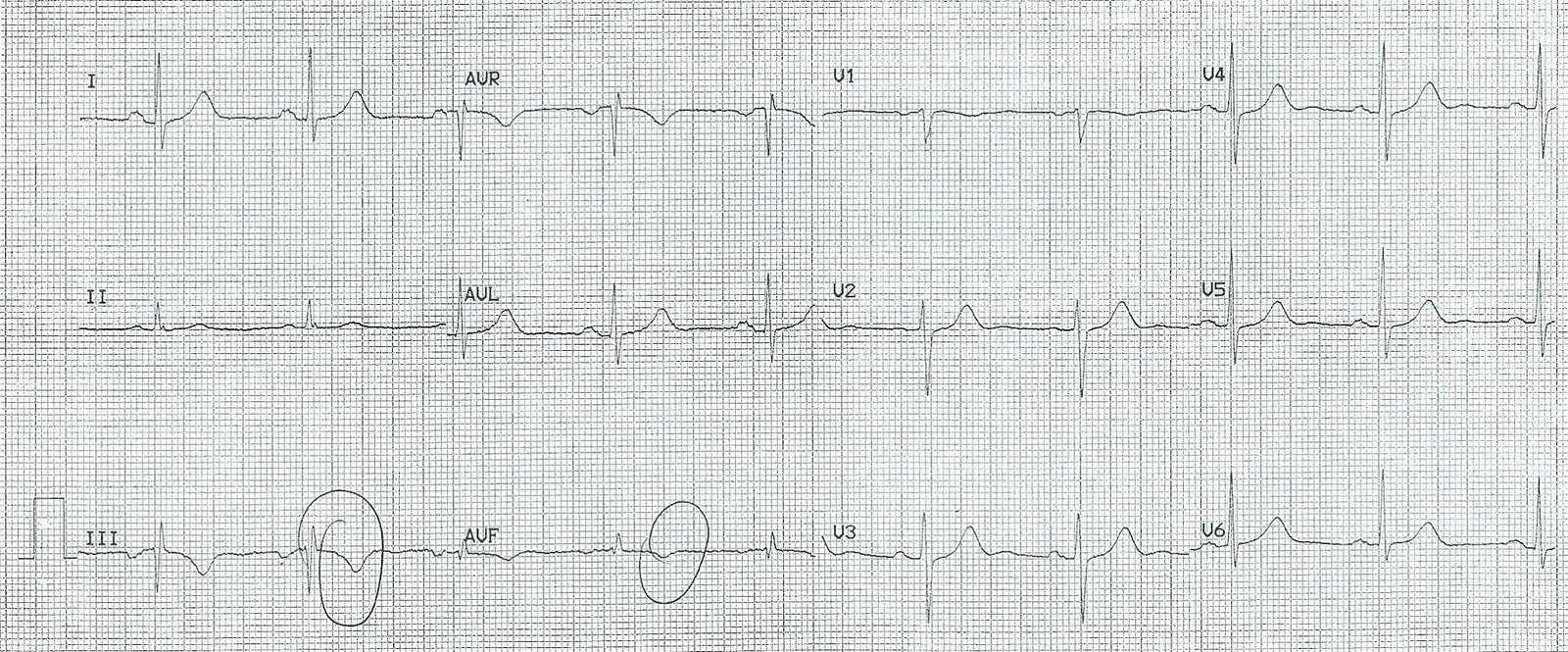
This 69 yo male with a history of HTN, but no h/o CAD, presented with chest pain at an outside hospital at 1700 hours with chest pain onset at approx 3 PM. Here is the first ECG, at 1720:
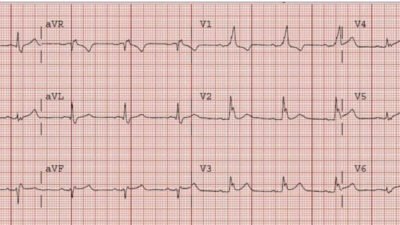
The patient received nitroglycerin, and became pain free. A second ECG was recorded at 1739:
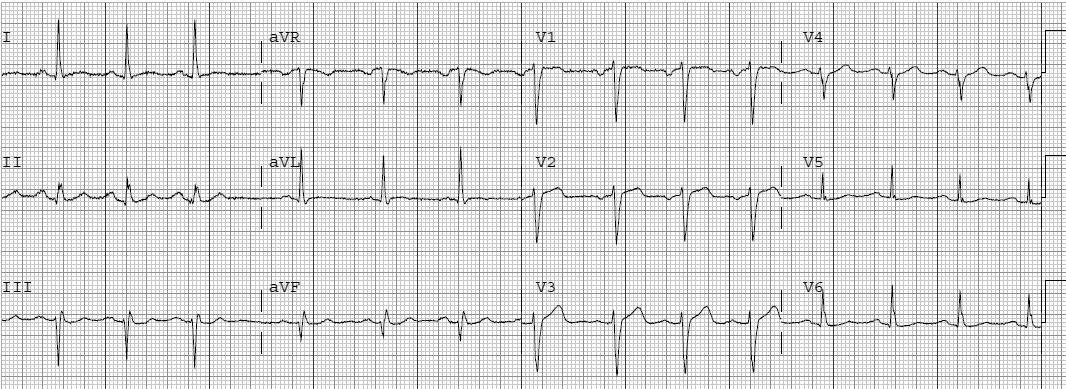
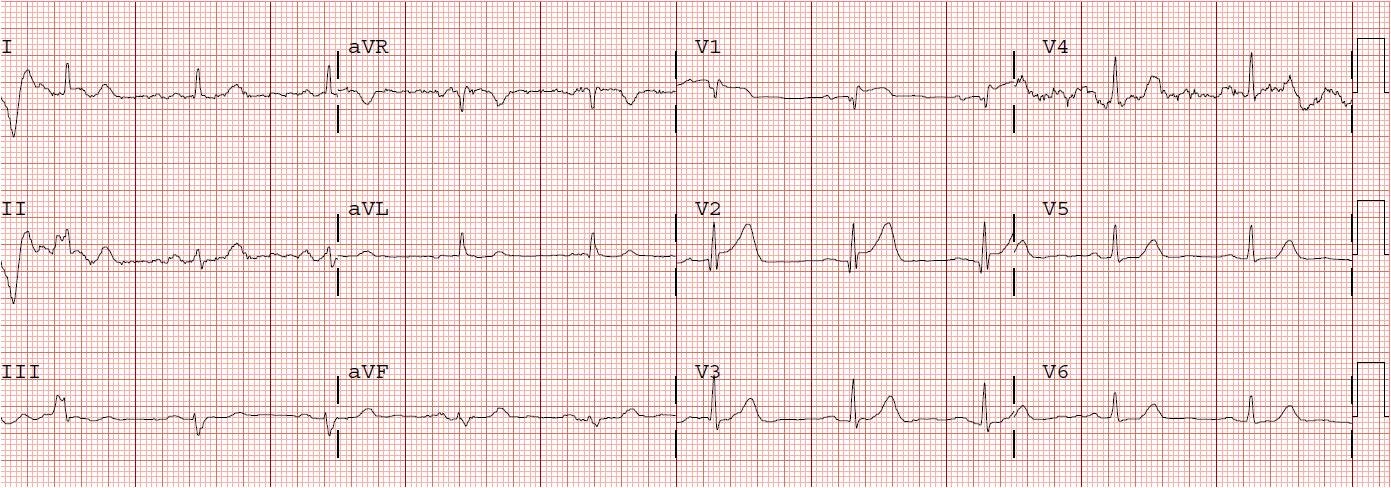
The patient was put on heparin and eptifibatide and transferred to our institution. Here, he remained pain free. His initial Troponin I was 16 ng/ml. A 3rd ECG was recorded at 2202:
 |
||
