Written by Jesse McLaren
Two 70 year olds had acute chest pain with nausea and shortness of
breath, and called paramedics. Who needs the cath lab?
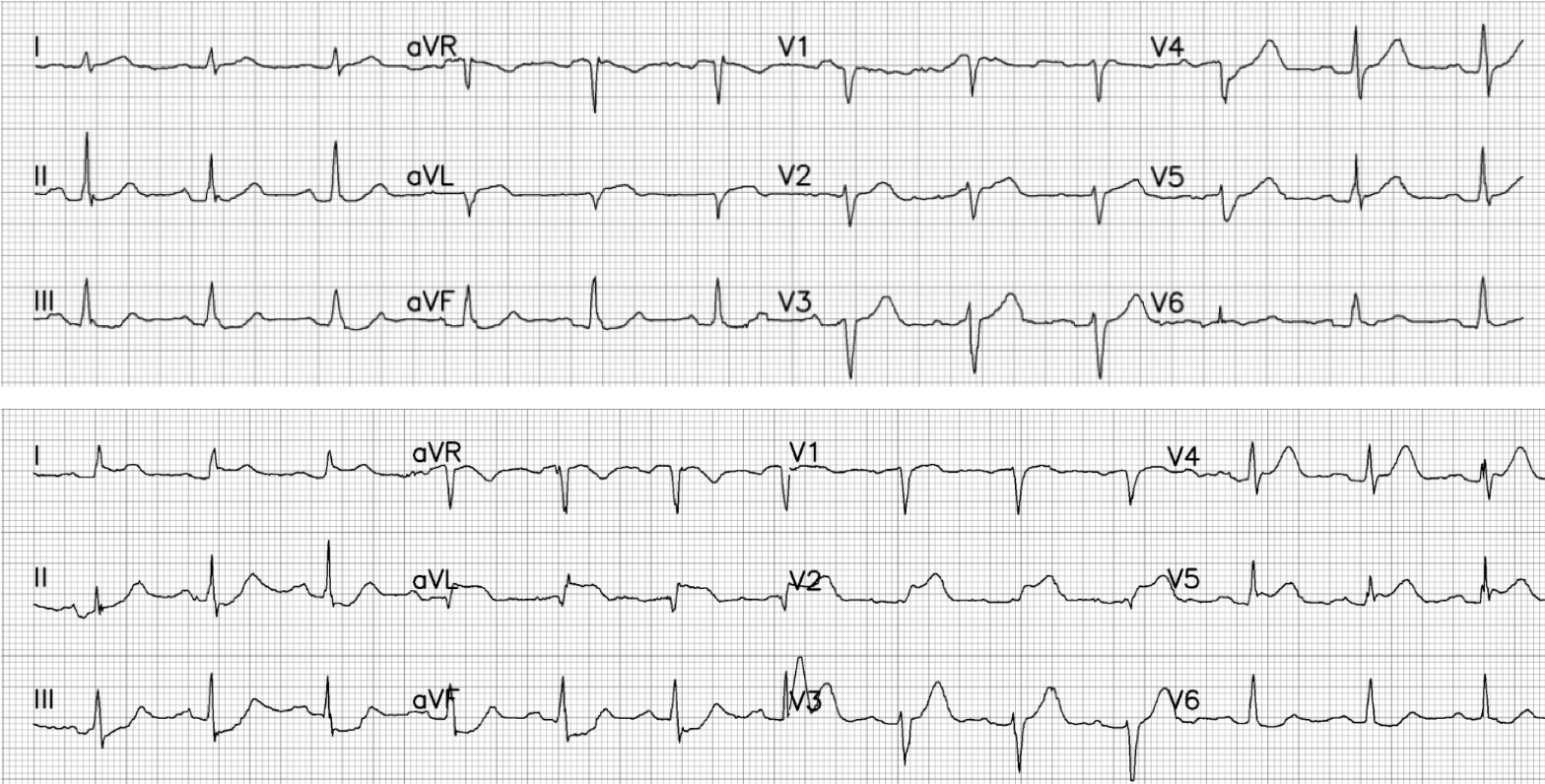
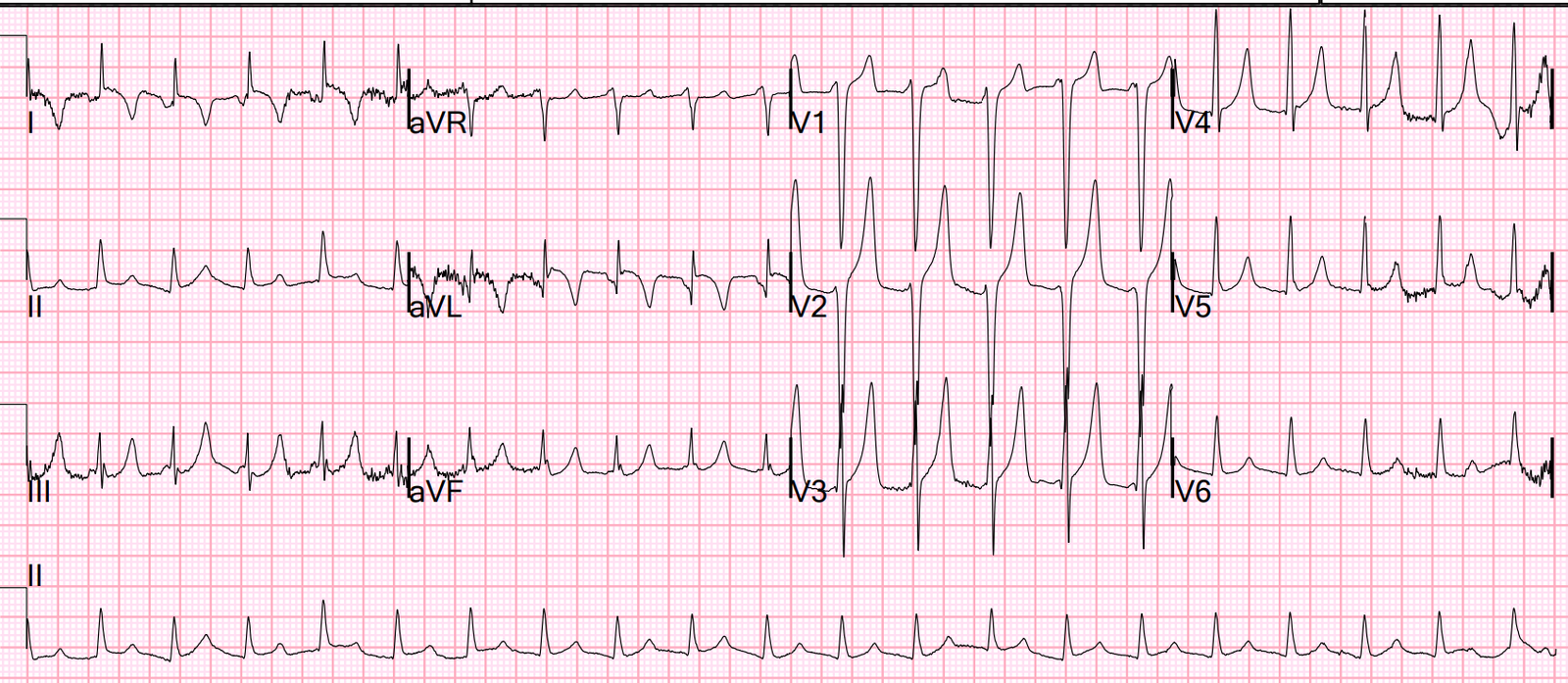
(photocopy of prehospital ECGs digitized by PMcardio)
ECG #1 (top): there’s normal sinus rhythm, normal conduction,
normal axis, normal R wave progression, and normal voltages. There’s inferior
ST depression which is reciprocal to subtle lateral convex ST elevation, and
the precordial T waves are subtly hyperacute – all concerning for STEMI(-)OMI
of proximal LAD.
ECG # 2 (bottom): there’s sinus rhythm with normal conduction, normal
axis, loss of R wave in V2, normal voltages. There’s ST elevation I/aVL/V2 that
meet STEMI criteria. There’s also hyperacute T waves V2-4, ST depression
inferiorly which is reciprocal to lateral ST elevation, and ST depression in V6
reciprocal to subtle ST elevation in V1 (swirl sign). This is obvious
STEMI(+)OMI of proximal LAD.
