These 2 ECGs were texted to me with the words “I think acute MI, but cardiology does not.”
I believed these to be 2 serial ECGs:
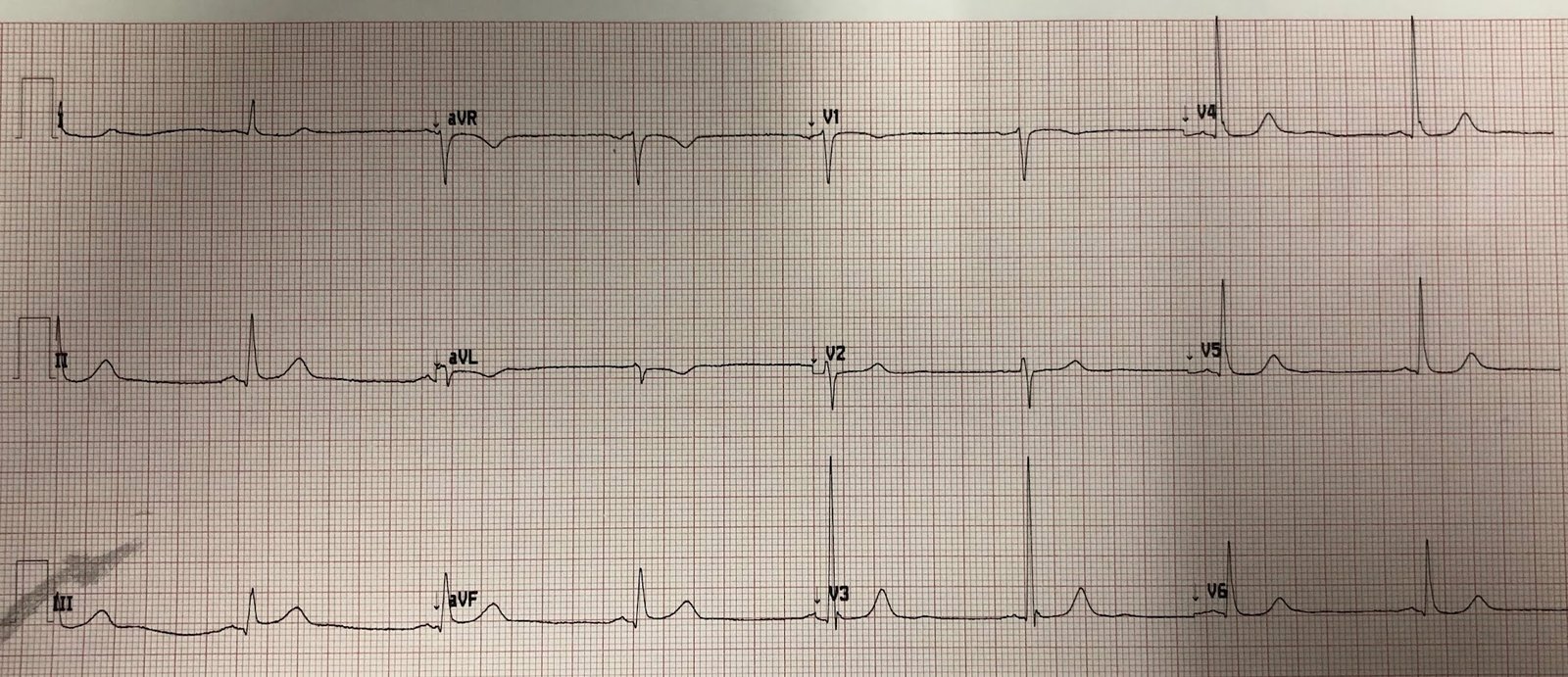
ECG 1: (later found to be time zero):
And the other: (later found to be time 24 minutes):
This was my response:
“It looks like a myocardial infarction…Does the patient have chest pain?”
History:
Syncope in clinic, some vague chest pain.