| The ST depression in precordial leads is gone. The biphasic T-wave in aVL remains, with an abnormal reciprocal ST segment in lead III. |
At 0032 another ECG was recorded:
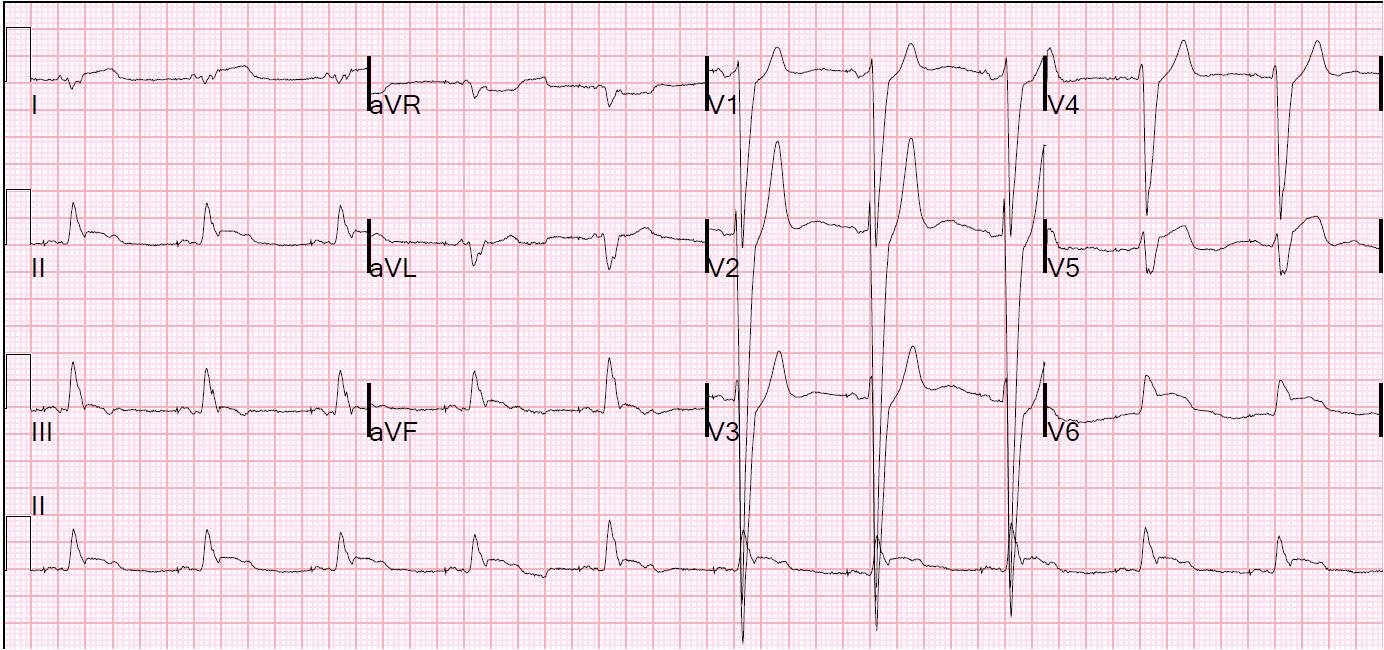
Here is another example of posterior reperfusion T-waves:
https://drsmithsecgblog.com/2010/12/computer-misses-again-two-cases-one.html
The next AM the patient went into atrial fib with RVR:
He was taken for cath and had a 100% occlusion of a large 1st obtuse marginal (circumflex). Ultrasound confirmed a posterolateral wall motion abnormality. The troponin peaked at 74, went down, then went back up to 180 after the atrial fib, and down again.