67 year old female complaining of epigastric pain that radiates to her
chest. Relief with burping. Symptoms had been ongoing for about 1 hour
prior to 911. Symptoms started after eating a high fat meal.
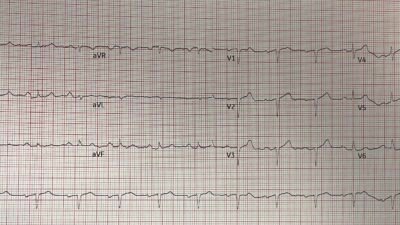
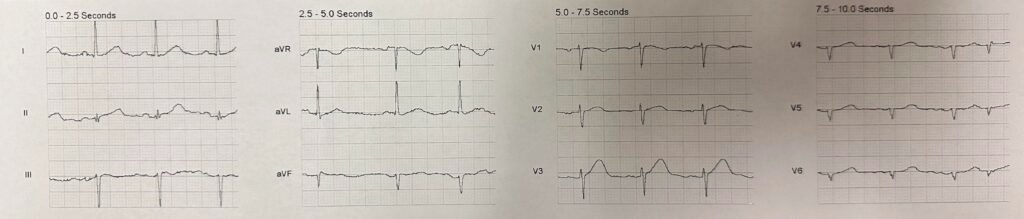
On arrival, the crew did a workup on her complaints which included a
12-lead ECG.
What do you think?
Smith: there is a clear hyperacute T-wave in lead V3. This is diagnostic of LAD OMI, but it is unusual to only be seen in one lead. I do wonder about lead placement. There is also very poor R-wave progression in V4-6, which contributes to a suspicion of LAD OMI.
The Queen of Hearts missed this one (raw output = 0.24; above 0.50 is OMI)
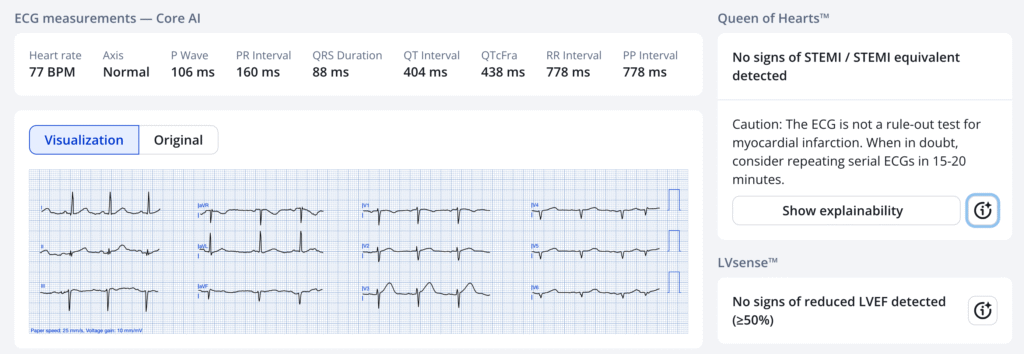
The PMCardio Hyperacute T-wave system identifies the HATW, but only in V3. Our definition of HATW in this system requires an average of 2 consecutive leads with a value over 0.7 (not related to the Queen’s raw output)
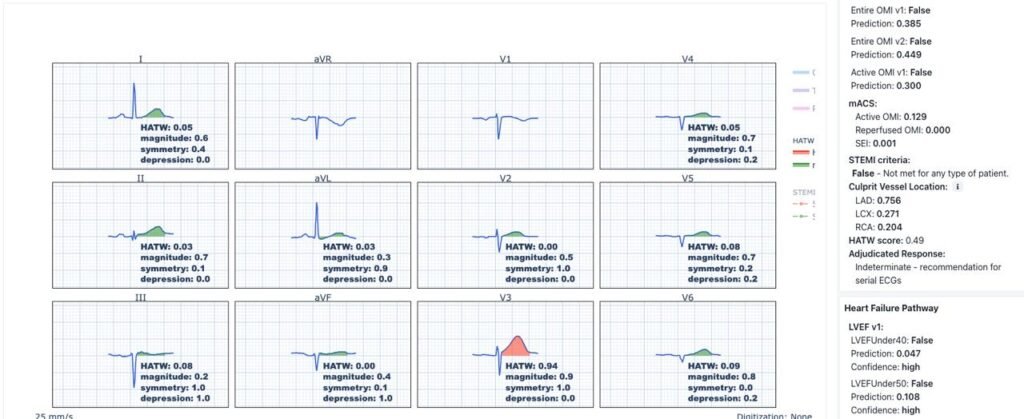
HATW in V3 only, with magnitude of 0.93; but all the adjacent T-waves are not at all hyperacute.
