Subtitle: It’s not the ECG which is “Non-diagnostic” — it is the physicians who are “Non-diagnostic!”
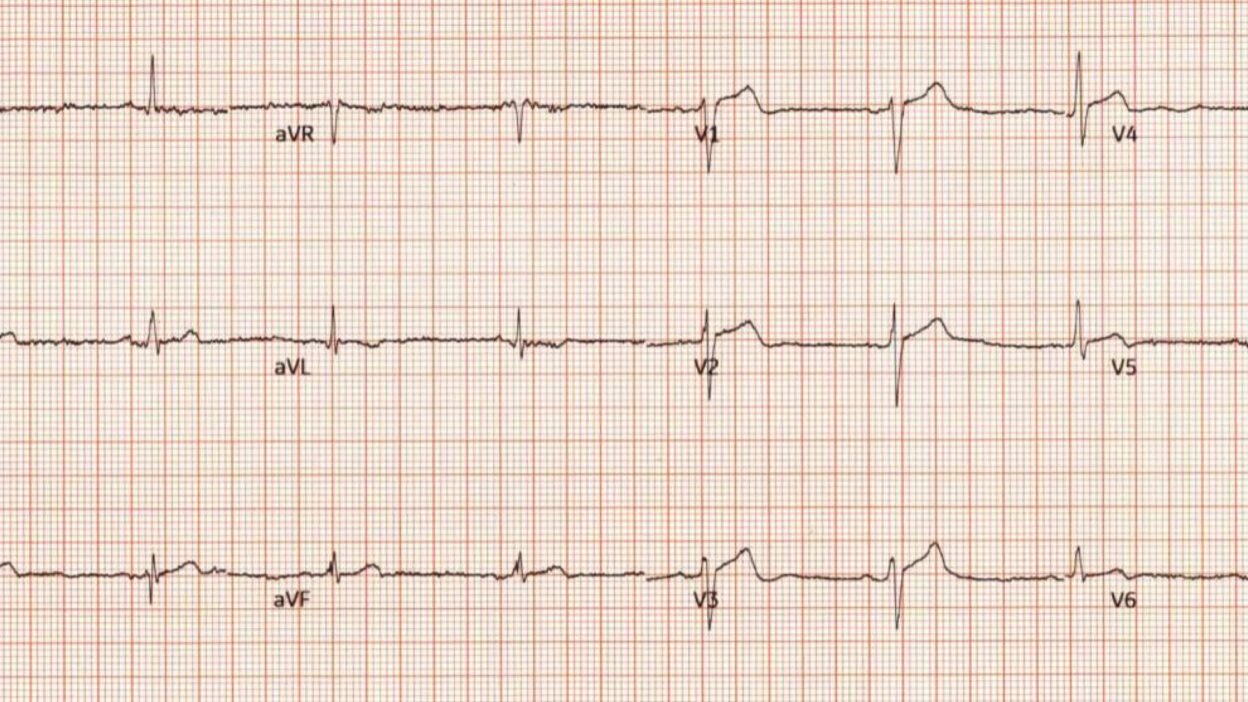
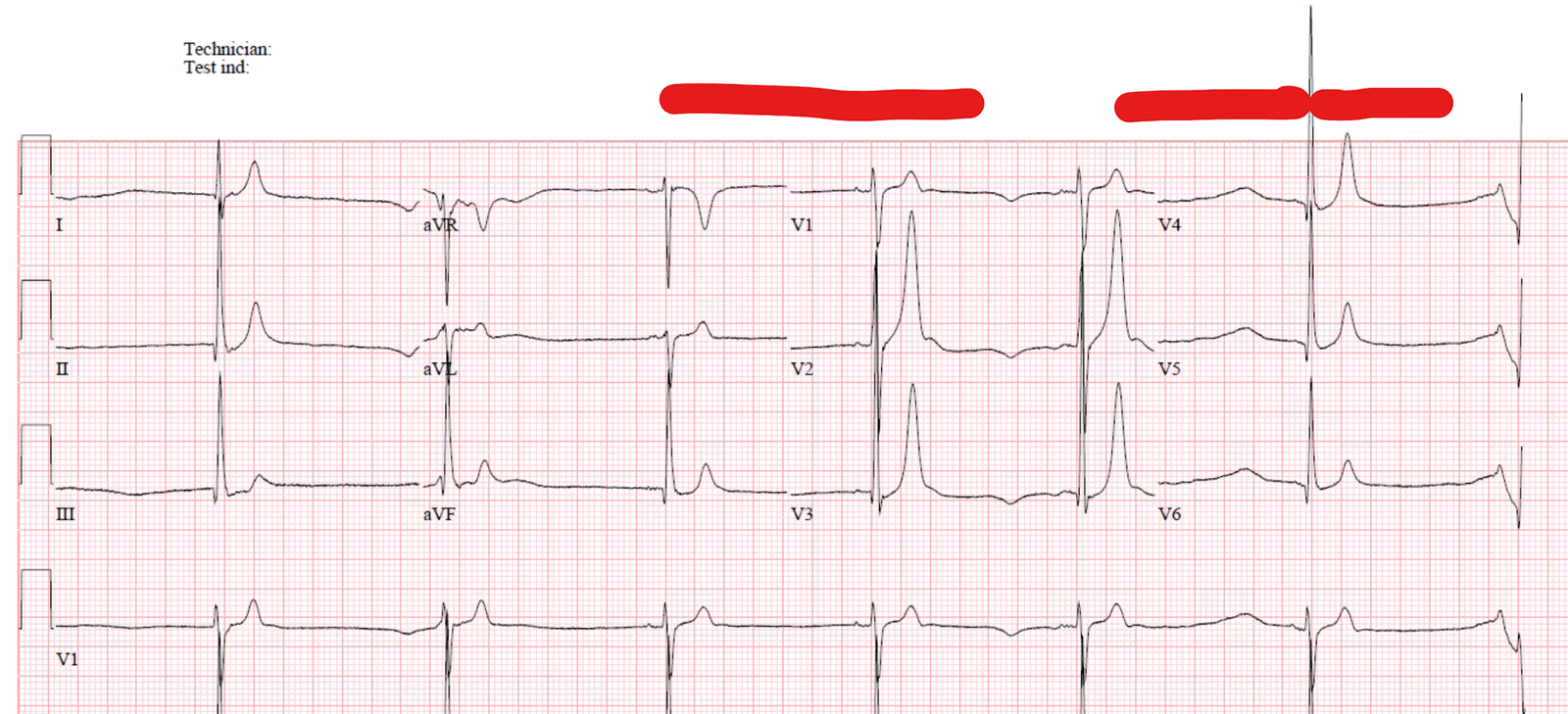
This ECG was sent to me, with no information, by a former resident.
What do you think?
Smith: “Diagnostic of inferior OMI.”
Response: “What makes you say that?”
Smith: “III and aVF, with reciprocal STD in aVL. There are also hyperacute T-waves in V1-V3, so this is probably a proximal RCA occlusion with RV infarct (Proximal to the RV marginal branch).”
