Written by Jesse McLaren
A previously healthy 60 year old
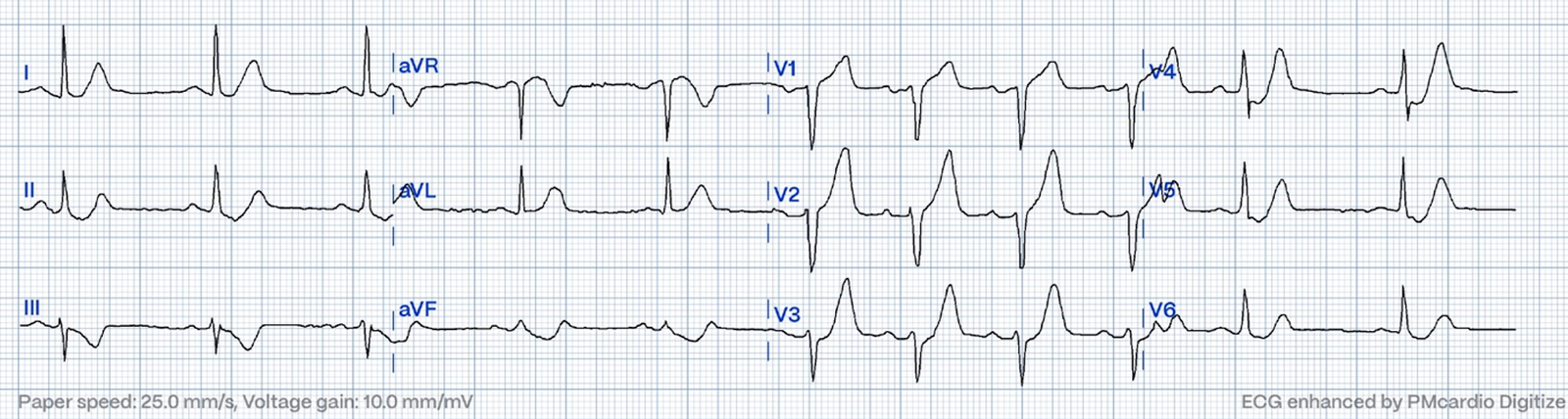
developed exertional chest pain with diaphoresis, and called EMS. Here’s the
EMS ECG, digitized with PM cardio. What do you think?
There’s sinus
arrhythmia with normal conduction, normal axis and normal voltages. There’s
loss of R waves in V2-3 with hyperacute waves V1-5. There’s no significant ST
elevation but there are two forms of ST depression: deWinter T wave V3-5 and
precordial swirl with ST depression V6 reciprocal to subtle STE in V1. In the limb leads
there’s no ST elevation, but there are hyperacute T waves in I/aVL with
reciprocal inferior ST depression. So while there’s no diagnostic STEMI criteria, there
are multiple ischemic abnormalities in 11/12 leads involving QRS, ST and T waves, which are
diagnostic of a proximal LAD occlusion.
Queen of Hearts PMCardio AI system was highly confident in OMI based on the hyperacute T waves and ST depression, despite absence of STEMI criteria:
Precordial Swirl — 20 cases of Swirl or Look-Alikes
Click here to sign up for Queen of Hearts Access
The paramedics called
a code STEMI from the field, and gave the patient aspirin and three sprays of
nitro. They arrived in the ED 30 minutes later to meet the cardiology team,
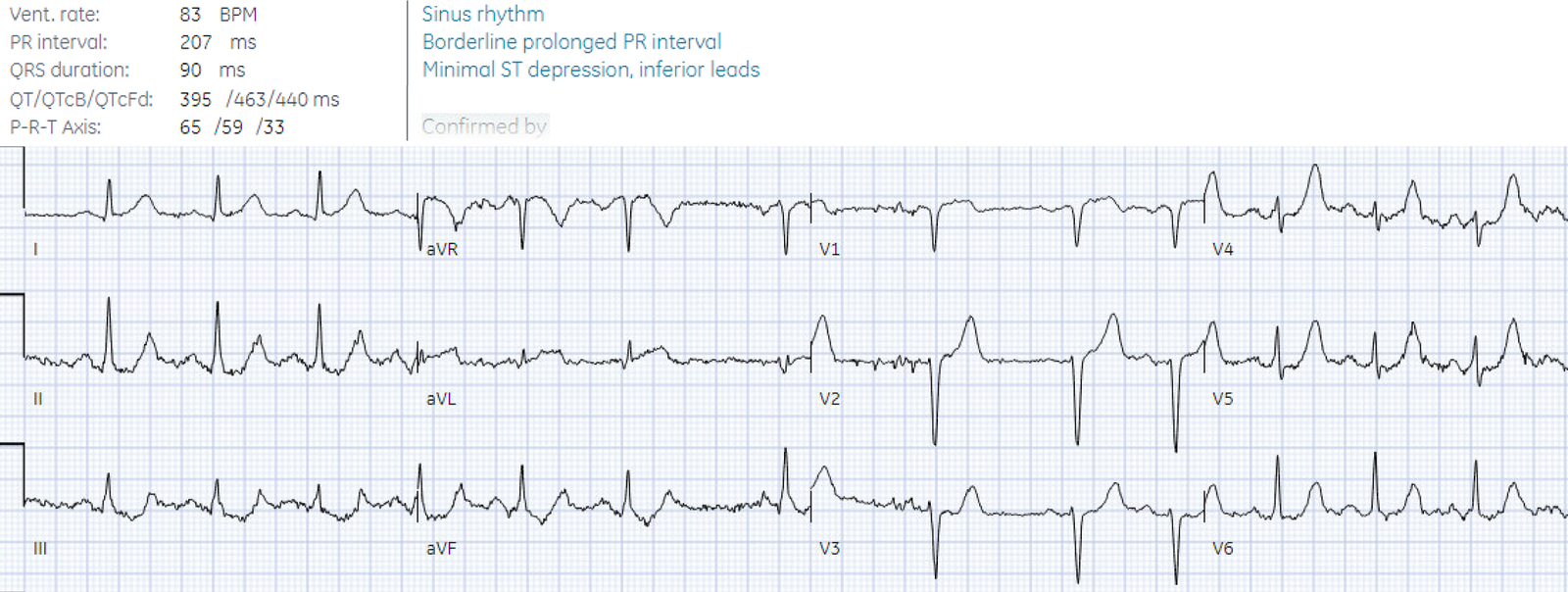
where an ECG was repeated:
Again no STEMI
criteria, and there has been improvement in the deWinter and swirl pattern. But
there are ongoing precordial hyperacute T waves and ongoing inferior ST
depression, and this is reciprocal to subtle straight ST elevation in aVL. The
final blinded cardiology interpretation noted only the minimal inferior ST
depression, but the ECG is still diagnostic of proximal LAD occlusion.
