This young woman presented with atypical chest pain, often severe, for 10 days. MI was ruled out and an alternative diagnosis was made by chest x-ray, then MRI, and this alternative diagnosis appeared to explain the symptoms. However, it did not:
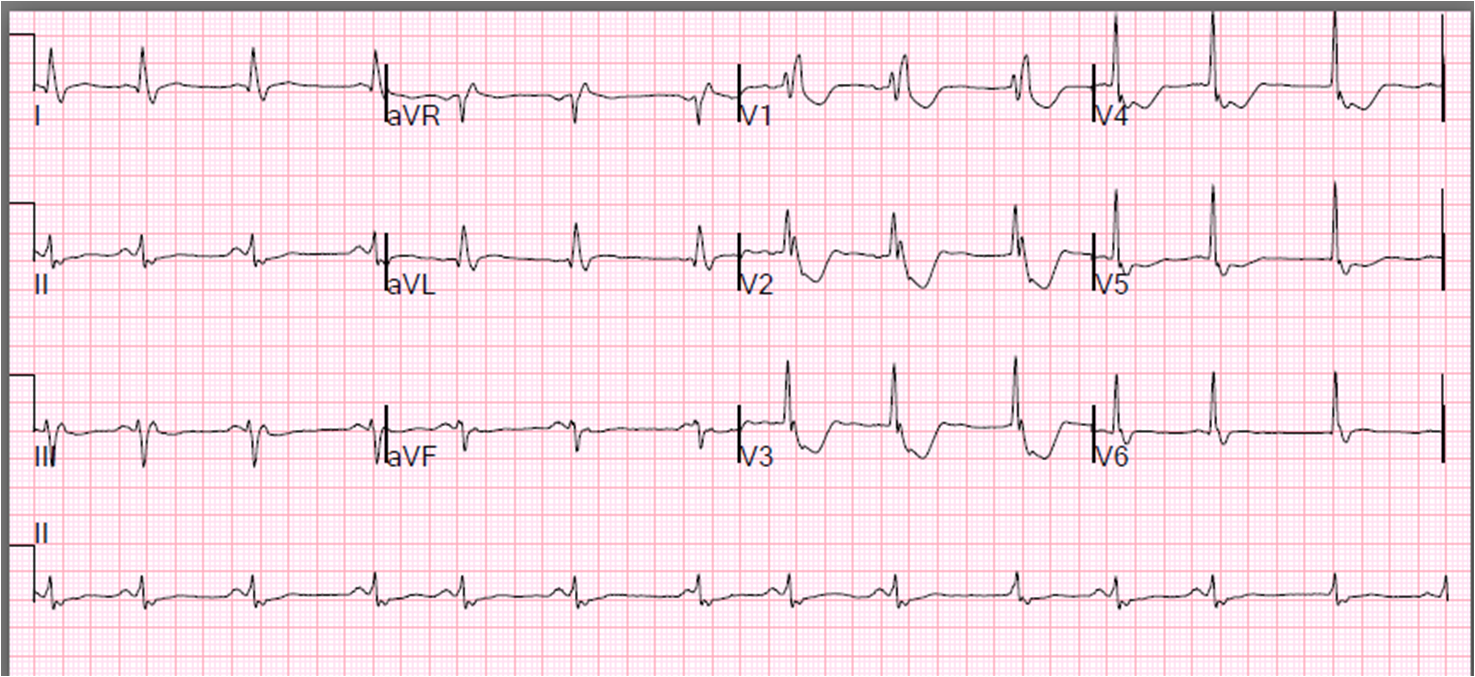
On day 1 (10th day of symptoms), she had this ECG:
 |
| There is slight ST elevation in leads I, II, aVL and aVF. There is no STE in III. There is no recipocal ST depression. This is consistent with either normal ST elevation or pericarditis |
On day 2, she had an echocardiogram which showed a very small pericardial effusion.