His answer: “Yes, it was a proximal RCA occlusion.”
Case presentation:
A 45 year old man presented with chest pain. The above ECG was recorded. It was interpreted as normal.
The patient had 2 high sensitivity troponin I which were both at 24 ng/L (below the URL). No further ECGs were recorded.
The patient was discharged.
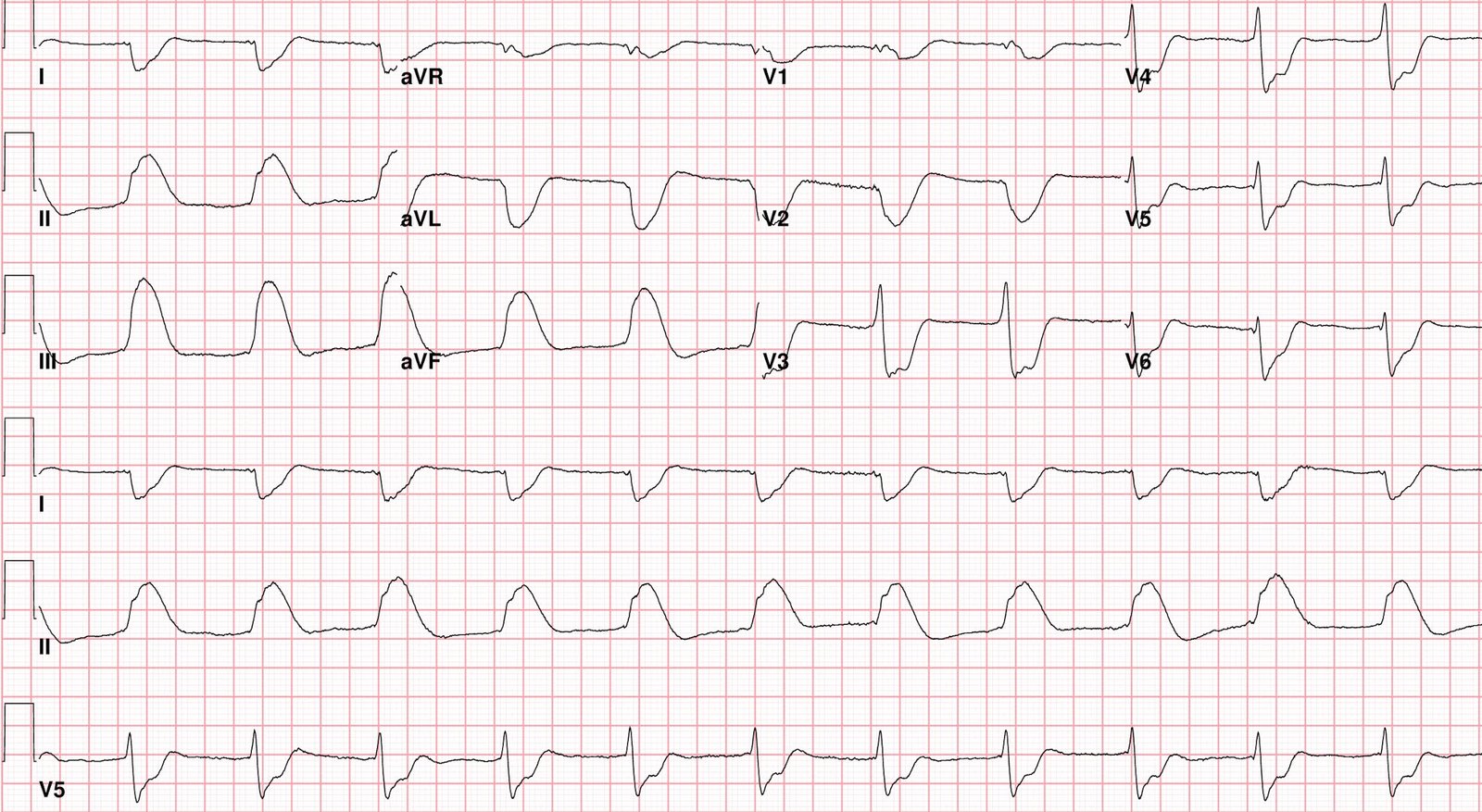
Some time later he presented by ambulance in cardiac arrest, in ventricular fibrillation.
ROSC was achieved after a long resuscitation.
