A 71 year old male complained of near syncope and SOB without any chest
pain. His pulse was slow. He was put on the monitor. Here is the
rhythm strip:
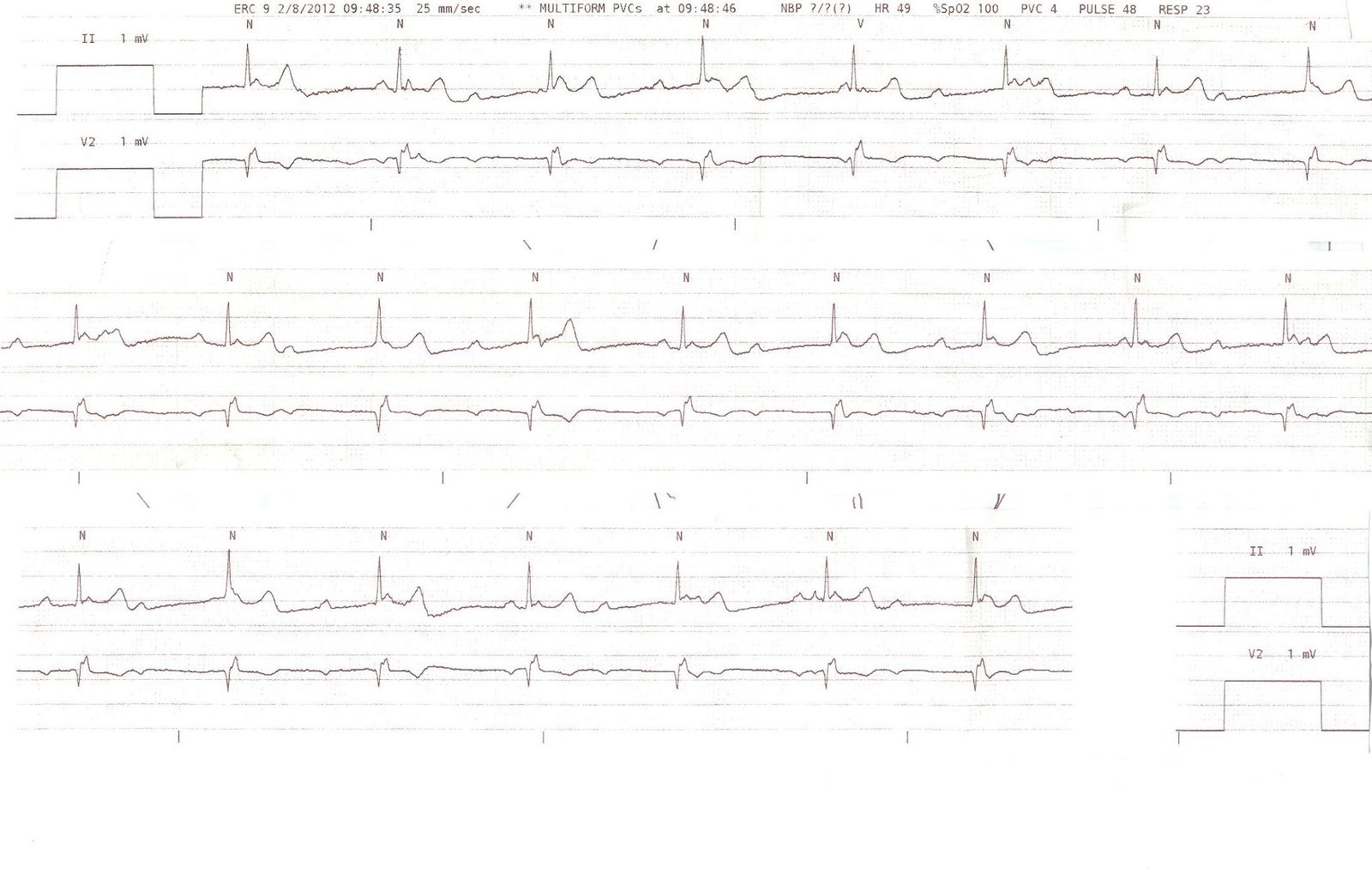 |
| There is 3rd degree AV block at a rate of 48 |
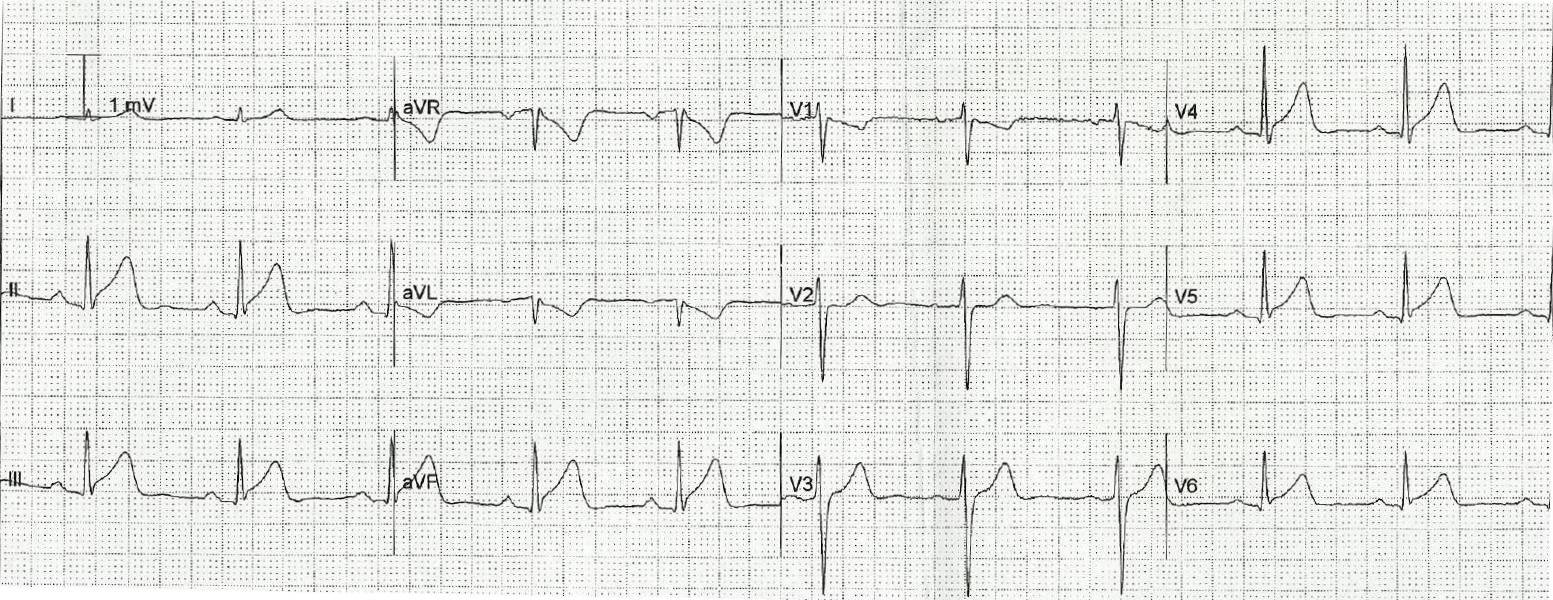
A 12 lead ECG was recorded about 5 minutes later:
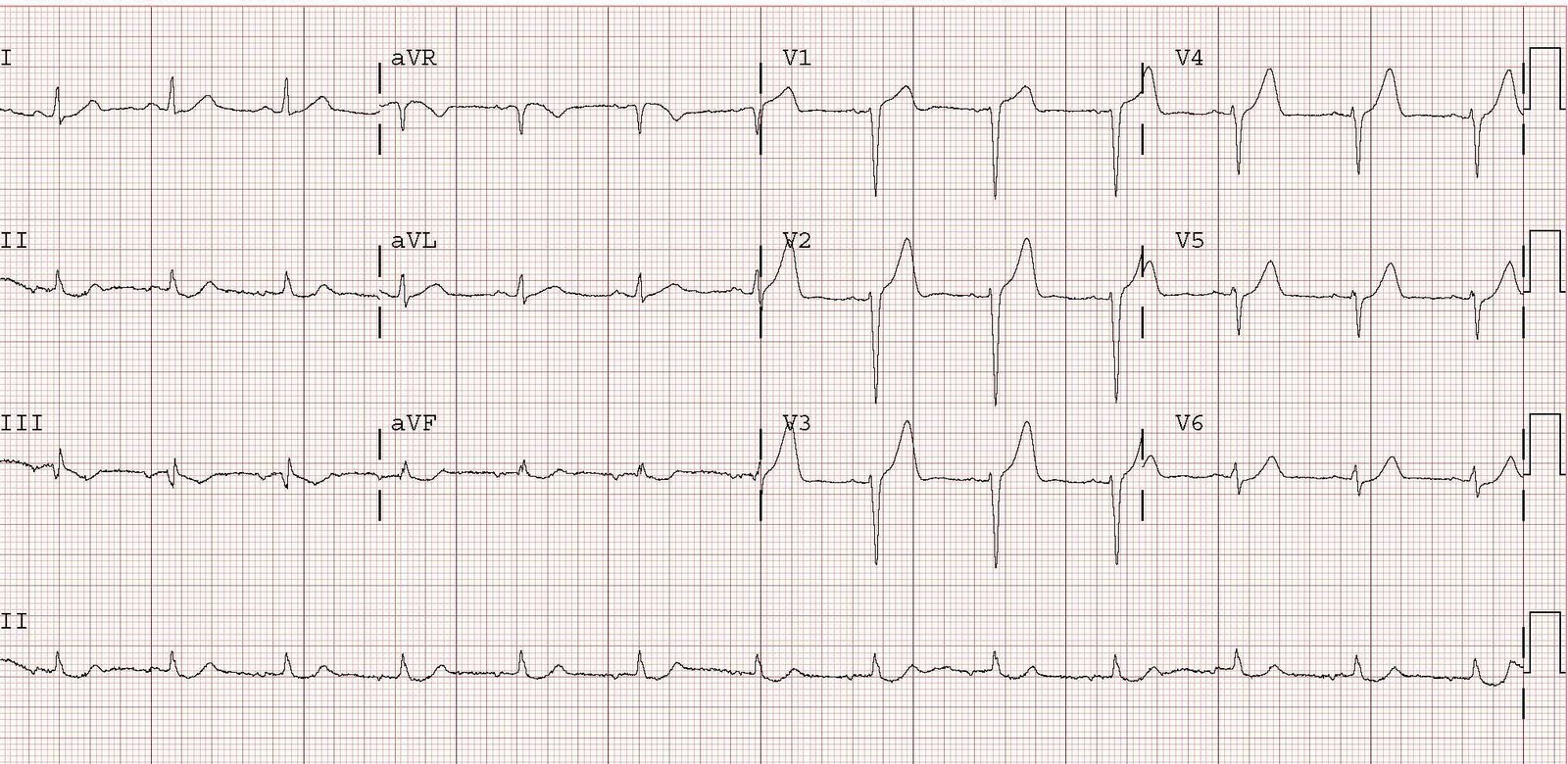
21 minutes later the patient became bradycardic again, so this ECG was recorded:
One might think that because there is associated RBBB, that it is infranodal
AV block. But the RBBB was present when the block and ST elevation
were not, so it is likely a baseline feature of this patient’s ECG.
Furthermore, inferior STEMI is much less likely to cause infranodal
block. The blood supply to the AV node is from the RCA, and the
infranodal (HIS bundle) area is supplied by the LAD. Therefore, intranodal (in the AV node) block is much more likely than infranodal (below the AV node, in the bundle of HIS).