On day 3, she had this ECG:
Pericarditis is usually diffuse (not localized to any one wall), with
all walls equally involved. Since the apex of the heart is directed
anterior and lateral and slightly inferior, all those ST vectors add up and the ST axis is in those directions. Thus, there is no reciprocal ST depression except for aVR (which is always reciprocal to other limb leads). The PR depression, which is 1 mm in leads I, II, and V3 is very specific for pericarditis. Spodick found in his series that 0.8 mm or more was specific. The best cutoff, and the respective sensitivities and specificities, are not exactly known. But it is important to remember that the normal Ta wave results in normal PR depression.
On day 5, a friction rub was heard and her heart rate was elevated at 110, but she had no increase in symptoms. She had this ECG recorded:
 |
| The STE is more pronounced, which could be due to the increasing effect of pericarditis, or to the increased heart rate. |
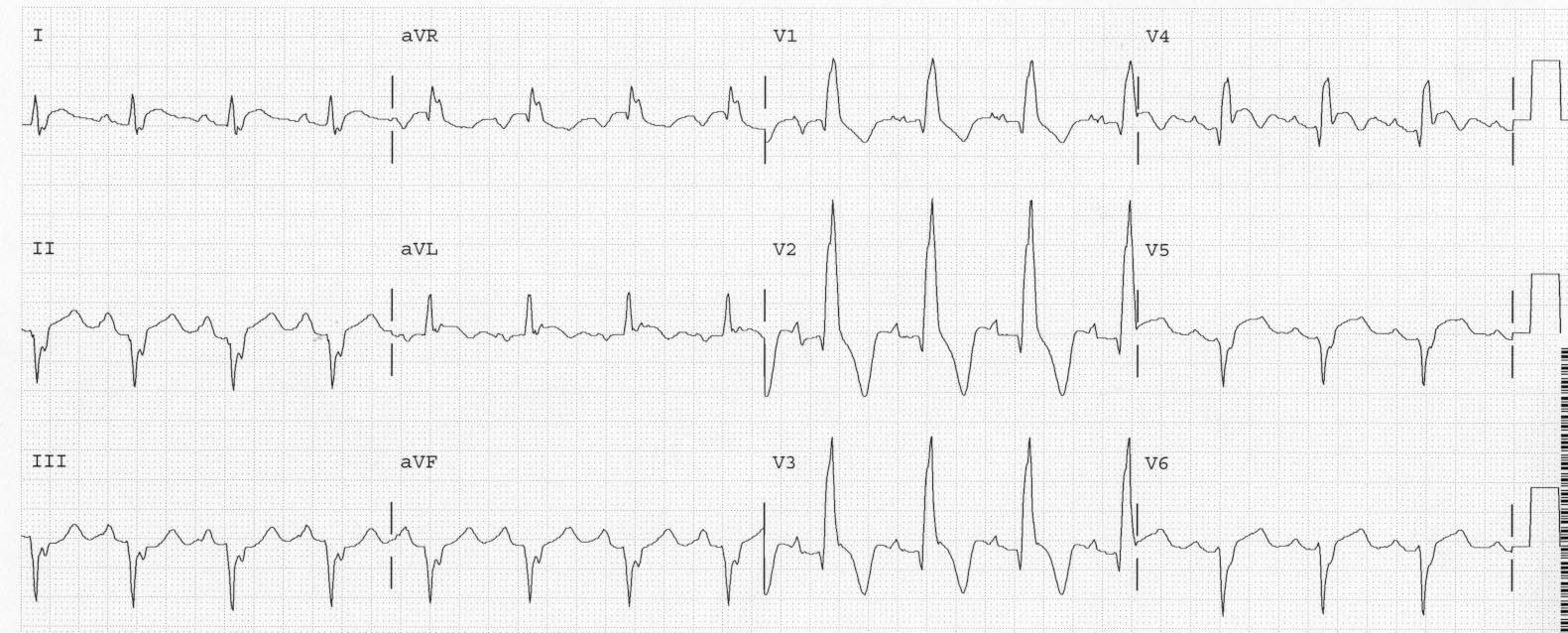
On day 6, her heart rate elevated to 135 and she had this ECG:
 |
| There is not also some subtle electrical alternans, which is a sign of tamponade (it does not occur in effusion without tamponade, at least not often) |
An echo showed a very large effusion and tamponade physiology. She underwent pericardiocentesis. It was idiopathic pericarditis. She did well.