The medics did not see acute MI, nor did the Zoll interpretation.
When time to transport, the patient stated she did not want
to go. Because the 12-lead did not say “STEMI” and the crew did not
recognize the ECG characteristics (to no fault of their own, as this
is not discussed in paramedic school and is only now starting to make
its way to the prehospital world), they were going to sign the
patient and leave her at home.
When the crew handed the patient the computer to sign a refusal, the
patient became unresponsive and pulseless.
She was found to be in ventricular fibrillation and was resuscitated.
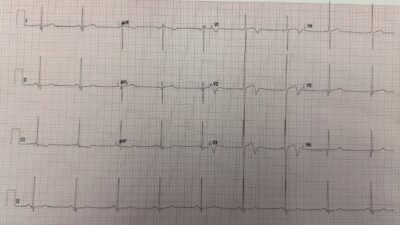
Here is the ECG after arrest:
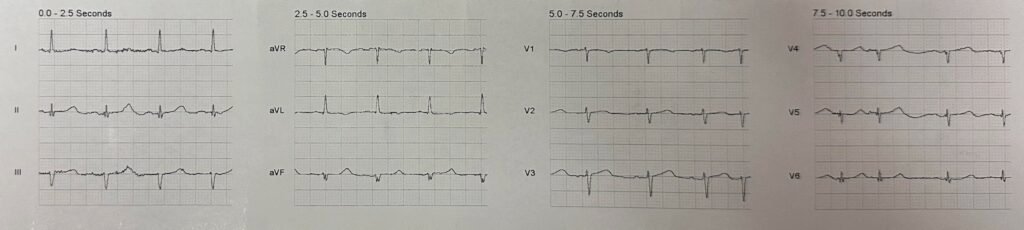
Now there is no evidence of OMI. Spontaneously reperfused.
The crew immediately recognized vfib and defibrillated the patient
bringing her back to a perfusing rhythm. After the defibrillation, the
patient regained consciousness and stayed this way throughout
transport.
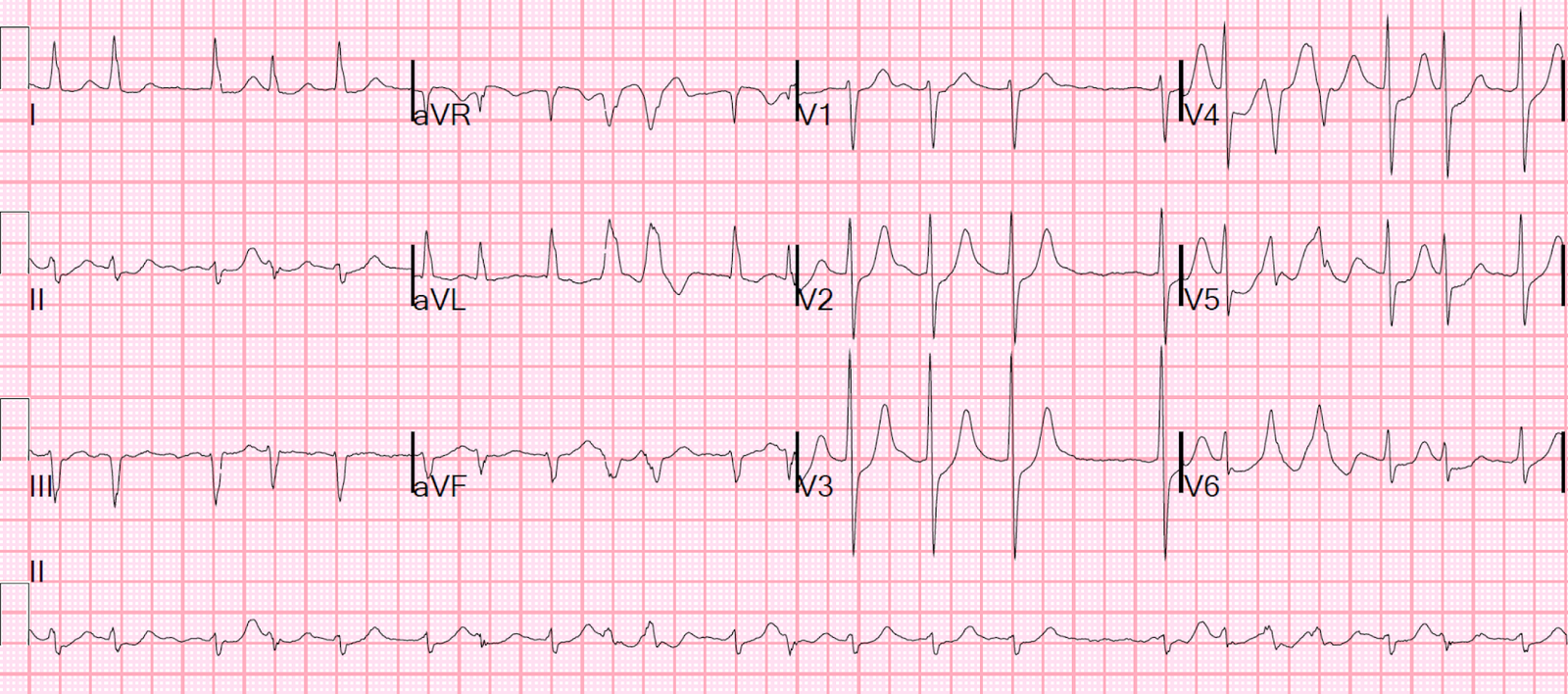
At the hospital, the patient was worked up for a PE. Smith: this is clearly NOT a PE, but a myocardial infarction with v fib arrest!
Initial troponin was 158 ng/L. 2 hours later, second troponin 2641 ng/L with the statement “This is consistent with her initial chest pain that was likely an NSTEMI that caused the V-Fib arrest…” also, “Cardiology did not feel she needed to proceed to Cath Lab unless she developed recurrent pain ..”