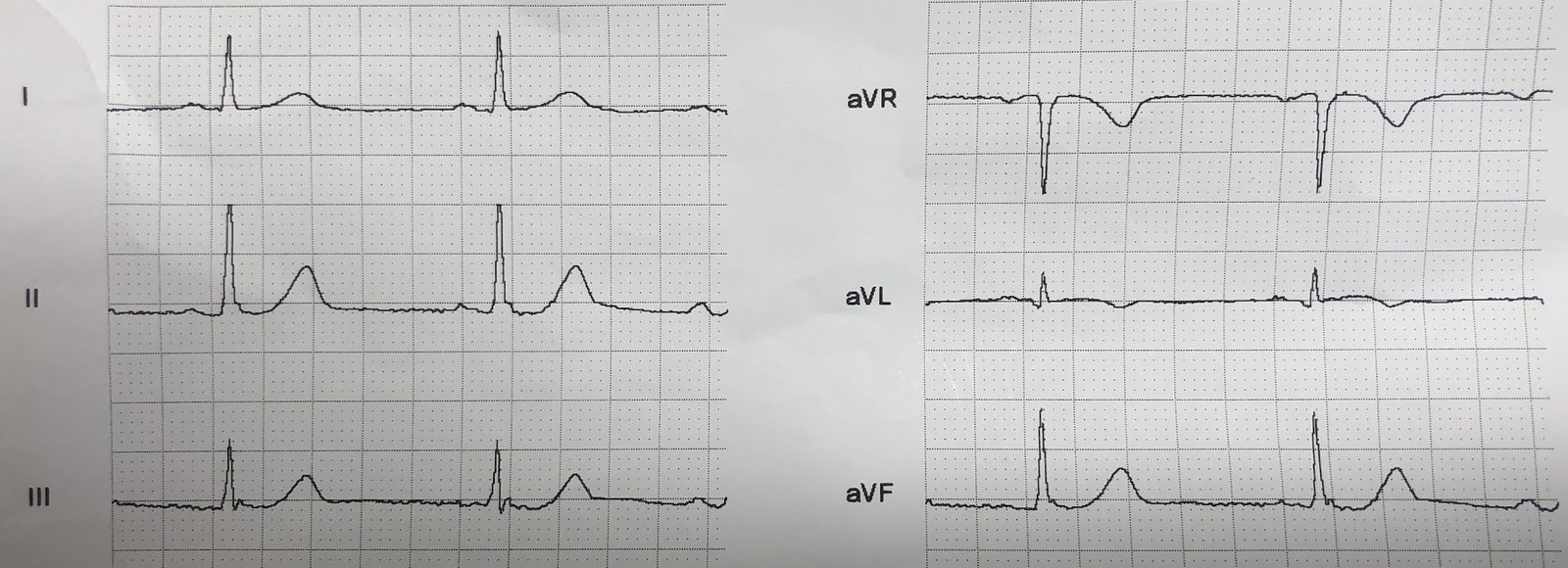
Not a great history, so we looked for a previous ECG:
 |
| From within the last year
No STE, no STD. |
Cardiology had wanted the patient to be admitted, but had not seen evidence of acute MI and had not wanted the cath lab activated.
In spite of this, my partner and I agreed the cath lab should be activated, so he did activate.
