A 26 year old male presented with syncope and chest pain. Syncope was sudden and without prodrome, and resulted in head trauma with a scalp laceration.
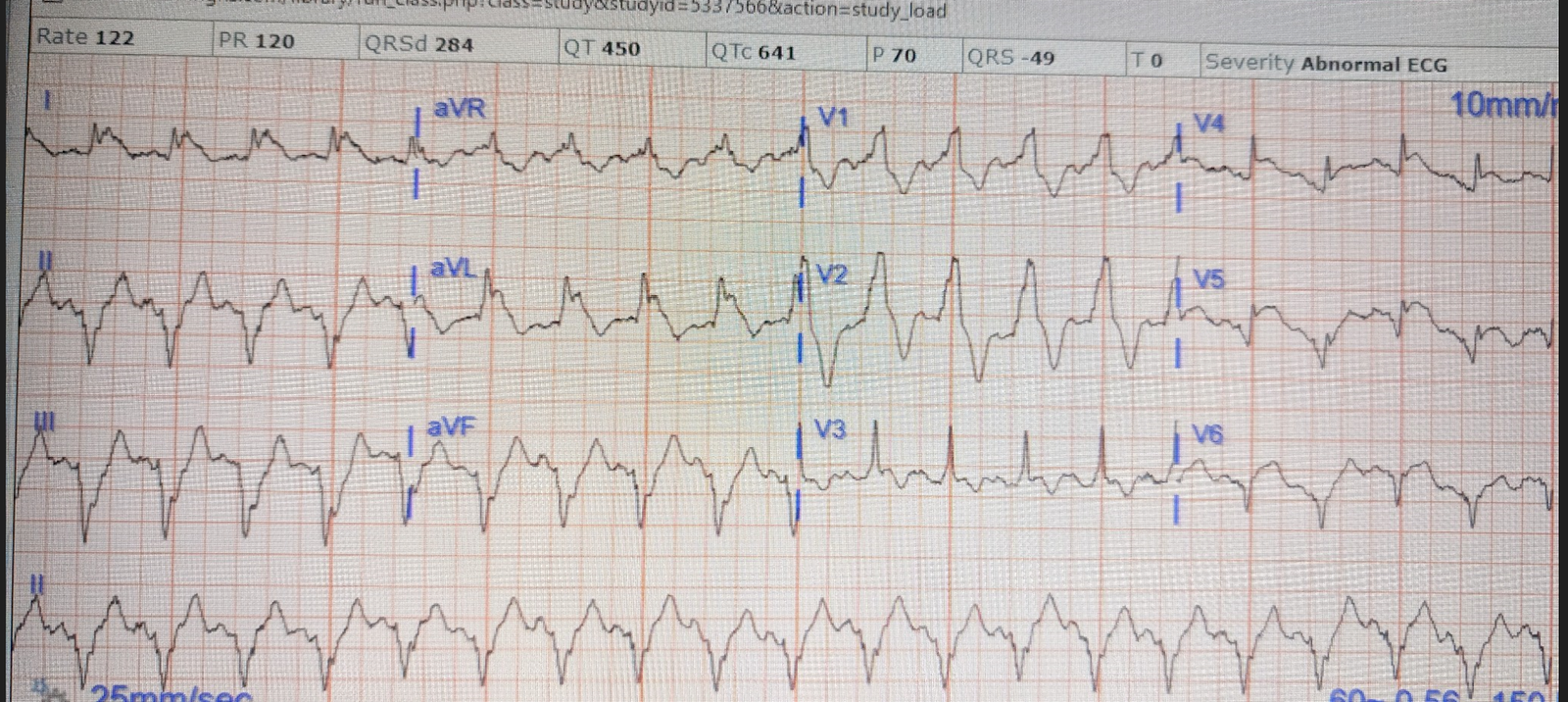
Here is his ECG:
There is significant ST Elevation in inferior leads, with reciprocal ST depression in aVL.
This appears to be an inferior OMI
What do you think?