There is no more followup.
Learning Points:
- Learn to recognize hyperacute T-waves.
- Do not ignore hyperacute T-waves.
- The Queen of Hearts, though better than probably any human being, is not perfect
- In OMI, there can be Hyperacute T-waves limited to just one lead.
- Most important: an ECG can be entirely normal in OMI. Acute MI can only be “ruled out” with troponins.
= = =
======================================
MY Comment, by KEN GRAUER, MD (11/17/2025):
The “Answer” to the question posed by Dr. Smith is “No” = In a patient with CP — the medics should not leave the patient at home even if the ECG is “normal.” There are several reasons why I say this:
- — i) Even if the ECG is correctly interpreted as “normal” — it could be that the ECG was recorded during “Pseudonormalization” (ie, If spontaneous reperfusion occurs — then “on the way” from ST elevation to the T wave negativity of reperfusion T waves — there will be a period in which the ECG may look relatively normal!).
- — ii) “Beauty is in the eyes of the beholder” — which translates in the world of ECG expertise as what may be interpreted as “normal” by one person — might clearly be abnormal to a more expert interpreter (especially when the ECG in question is from a patient with new CP). In today’s case, before I knew that this patient coded — I immediately interpreted the initial ECG as definitely abnormal in this older woman with new CP!
= = =
Why is the Initial ECG Abnormal?