Angiography confirmed an acute mid RCA occlusion.
There was a case conference afterwards. All the physicians thought the ECG was non-diagnostic. When my friend told them what I thought, they were dismissive.
It is the same as always: “If I can’t see it, it doesn’t exist.”
Which is why it is nice to have a neutral arbiter, like the Queen of Hearts:
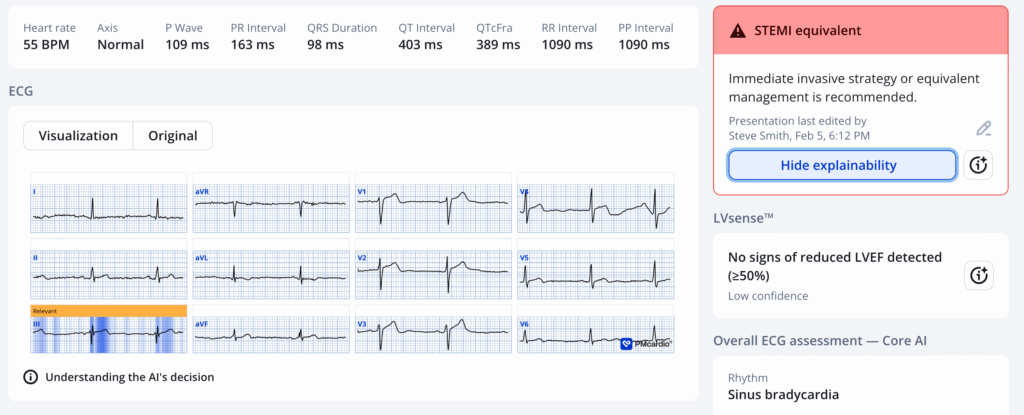
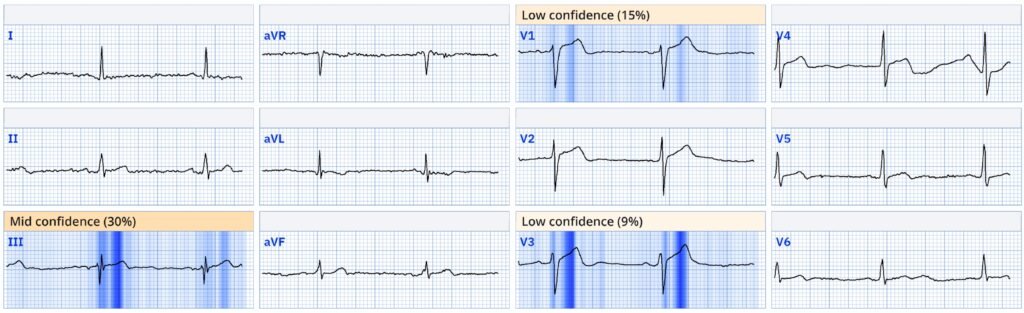
This ECG is DIAGNOSTIC of inferior injury. Troponins can only be trusted when the ECG is completely non-ischemic.