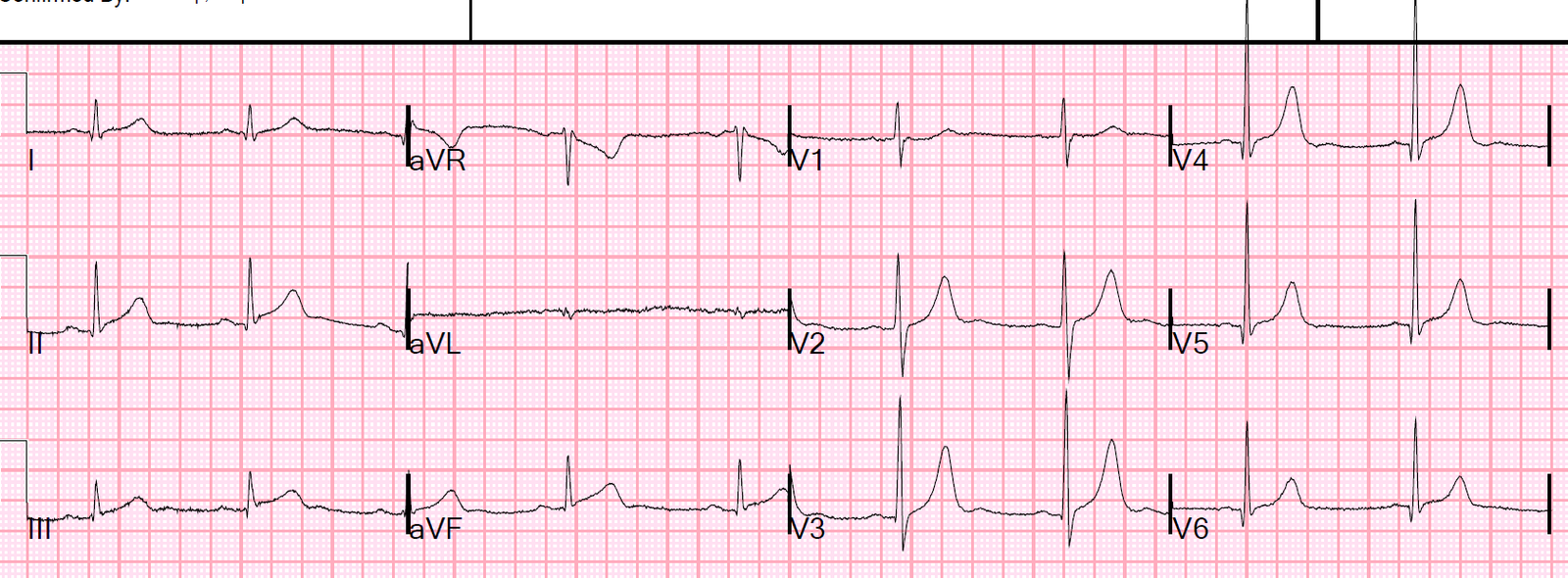
Just before transport, another ECG was recorded at time 71 min, prior to cath:
 |
| Now obvious inferior and posterior STEMI. |
The patient had a ventricular fibrillation arrest before the angiogram, and was resuscitated.
Angiogram: 100% distal RCA occlusion.
After cath, next day:
 |
| Reperfusion T-wave in III. STE resolved. |
Peak trop 47.4 ng/mL (large MI)
Echo: Regional wall motion abnormality-inferior, EF 60%.
Learning Points:
1. In the original thrombolytic trials (the only placebo-controlled reperfusion trials!), especially GISSI-1, treatment of inferior MI with streptokinase did not have a measurable effect on mortality outcome. Here we see what appears to be an electrocardiographically tiny inferior MI, which only later becomes large. The patient arrests and has a very high troponin. So don’t be fooled by an apparently small inferior MI.
2. Do serial ECGs.
3. Compare with a previous ECG.
4. You must push to get patients who need it to the cath lab.
5. Cardiologists have a huge amount they have to know, spanning an enormous specialty. They do not always have time to learn the subtleties of OMI on the ECG.
6. You have to be the expert!!
===================================
Comment by KEN GRAUER, MD (6/23/2019):
===================================
The definition of the word “subtle” is — so delicate or precise as to be difficult to analyze or describe (especially when referring to a change). Subtlety is the “theme” of this case.
- For clarity — I’ve put the first 3 ECGs shown in this case together in Figure-1. Because of how subtle the findings are — I’ve enlarged one complex in leads II, III, aVF and aVL, that I’ve placed to the right of each of these tracings.