This case illustrates three common pitfalls of the STEMI paradigm, which can be improved by OMI ECG findings:
1. STEMI on serial ECG,
or OMI from the start?
According to the STEMI paradigm, ECG #1 is nondiagnostic
whereas ECG #2 is STEMI. So the first patient doesn’t need emergent reperfusion
whereas the second does. But these ECGs were from the same patient: #1 on
paramedic arrival and #2 thirty minutes later. The patient’s LAD was occluded from the start even
though the first ECG didn’t manifest STEMI criteria.
I sent the first ECG to Dr. Meyers without any information,
and he replied, “good one. OMI. Will be missed easily.” Indeed, in his study
comparing accuracy of OMI vs STEMI findings, more than half of OMIs were STEMI
negative but diagnostic of OMI, and could be identified a median of 1.5 hours
earlier, and the two most common OMI ECG findings were “subtle STE not meeting STEMI criteria” and “reciprocal ST depression and/or reciprocal T wave inversion”.[1] So even for true positive STEMIs, identifying OMI can help expedite
reperfusion.
Thankfully this patient’s second ECG met STEMI criteria, so
paramedics brought them as a code STEMI. This seems to validate the STEMI
paradigm because serial ECGs arrived at the diagnosis. Looking at ECG #1 and 2 it could look like a simple case of evolving STEMI, even if the first is not recognized as LAD occlusion. But what if the second
ECG hadn’t been recorded at that exact moment?
2. Non-STEMI or
STEMI(-)OMI?
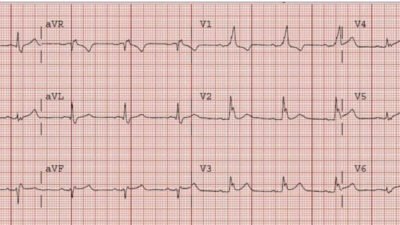
Three minutes later, paramedics recorded a third ECG. Below is ECG #1 and ECG #3:
ECG #3 no longer meets STEMI criteria, but is still
diagnostic of proximal LAD occlusion (and shows subtle loss of R waves V2-4). If the patient only had these two ECGs recorded, it would have missed the transient time between them which were STEMI positive, and the patient would then have arrived at the ED as “serial ECGs STEMI negative.” With an elevated troponin, ECGs like are often be misinterpreted as “inferior ST depression” and then labeled “non-STEMI”, but ST depression doesn’t localize and the inferior ST depression is reciprocal to subtle lateral ST elevation/hyperacute T waves. This puts OMI patients at risk for delayed reperfusion—like more than a quarter of “non-STEMIs” with totally
occluded arteries, most of which can be identified by OMI signs.[2]
Transient STEMI, or
ongoing OMI?
If we look at ECG #2 and #3, another pitfall emerges:
according to the STEMI paradigm, the patient had a “transient STEMI” because
their ECG has gone from STEMI positive (#2) to STEMI negative (#3).
According to the interpretation of some
trials, patients with transient STEMI don’t need emergent reperfusion.[3] But ‘transient
STEMI’ requires complete resolution of symptoms and ECG changes, and delaying
cath lab for patients with spontaneous reperfusion puts them at risk for
reocclusion.[4] But this patient hasn’t even spontaneously reperfused, because
their ECG shows ongoing LAD occlusion even though it no longer meets STEMI
criteria.
This routine case was a near miss, and shows three common pitfalls of the STEMI
paradigm:
1.
ECG #1-2, from STEMI(-)OMI to STEMI(+)OMI:
risk of delayed diagnosis of true positive STEMI, when diagnostic of OMI from the start
2.
ECG #1/3, STEMI(-)OMI: risk for false
negative STEMI and admission as Non-STEMI, despite serial ECGs showing OMI
3.