The Queen’s numerical output was 0.73. Values between 0.67 and 0.83 have 98% specificity. So she is VERY certain that this represents OMI (otherwise known as “STEMI Equivalent”)
Learning points:
- It’s not the ECG which is “Non-diagnostic”. It is the physician who is “Non-diagnostic”
- Just because you don’t see it, does not mean it is non-diagnostic.
- Everyone needs a LOT of humility. Seeing OMI in ECGs can be extremely hard and hardly anyone is truly expert at reading.
- Everyone needs the Queen of Hearts. It is the ECGs that appear normal to you which need the Queen the most, because those are the ones that will surprise you the most.
- The Queen is the result of years of our (Pendell and mine) passion for the ECG in Acute Coronary Occlusion, in my case for over 35 years.
New PMcardio for Individuals App 3.0 now includes the latest Queen of Hearts model and AI explainability (blue heatmaps)! Download now for iOS or Android. https://www.powerfulmedical.com/pmcardio-individuals/ (Drs. Smith and Meyers trained the AI Model and are shareholders in Powerful Medical). As a member of our community, you can use the code DRSMITH20 to get an exclusive 20% off your first year of the annual subscription. Disclaimer: PMcardio is CE-certified for marketing in the European Union and the United Kingdom. PMcardio technology has not yet been cleared by the US Food and Drug Administration (FDA) for clinical use in the USA.
= = =
======================================
MY Comment, by KEN GRAUER, MD (2/6/2025):
The events of today’s case are tragic. We need to learn from it.
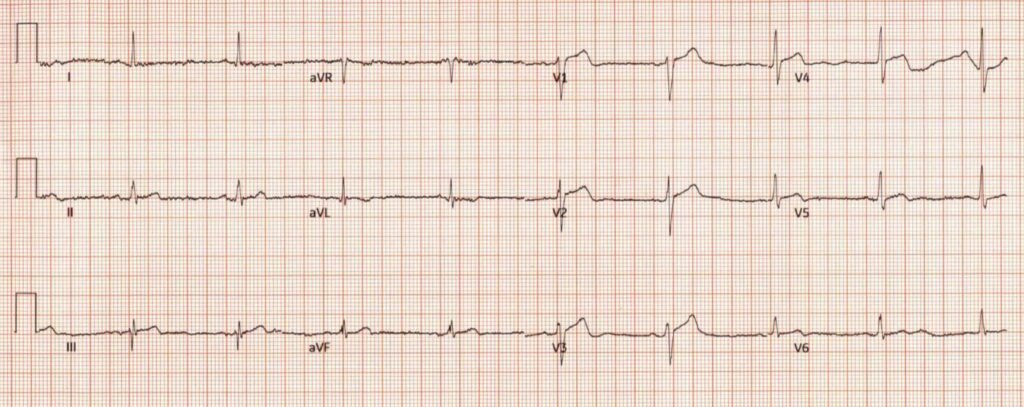
- Like Dr. Smith — I looked at today’s ECG with no information.
- Like Dr. Smith — I immediately saw that this ECG is not “normal”.