Smith: I recognize this as a STEMI mimic. I was not alarmed. The providers showed me the ECG and I told them that I thought it was a fake. It is a sad fact that although pericarditis with STE in inferior leads rarely has reciprocal ST depression in aVL, normal variant ST Elevation sometimes does manifest STD in aVL
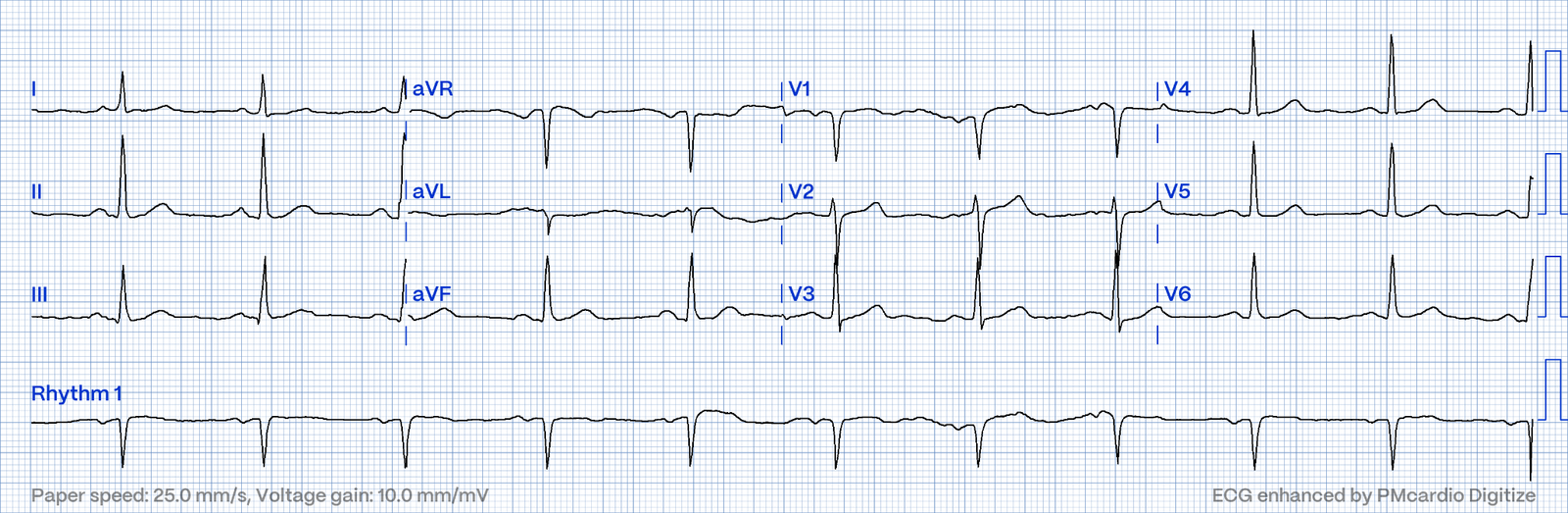
He had a previous ECG on file from one year prior:
There is some abnormal atrial activation, but no ST Elevation
Does this mean that the new one is necessarily due to OMI/ischemia?
No.
What does the Queen of Hearts think?
“No signs of OMI”
The chest pain resolved after some time, and another ECG was recorded:
The ST Elevation is nearly gone.
Doesn’t this necessarily mean that he was having ischemia?
Unfortunately, life is not so simple. I recognize this as a normal variant. Amazingly, the Queen also recognizes it as “Not OMI”. She is very good.
The first troponin was < 3 ng/L. The 2 hour troponin was < 3 ng/L.
He was admitted for monitoring and had no dysrhythmias.
He had a formal contrast echo that was completely normal:
Normal estimated left ventricular ejection fraction; 69%.
No left ventricular wall motion abnormality identified.
Normal LV cavity size and borderline wall thickness.
Normal right ventricular size and function.
No hemodynamically significant valvular abnormalities.
I want to emphasize that it is not the patient’s age which made me think the ECG was a mimic. It was the ECG morphology. The queen does not know the patient’s age. And I have long warned doctors that young people have acute MI and OMI.
Especially, if a young woman has OMI, she is likely to be disregarded with a “Nah, couldn’t be OMI!”
See here for young women with OMI
===================================
MY Comment, by KEN GRAUER, MD (1/9/2025):
===================================
I found today’s case challenging — and an excellent example of how despite my not being certain of the diagnosis from the history and initial ECG — careful follow-up yielded the answer.
- To facilitate comparison in Figure-1 — I’ve put together the 3 ECGs from today’s case.
Why I was Uncertain about ECG #1
I found today’s initial ECG and the history to be study in contrasts.
- The history of syncope that was sudden and without prodrome, and severe enough to result in head trauma on falling — is concerning. The most common cause of syncope in a previously healthy young adult like today’s patient — is vasovagal syncope. But vasovagal syncope typically has a prodrome — such that further evaluation of today’s patient may be needed as an outpatient to better assess for the cause of his sudden syncope.
- Concern about this patient’s initial ECG was enhanced by the history of “chest pain” — although: i) We are not told the specifics regarding this chest pain (ie, Whether or not this truly was cardiac-sounding CP?); — but, ii) In a previously healthy 26-year old man — syncope is not a common accompaniment of an acute MI.
Regarding the initial ECG:
- There is no denying the presence of nearly 2 mm of ST elevation in each of the inferior leads. In addition, there appears to be some ST segment straightening in these inferior leads — which adds to potential concern in a patient with CP.