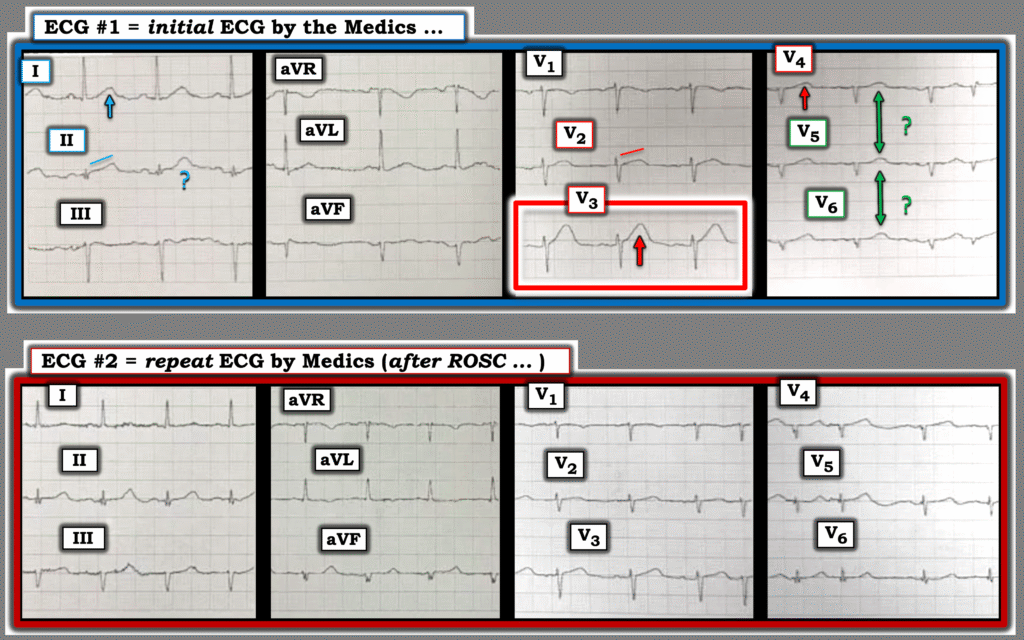
In addition to the obvious hyperacute T wave in lead V3 of the initial ECG that Dr. Smith emphasized in his above discussion (within the RED rectangle in Figure-1) — there are a number of other concerns with this tracing:
- There is definite lead misplacement of leads V5,V6 — as P waves, QRS morphology and T wave appearance in leads V4,V5,V6 is virtually identical! (GREEN double arrows in ECG #1). We know that left-sided lead V6 can not be correct in ECG #1 — because the QRS is tiny and almost entirely negative — whereas much more reasonable voltage with an essentially all-positive QRS complex is recorded in both left-sided limb leads ( = leads I and aVL).
- Given that the history is new CP in this older woman — awareness that we are unable to include leads V5,V6 (if not also V4) in our interpretation because of obvious lead misplacement — is clear indication to immediately repeat the ECG, so that we can have access to all 12 leads for optimal decision-making!
- Given the clinical context of new CP in an older woman — I thought both of the neighboring leads to the obvious hyperacute T wave in lead V3 were also abnormal. For example — Instead of the normal, slowly upsloping ST segment that blends into an upright T wave (as is normal for lead V2) — we see straightening of the ST segment takeoff.
- And — if lead V4 is correct (and it is only leads V5,V6 that are malpositioned) — then the T wave in lead V4 is also hyperacute by being much “fatter”-at-its-peak than it should be given small size of the QRS (and given that this lead is right next to lead V3 which is so obviously hyperacute).
- Given these abnormal chest lead findings in this older woman with new CP — I also interpreted the T wave in lead I as abnormal, being “fatter”-than-it-should-be.
- Lead II is difficult to interpret — because we really only see 2 QRST complexes, and the 2nd complex (highlighted by the ? ) looks altered by artifact. So, judging by the only QRST complex that we have to go on in lead II — the straightening of the ST segment takeoff that rises to a disproportionately tall T wave in this lead with such a tiny QRS — is abnormal until proven otherwise.
My Impression of ECG #1: Given the history — any potentially acute ST-T wave abnormality needs to be assumed abnormal until proven otherwise. The finding of the obviously hyperacute T wave in lead V3 — in association with the other findings described above — makes for 5/10 leads suggesting acute OMI (with V5,V6 excluded from diagnostic consideration given lead misplacement).
- Comparison of ECG #1 with ECG #2 is insightful. As per Dr. Smith — this post-resuscitation ECG tells us there has been spontaneous reperfusion of the “culprit” artery. Specific changes to highlight in this comparison in Figure-1 include: i) Deflation of the abnormal ST segments in leads I,aVL; V2,V3,V4; — ii) Terminal T wave positivity now in leads III,aVF (this being another indication of spontaneous reperfusion); — and, iii) A change in QRS morphology for leads V5,V6, which now both show some positivity (thereby confirming that leads V5,V6 were malpositioned in ECG #1).
= = =
Additional Learning Points:
- Awareness of a high-risk history (ie, today’s older woman with new CP) — is important in our interpretation. Such a history tells us that we need to rule out an acute OMI, rather than having to “rule it in”.
- The presence of a single clearly hyperacute T wave (as in lead V3) in a patient with new CP — is all-that-is-needed to know that the cath lab should be promptly activated.
- If uncertain about the acuity of the initial ECG (as providers in today’s case were) — then awareness of lead malposition (as was evident for leads V5,V6 in ECG #1) is indication to immediately repeat the ECG, rather than handicapping your interpretation by not having a full 12-lead tracing that you can interpret.
= = =
Figure-1: Comparison of the 2 ECGs in today’s case.