= = =
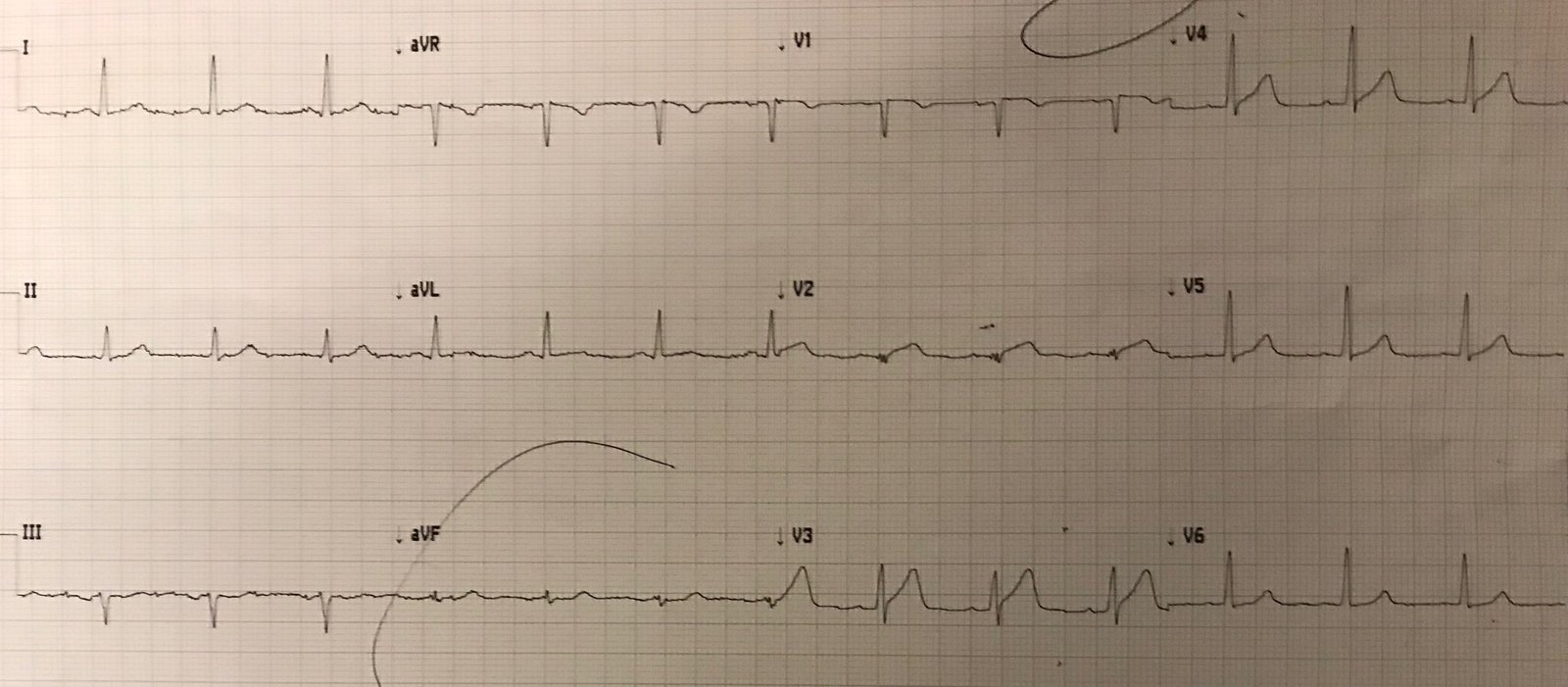
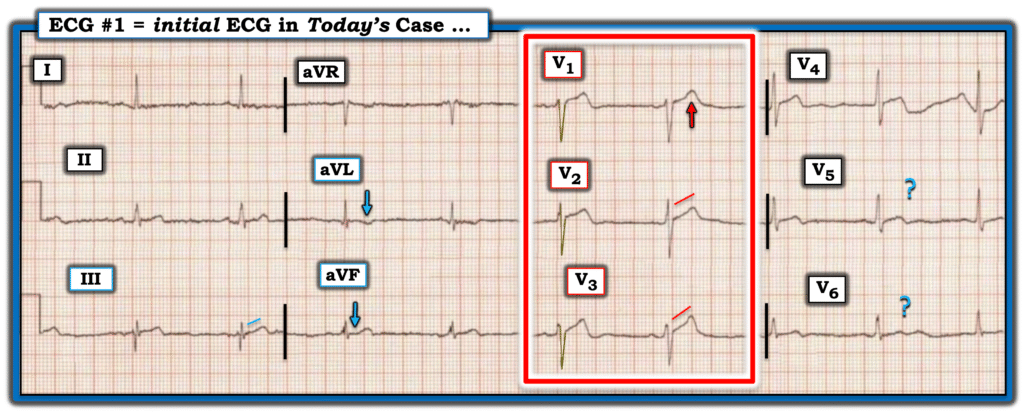
For clarity in Figure-1 — I’ve labeled potential findings of concern.