When in the node, AV block has a much better prognosis than when below the node.
In the setting of STEMI, the ACC/AHA guidelines, page 618, recommend permanent pacing as a Class I indication for:
1. persistent second-degree AV block in the His-Purkinje system (infranodal)
with bilateral bundle-branch block or third-degree AV block within or
below the His-Purkinje system after STEMI. (Level of Evidence: B)
2. transient advanced second- or third-degree infranodal AV block and associated bundle-branch block. If the site of block is uncertain, an electrophysiological study may be necessary. (Level of Evidence: B)
3. persistent and symptomatic second- or third-degree AV block. (Level of Evidence: C)
Persistent here is important, because it is likely that, after opening the artery, the block will resolve, and thus will not be persistent.
The patient was comfortable while supine, even with 3rd degree AV
block. The block was intranodal. The patient would soon have PCI. So
no pacing was necessary. One should have external (transcutaneous)
pacing at the ready in case of worsening block, but with inferior STEMI
this is unlikely to be necessary.
He went to PCI and had a mid-RCA occlusion opened. Here is his post PCI ECG:
Initial troponin I was 0.035 ng/ml (99% reference, 0.034) and peaked at
13.4. Echo showed infero-postero-lateral wall motion abnormality.
Learning points:
1. STEMI does not always have chest pain or SOB. It is wise to obtain
serial ECGs when there are ischemic symptoms, and especially with AV
block.
2. Inferior STEMI may cause AV block, but it is intranodal
3. Infranodal AV block, especially in the context of anterior STEMI, is
very dangerous and will probably require internal pacing unless the
artery can rapidly be opened. Before the artery is opened, it is at
least likely to require external pacing.