ECG #2-3, from STEMI(+)OMI to STEMI(-)OMI: risk
of delayed reperfusion for transient STEMI when there’s ongoing OMI
Two factors expedited reperfusion for this patient: ECG #2 met
STEMI criteria so code STEMI was activated from the field, and even though STEMI criteria
resolved the patient had a VF arrest on arrival, after which they were defibrillated
and taken immediately to the cath lab. There was 100% proximal LAD occlusion,
EF was 55% with severe hypokinesis to mid-distal septum and apex. First
troponin I was 150 ng/L (normal <26 in males and <16 in females) and peak
was 7,500.
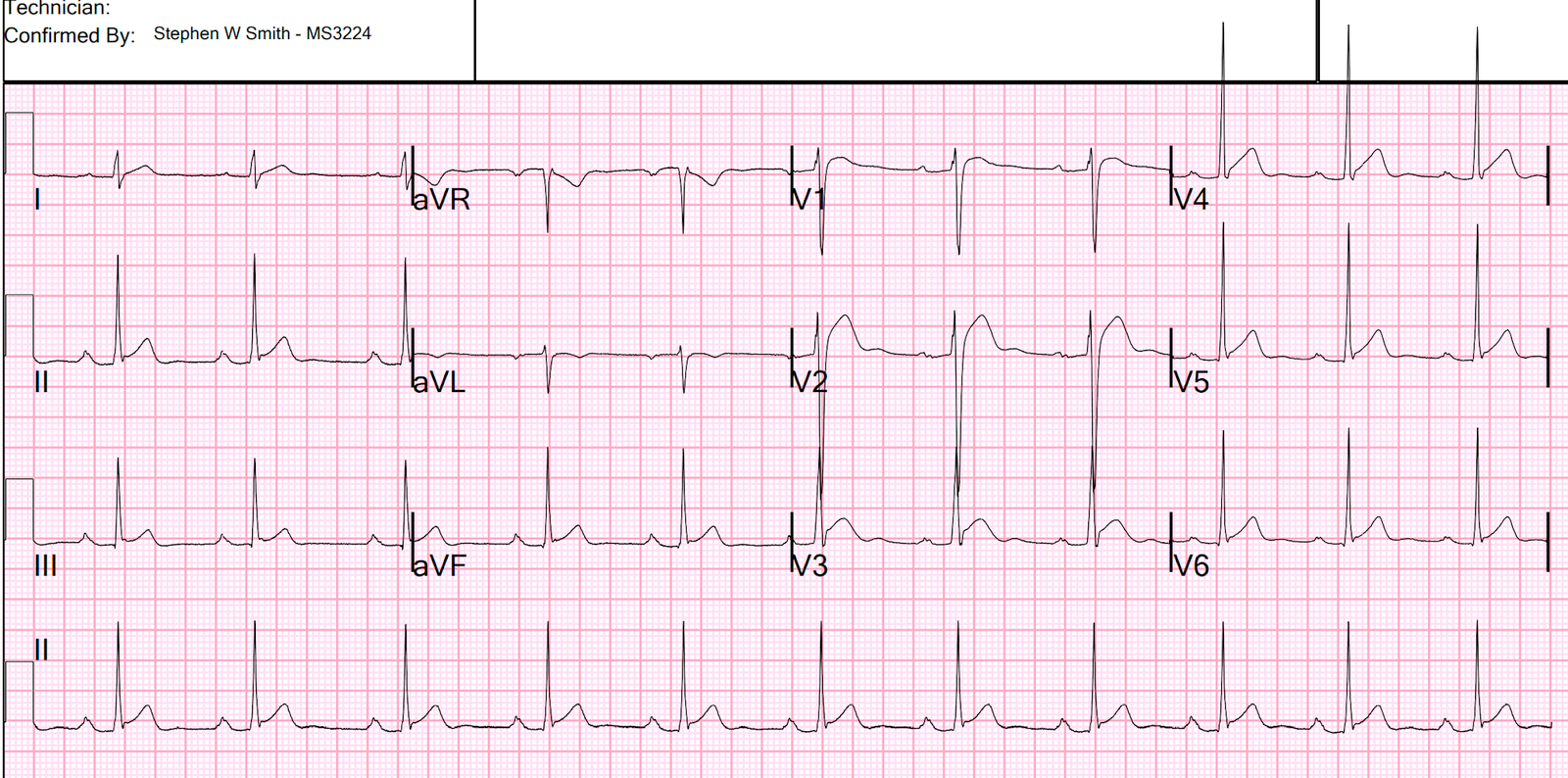
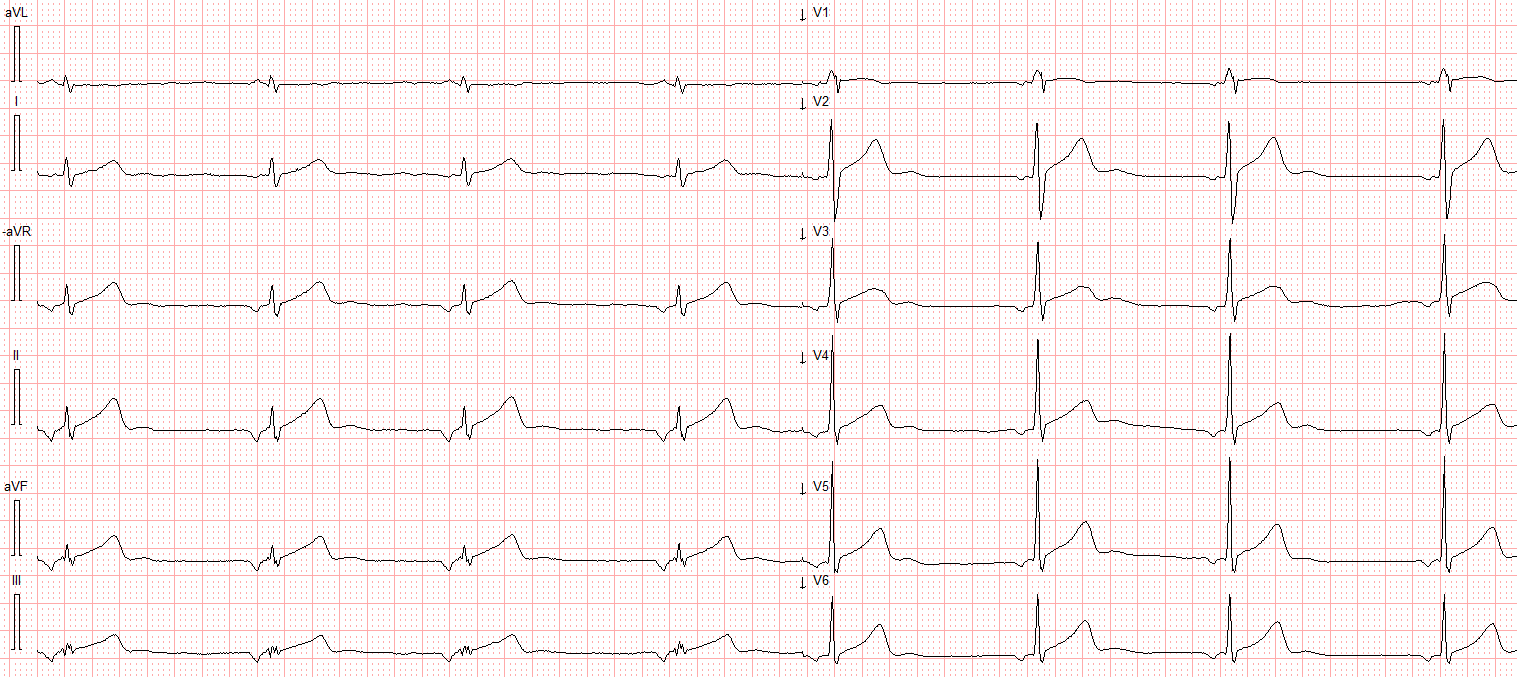
Post-angiogram ECG showed proximal LAD reperfusion:
Take home
1.
OMI ECG findings can diagnose true positive STEMI
earlier
2.
OMI ECG findings can diagnose false negative STEMI
3.
‘transient STEMI’ can have ongoing OMI
References
1. Meyers et al. Accuracy of OMI findings versus
STEMI criteria for diagnosis of acute coronary occlusion myocardial infarction.