- To emphasize — As a single ECG, I thought this tracing was non-diagnostic, but potentially concerning pending more information. Clearly — A clinical history is needed.
- Subsequently learning that this 45-year old man presented to the ED for new CP (Chest Pain) should automatically increase our concern — since even before looking at the ECG, this immediately places this patient in a higher-risk group for having an acute event. This means that we need to be attentive to subtle findings that in an asymptomatic patient might not be significant.
- We need to remember that — a single ECG, even if seemingly “unremarkable” — does not rule out an acute event. This is because “pseudo-normalization” is commonly seen if an ECG is recorded in between the time that ST segments were elevated, and are now on their way toward developing the T wave inversion of reperfusion. Alternatively, a single ECG may be recorded shortly before acute ST-T wave changes develop.
= = =
ECG Findings of Potential Concern in Figure-1 …
Given the history of new-onset CP — I’ve noted a number of subtle-but-potentially-important findings in Figure-1:
- My “eye” was immediately captured by the ST-T wave appearance in leads V1,V2,V3 (within the RED rectangle). The KEY is proportionality — and I thought there was no way the disproportionately tall T wave in lead V1 could be “normal” in a patient with new CP, given the very modest size of the S wave in this lead.
- In support that the T wave in lead V1 is abnormal — is the subtle ST segment straightening in leads V2,V3.
- Artifact mars interpretation of leads V4,V5,V6 — yet it clearly appears that there is ST segment flattening in leads V5,V6 (if not, terminal T wave inversion at least in lead V5). In a patient with new CP and in association with my concerns about leads V1,V2,V3 — I wondered if these chest lead changes might not represent an early Precordial Swirl pattern?
- Further support that something acute might be ongoing is evident from ST-T wave appearance in the limb leads in Figure-1. Although the ST segment straightening in lead III is clearly subtle — there is no denying the abnormal T wave inversion in lead aVL (BLUE arrow in this lead).
- In the context of these findings in leads III and aVL — I interpreted the ST segment flattening in lead aVF (BLUE arrow) as also abnormal.
- Although the ST-T wave flattening in lead I is clearly nonspecific — I thought it might be of similar significance as the ST-T wave flattening in the lateral chest leads.
= = =
Figure-1: The initial ECG in today’s case.
= = =
My Bottom Line re Today’s ECG:
While important to emphasize that the above described findings in Figure-1 are subtle and non-diagnostic when viewed in isolation — in today’s patient who presents to the ED with new-onset CP — I interpreted ST-T wave findings in leads V1,V2,V3 and aVL as abnormal until proven otherwise. And, in that context — I interpreted the ST-T wave appearance in no less than 9/12 leads as potentially consistent with an acute OMI until proven otherwise.
- We are told that 2 high-sensitivity Troponin values were each 24 ng/L. Assuming an upper normal limit of 20 ng/L for men — these repeat values of 24 ng/L would not be “normal”, but elevated. Even slight Troponin elevation is significant in a patient with new CP and potentially concerning ECG findings as are seen in Figure-1.
- That said — norms for hs-Troponin may vary depending on the institution and specific assay used. But regardless of whether or not one or both of these 2 hs-Troponin assays are elevated — this would not rule out the possibility of an acute OMI (ie, hs-Troponin might not become elevated despite acute coronary occlusion IF the period of occlusion is brief — See this Search in Dr. Smith’s ECG Blog for cases with Normal Troponin).
- To quote Dr. Smith, “Using Troponin to diagnose acute coronary occlusion is like relying on a rear-view mirror to navigate a car pile-up: It shows wreckage behind you that has already happened, but can not see the road ahead.” As a result — “A normal initial Troponin can give false reassurance, when there’s a head-on collision happening in real time!” (from the March 24, 2023 post).
= = =
Learning Points:
- Regardless of whether or not the first 2 hs-Troponin assays are normal — A single normal ECG does not rule out an acute ongoing event.
- In a patient who presents to the ED with new-onset CP — suspicious findings on an initial ECG are often all that is needed to justify activating the cath lab.
- IF in doubt about whether the initial ECG is “normal” (as providers in today’s case were) — then repeat the ECG! Waiting 10 (at most 20) minutes will often be all that is needed to demonstrate “dynamic“ ST-T wave changes that prove your patient is in process of evolving an acute OMI.
- Given the history of new CP — today’s initial ECG should have been enough to activate the cath lab at that time. Had this been done — perhaps the outcome of today’s case may have been different.
= = =
= = =