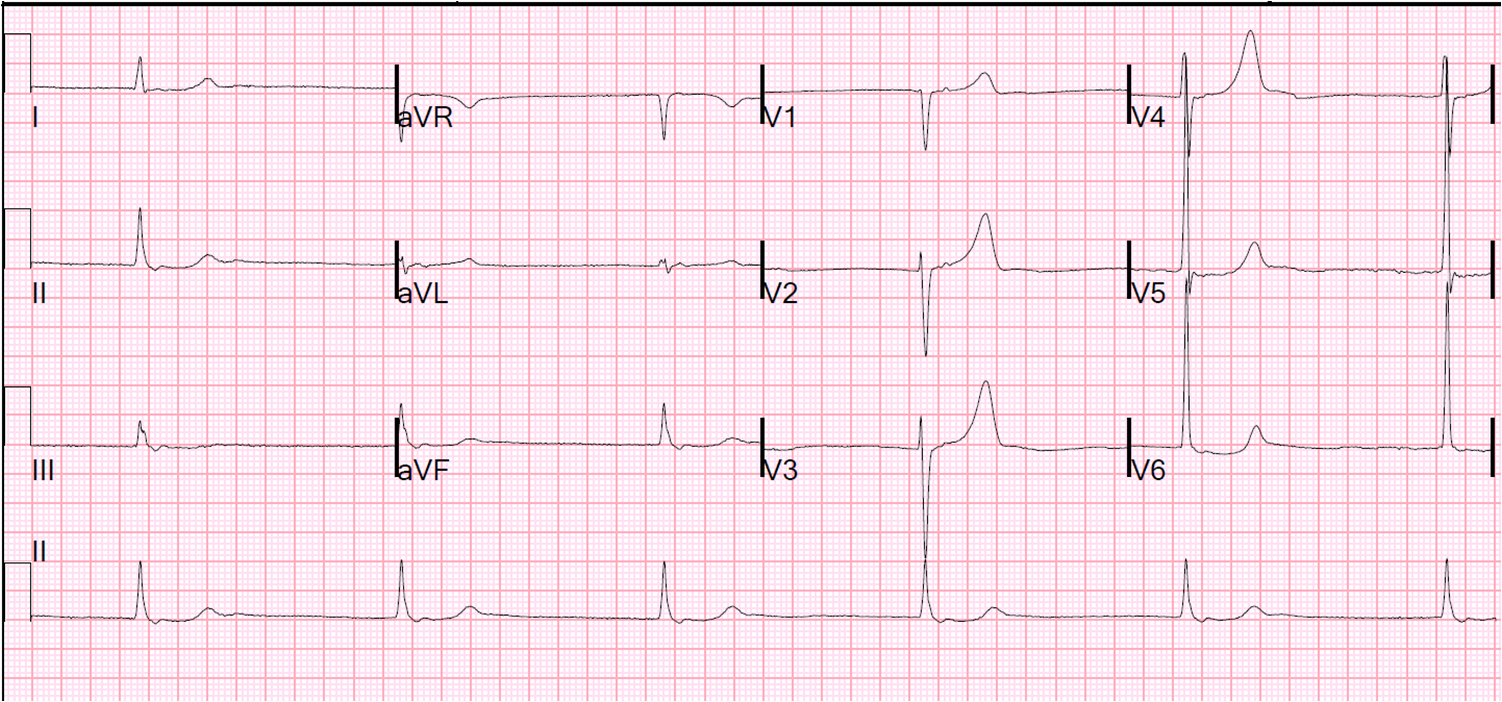
The ECG was repeated 36 minutes later:
 |
| The findings are improving |
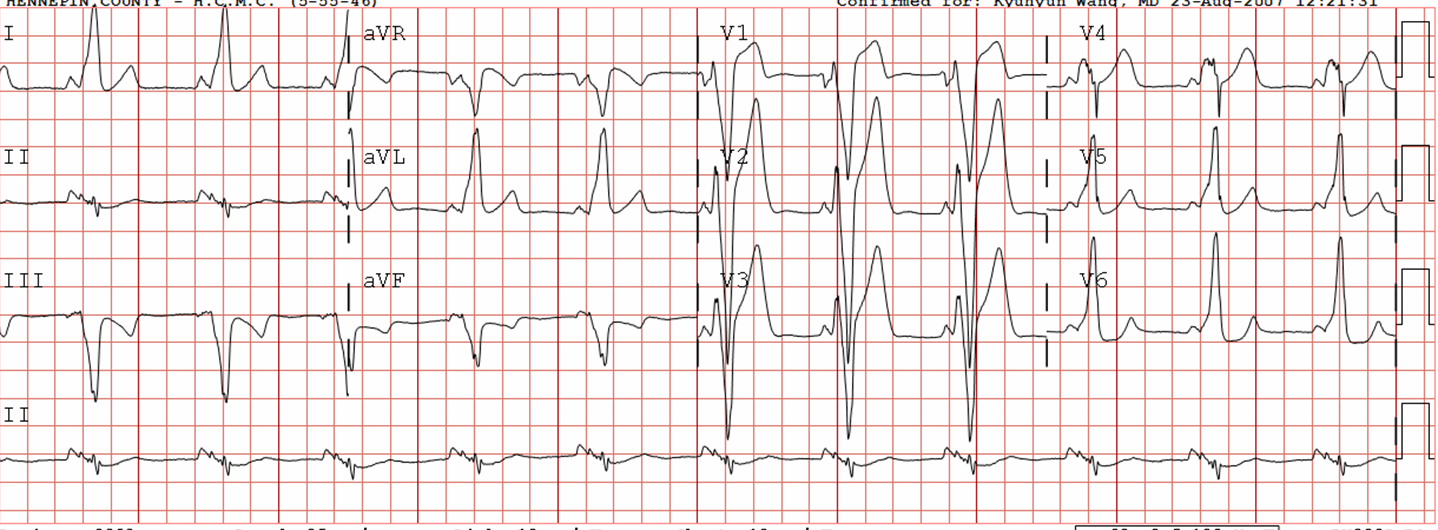
Is this:
1. Myocardial contusion?
2. Stress Cardiomyopathy due to stroke?
3. ACS?
4. Type II (demand ischemia) from stable coronary disease with stress?
5. Aortic
dissection affecting both carotid artery and aortic coronary cusps?