- That said, there were features less commonly seen with acute OMI. These included subtle J-point notching in each of the inferior leads (typically a benign finding) — with a QTc that looked relatively short — and a “funny-looking” ST-T wave shape that did not necessarily look acute despite the ST elevation.
- I was not convinced that lead aVL was showing “reciprocal” ST depression — as the T wave vector often follows closely behind that of the QRS, such that the very shallow T wave inversion in aVL in which the QRS was essentially all negative might be a normal finding.
- Finally — I added question marks over the ST-T waves in leads V1,V2,V3 because the progression of the QRS and ST-T waves did not make sense. That is — the R wave decreases from V1-to-V2, but then increases from V2-to-V3 — and the ST segment suddenly becomes flat in lead V2, before abruptly becoming quite large in lead V3 (which interestingly manifests a similar amount of ST elevation and a similar ST-T wave shape as is seen in the inferior leads). At the least — I thought there may be some lead malposition. But the shape of the ST-T waves in these 3 anterior leads certainly did not suggest posterior OMI, which is such a common accompaniment IF there is ongoing inferior OMI.
BOTTOM Line about ECG #1: There is no denying that despite the young adult age of this patient — he presented to the ED with chest pain and syncope — and his initial ECG shows nearly 2 mm of ST elevation in each of the inferior leads.
- I wondered if there might be more details in the history that could suggest acute myocarditis, which could be a better “fit” than an acute OMI for the findings in ECG #1.
- I felt more evaluation was needed before being able to completely rule out an acute event.
 |
| Figure-1: I’ve labeled the the 3 ECGs in today’s case. |
A Previous ECG is Found:
Optimal comparison of serial ECGs is best performed by placing both tracings side-by-side, as I have done in Figure-1.
- There is no denying the change in appearance between ECG #2 (done ~1 year earlier) — and today’s initial tracing ( = ECG #1). There is virtually no ST elevation on the earlier tracing — and the T wave is clearly upright in lead aVL.
- Of interest, upward sloping ST elevation with J-point notching (BLUE arrows) is seen in ECG #2 (that was done a year earlier) — whereas these findings are not seen in leads V2,V4,V5,V6 of today’s initial ECG. Considering the normal R wave progression — plentiful QRS amplitude — and the 6 BLUE arrows highlighting J-point notching in ECG #2 — this previous tracing is typical of a repolarization variant.
The ECG is Repeated:
The 3rd ECG in today’s case appears at the bottom of Figure-1.
- With the exception of now manifesting a nice normal sinus P wave and a slightly faster heart rate — ST-T wave morphology in ECG #3 looks very similar to that in baseline ECG #2.
- Comparing ECG #3 to the initial ECG in today’s case — the inferior lead ST elevation has resolved — the T wave in lead aVL is now clearly upright — and upward sloping ST elevation with J-point notching is more prominently seen in the chest leads.
Putting the Case Together:
In this young adult man who presented to the ED for chest pain and syncope — the ST elevation manifest on his initial ECG resolved while he was in the ED undergoing evaluation.
- That said, rather than reperfusion changes of an evolving OMI — the principal change between ECG #1 and the repeat ECG ( = ECG #3) is reestablishment of the repolarization variant pattern that was seen on this patient’s baseline ECG.
- Troponins were negative.
- Overnight telemetry showed no arrhythmias (important to reduce the risk of worrisome arrhythmia given this patient’s chief complaint of sudden syncope without prodrome).
- Formal contrast Echo showed normal LV function without wall motion abnormality.
- The patient was discharged home.
Learning Points:
- There are features in today’s patient’s initial ECG that are not typical for an acute OMI. Despite this — given the presentation to the ED of chest pain and ST elevation — “Prudence is the better part of valor” — so a period of monitoring during evaluation with Troponins, repeat ECG and Echo were indicated to attain 100% comfort before discharge the next day.
- The ST-T wave appearance in repolarization patterns is not always constant. Instead, the ST-T wave appearance may change in serial tracings recorded over the course of a single ED visit. Although this is not a common phenomenon — You will see it on occasion (See the June 30, 2023 post — the November 27, 2023 post — and the July 24, 2013 post in Dr. Smith’s ECG Blog). As in today’s case — the potential for the ST-T wave appearance of repolarization patterns to vary can be easily confused with “dynamic” ECG changes indicative of an acute evolving OMI.
- Greenfield and Rembert have noted that up to 1/3 of patients with ER (Early Repolarization) but no cardiac symptoms — may show marked variation in the amount of ST elevation from one tracing to the next. These ER patients do not have ischemia — and the variation in ST elevation has not been shown to be related to either heart rate or QRS amplitudes (Variation in ST-Segment Elevation in Early Repolarization: Electrocardiography 40:10,2007).