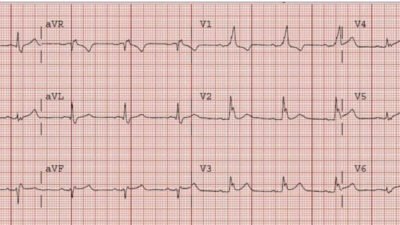
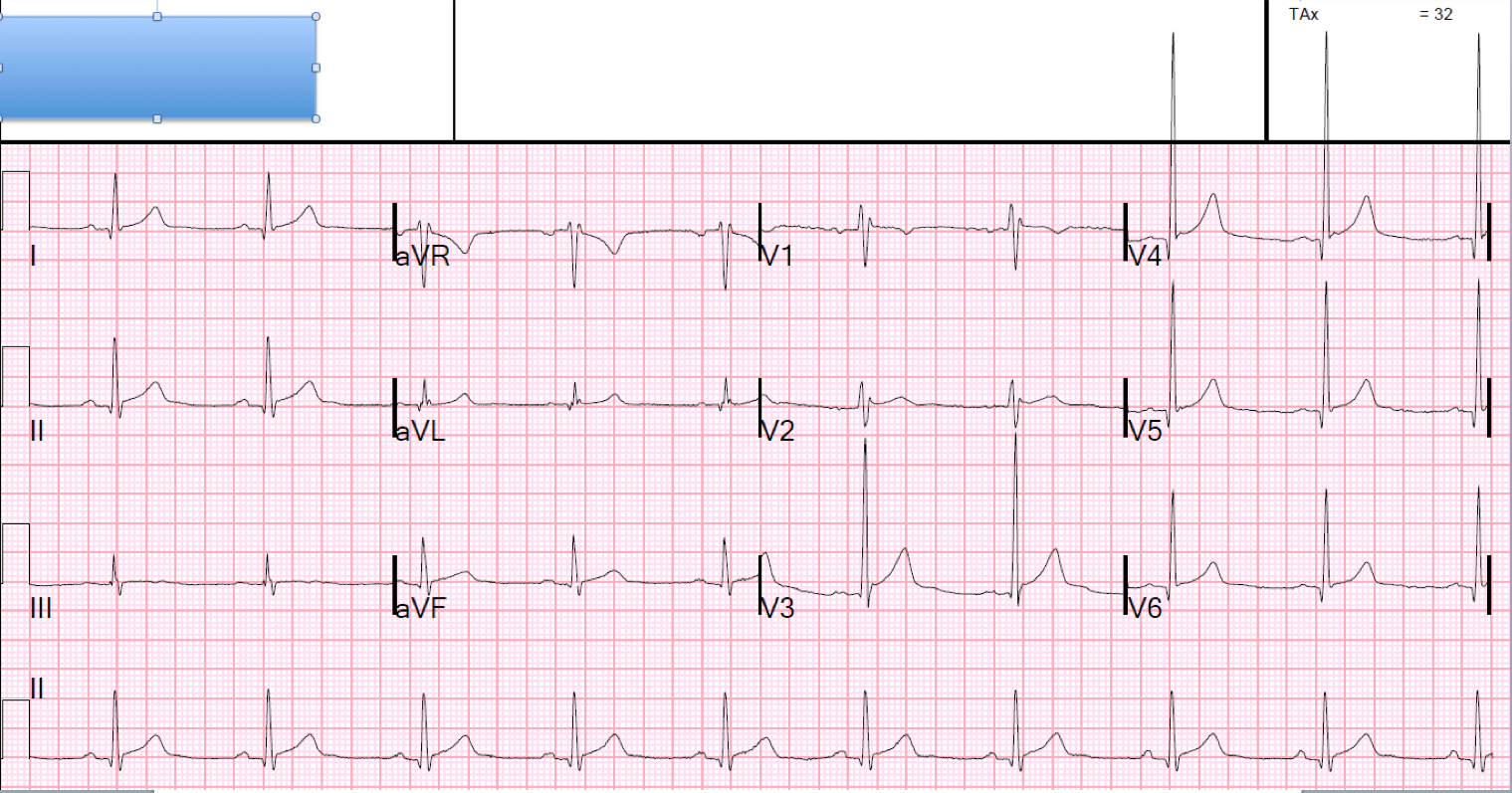
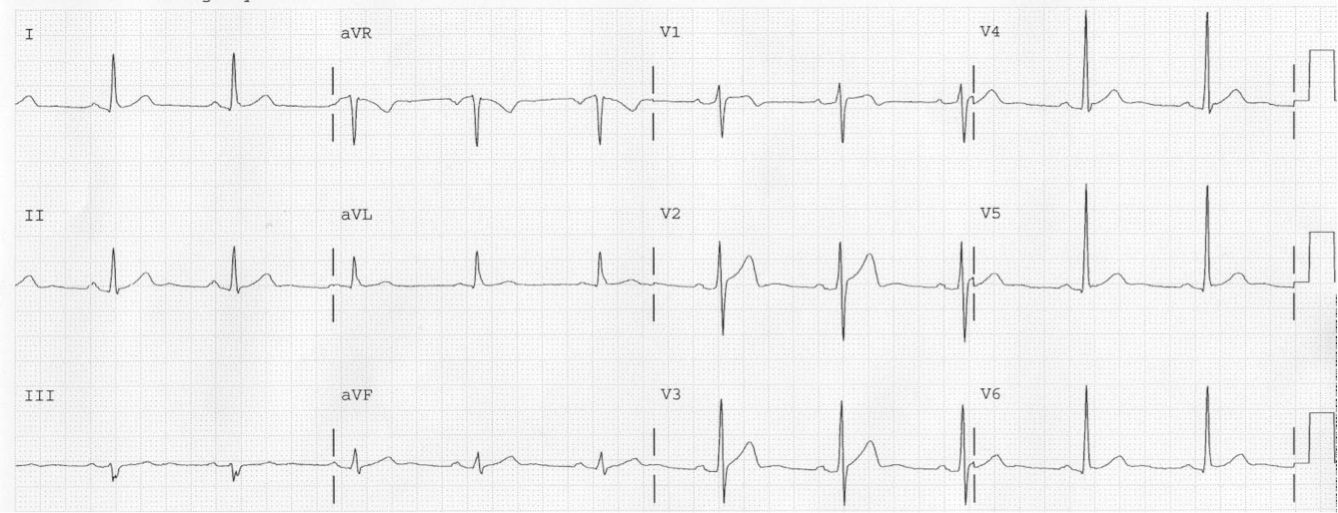
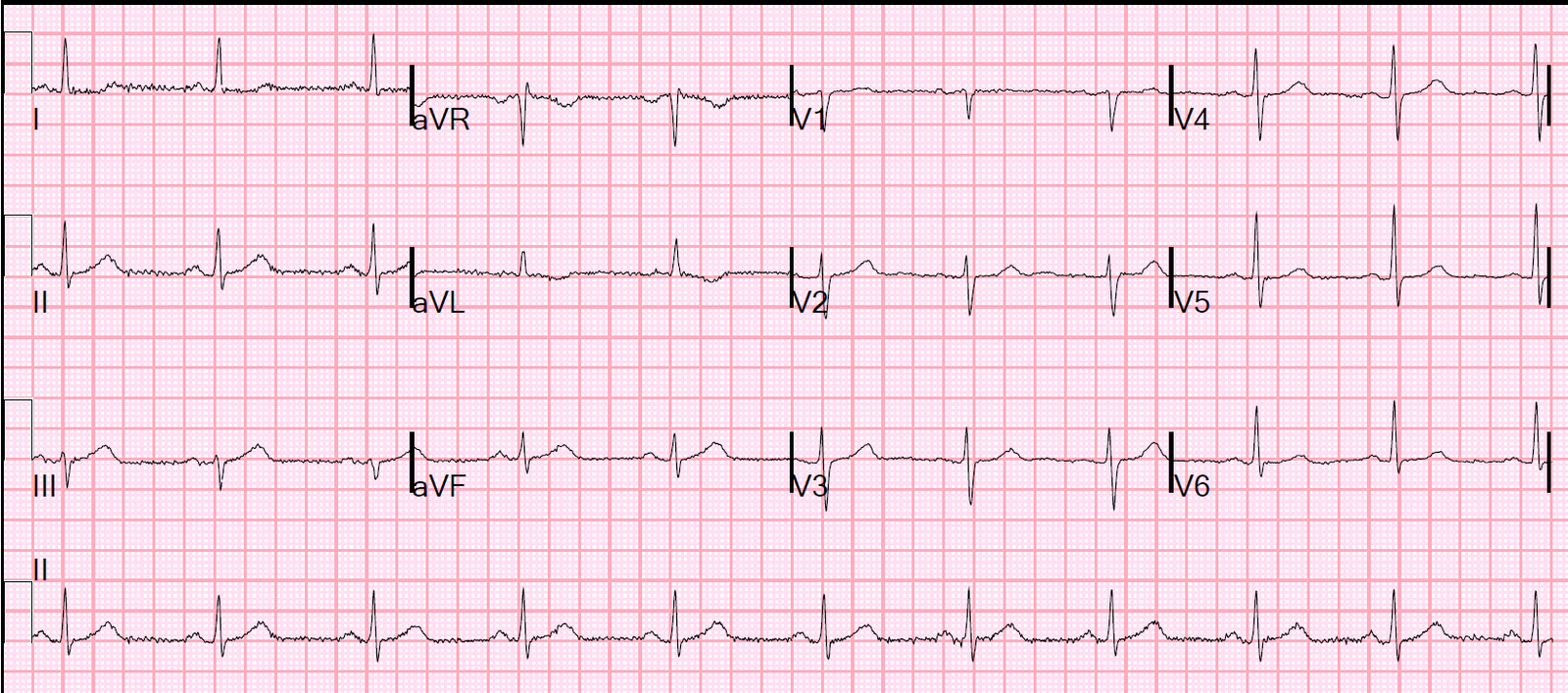
This is my most popular lecture, which Scott Joing of www.hqmeded.com just recorded for me in his amazing video recording studio.
When I give this lecture real-time, I usually do it in a workshop and have more time – enough time to stop and let people get a good look at the ECG and try to find the critical elements for themselves before going on to explain them. That makes for a significantly longer lecture.
But if you want to have time to scrutinize any ECG, just pause the video to look at the ECG for a while before you play my explanation.