Int J Cardiol Heart Vasc 2021
2. Aslanger et al. DIagnostic accuracy oF
electrocardiogram for acute coronary OCClusion resulTing in myocardial
infarction (DIFOCCULT study). Int J Cardiol Heart Vasc 2020
3. Lemkes et al. Timing of revascularization in patients with transient ST segment elevation myocardial infarction: a randomized clinical trial. Eur Heart J 2018
4. Bergmark et al. Transient ST-segment myocardial
infarction: a new category of high risk acute coronary syndrome? Eur Heart J
2019
==================================
Comment by KEN GRAUER, MD (2/13/2023):
==================================
I love cases like this one! They convincingly demonstrate the futility of staying “stuck” in the outdated STEMI paradigm that delays treatment of a significant percentage of acute MI patients.
- Today’s patient is a 70-year old adult who called EMS because of new-onset chest pain, associated with nausea and shortness of breath. This clinical presentation alone immediately places this patient in a “high-prevalence” group for having an acute event even before you look at the ECG! As a result — even subtle ECG findings are likely to be acute until proven otherwise.
Dr. McLaren’s excellent sequential presentation of today’s case takes us through the course of this actively evolving STEMI. As commonly occurs — the “culprit” vessel may spontaneously reopen — only to reocclude — sometimes repeating this occlusion-reopening process a number of times until the final state of the “culprit” vessel is reached.
- As per Dr. McLaren — today’s patient was clearly in need of prompt cath as soon as the initial ECG was recorded.
- That said — the initial ECG alone may not have sufficed to make prompt cath happen, if it were not for the occurrence of 2 additional factors: i) A 2nd ECG recorded 30 minutes later, showed frank STEMI criteria; and, ii) The patient had VFib arrest on arrival to the ED.
- In the hope of reinforcing Dr. McLaren’s case for immediate cath in today’s patient — I thought it worthwhile to take another look at the subtle-but-definitely-present ECG findings that were clearly evident in the initial tracing (Figure-1).
 |
| Figure-1: The initial ECG in today’s case — recorded by the paramedics on arrival at the scene. (To improve visualization — I’ve digitized the original ECG using PMcardio). |
Another Look at the Initial ECG:
To Emphasize — The patient in today’s case is a 70-year old adult who presented with severe new-onset chest pain. As a result — even subtle ECG findings need to be considered acute until proven otherwise.
- Given this clinical presentation — I like to start by asking myself IF there are any 1 or 2 leads that are definitely abnormal in a patient with severe new chest pain. In view of this clinical scenario — there is no way the coved and slightly elevated ST segment in lead aVL can be considered normal. (QUERY: Given the modest size of the QRS in lead aVL — Isn’t the ST segment in lead aVL disproportionately elevated as well as abnormally shaped?).
- Whether the QS in lead aVL is (or is not) an infarction Q wave — is hard to determine from this single tracing.
- Support that the coved and elevated ST segment in lead aVL is real — is forthcoming from the scooped ST depression in each of the inferior leads (with this “scooped” shape being a mirror-image opposite ST-T wave change to the appearance of the coved ST segment in lead aVL).
ST-T wave changes in the Chest Leads are more subtle — but given the context of new severe chest pain + ST elevation in aVL with reciprocal ST changes in the inferior leads — even subtle ECG abnormalities in the chest leads need to be considered real.
- In the context of the above limb lead abnormalities — I thought the T waves in leads V3 and V4 appeared hyperacute — in that these T waves are fatter-at-their-peak and wider-at-their-base than expected (ie, hypervoluminous).
- In this context — neighboring leads V2 and V5 are also suspicious (straightening of the ST segment takeoff in lead V2 — and a fatter T wave peak than expected in lead V5).
- Finally — the T wave in lead V6 is clearly much flatter than it should be (When the QRS is upright in lead V6 — the T wave in this lead should be upright and larger than seen here).
In Conclusion: Millimeter-based STEMI criteria are not met in ECG #1. That said, in this patient with severe new chest pain — the overall ECG picture with ST-T wave abnormalities in 9/12 leads has to be considered (as stated by Dr. McLaren) — as “All concerning for acute LAD occlusion”.