Yesterday, I posted this interesting transient STEMI.
I was asked why it is not pericarditis. I have edited the post (see red text) to add the following:
Added to description of presenting ECG:
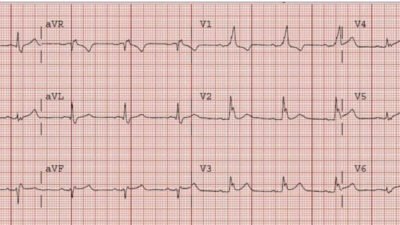
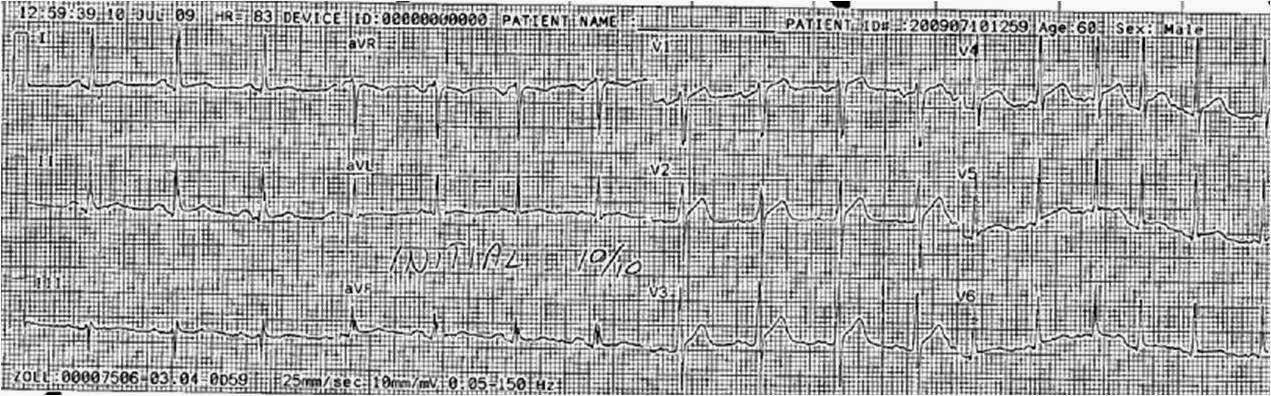
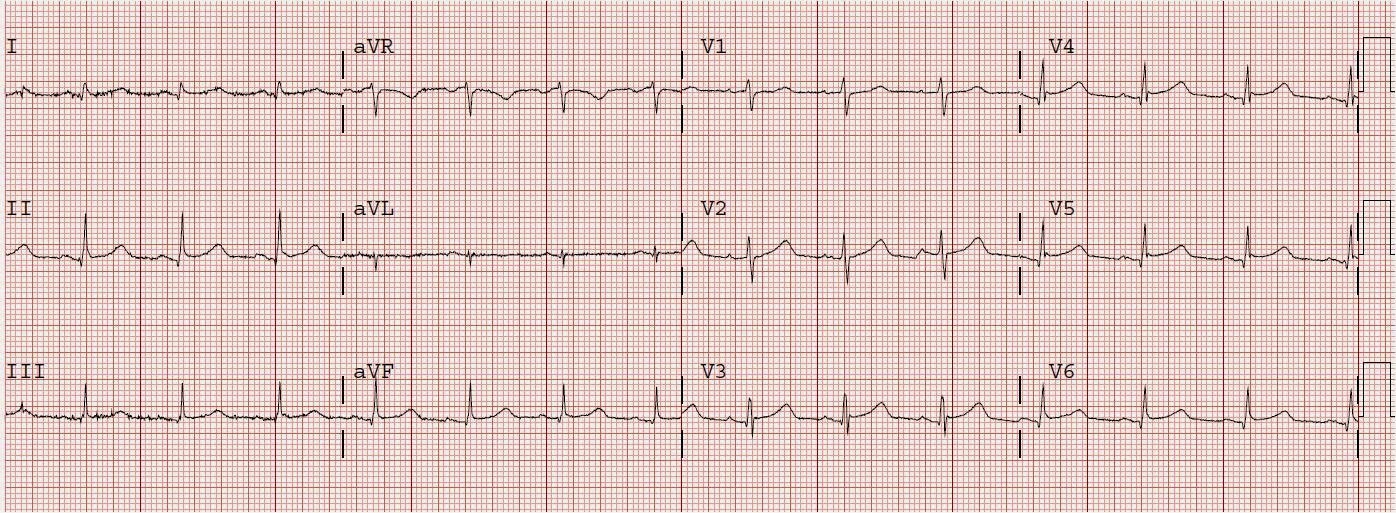
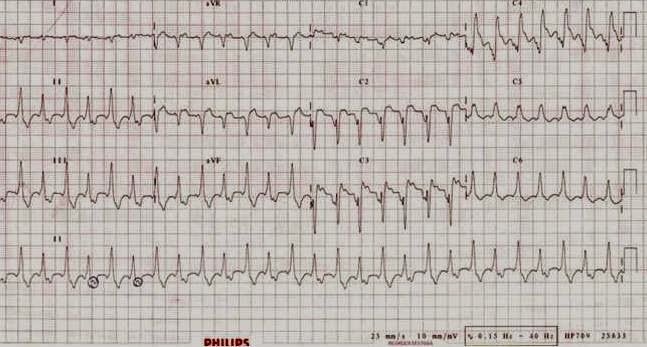
The old ECG has a Q-wave with persistent ST elevation in lead III, and some reciprocal ST depression (typical for aneurysm morphology). The new ECG has relative reciprocal ST depression in lead III, with ST elevation in aVL. This rules out pericarditis, which essentially never has reciprocal ST depression.
Added to description of old ECG:
Notice the ST elevation in lead III that follows a deep Q-wave. This is “Persistent ST elevation after previous MI” or “LV aneurysm morphology”. LV aneurysm is very different for inferior vs. anterior MI.
And have added the following to the conclusions:
4. This is not pericarditis because:
a. Pain was typical for MI (substernal, not postional or sharp, resolved with NTG)
b. There is relative reciprocal ST depression in lead III.
Pericarditis does not have reciprocal depression.
c. ST elevation of pericarditis is maximal in leads II and V5, V6.
Here the ST elevation is maximal in V2-V4.
d. Pericarditis does not have hyperacute T-waves.
e. Tight proximal LAD stenosis explains STE in precordial leads and I and aVL.