Fortunately, the
treating cardiology team noted the hyperacute T waves and subtle STE in aVL and
continued with the plan for emergent angiography: 100% proximal LAD occlusion. First
trop was 7,000ng/L (normal <26 in males in <16 in females) which goes
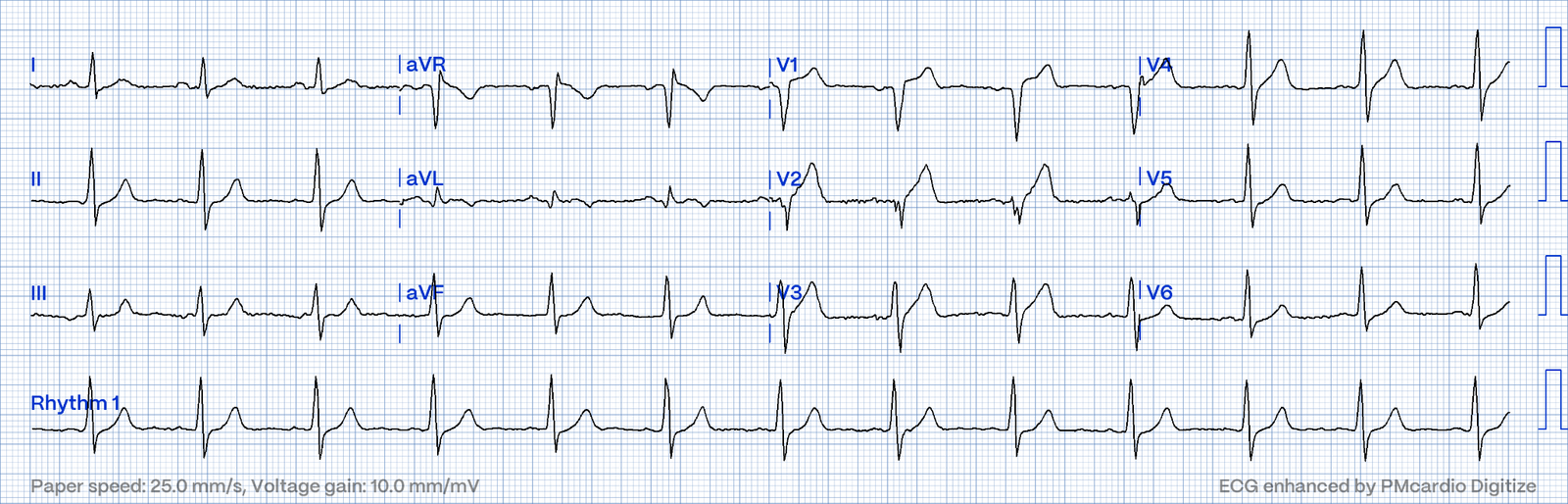
along with the loss of R waves, and peak was 94,000 ng/L. Echo showed EF reduced to 35% with anteroseptal hypokinesis and akinetic apex. Discharge ECG showed
antero-lateral reperfusion T wave inversion:
The discharge
diagnosis was ‘STEMI’ but no ECG met STEMI criteria, and blinded cardiology
interpretation of the ED ECG was also STEMI negative.
In the current paradigm
it would make more sense to call this Non-STEMI because the patient had a type
1 MI without any ECG meeting STEMI criteria. But that wouldn’t account for why
the cath lab was activated emergently, because this is supposed to be reserved for
patients with STEMI. So the discharge
diagnosis ‘STEMI’ was more a reflection of the time to treatment (emergent cath) rather
than current diagnostic dichotomy (STEMI vs Non-STEMI). It is an example of a frequent occurrence: clinicians call OMI “STEMI.” So this is a STEMI(-)OMI which was treated like a STEMI, with rapid reperfusion
despite the current paradigm.
Discharge
diagnosis: STEMI/NSTEMI vs OMI/NOMI
Why this
matters is that > 25% of ‘Non-STEMI’ patients with delayed
angiography have the exact same pathology of acute coronary occlusion. Their discharge
diagnosis also better reflects time to treatment (non-urgent
cath), rather than diagnosis.
These discharge diagnoses create a bias in STEMI/Non-STEMI databases: not
only are STEMI(-)OMI with delayed reperfusion buried in Non-STEMI databases
along with non-occlusive MIs, which prevents us learning from missed
occlusions; but also, STEMI(-)OMI that are rapidly reperfused are buried in
STEMI databases, which prevents us from learning from great cases like this.
Both
reinforce the false STEMI/non-STEMI dichotomy, and are barriers to shifting
towards the OMI paradigm.
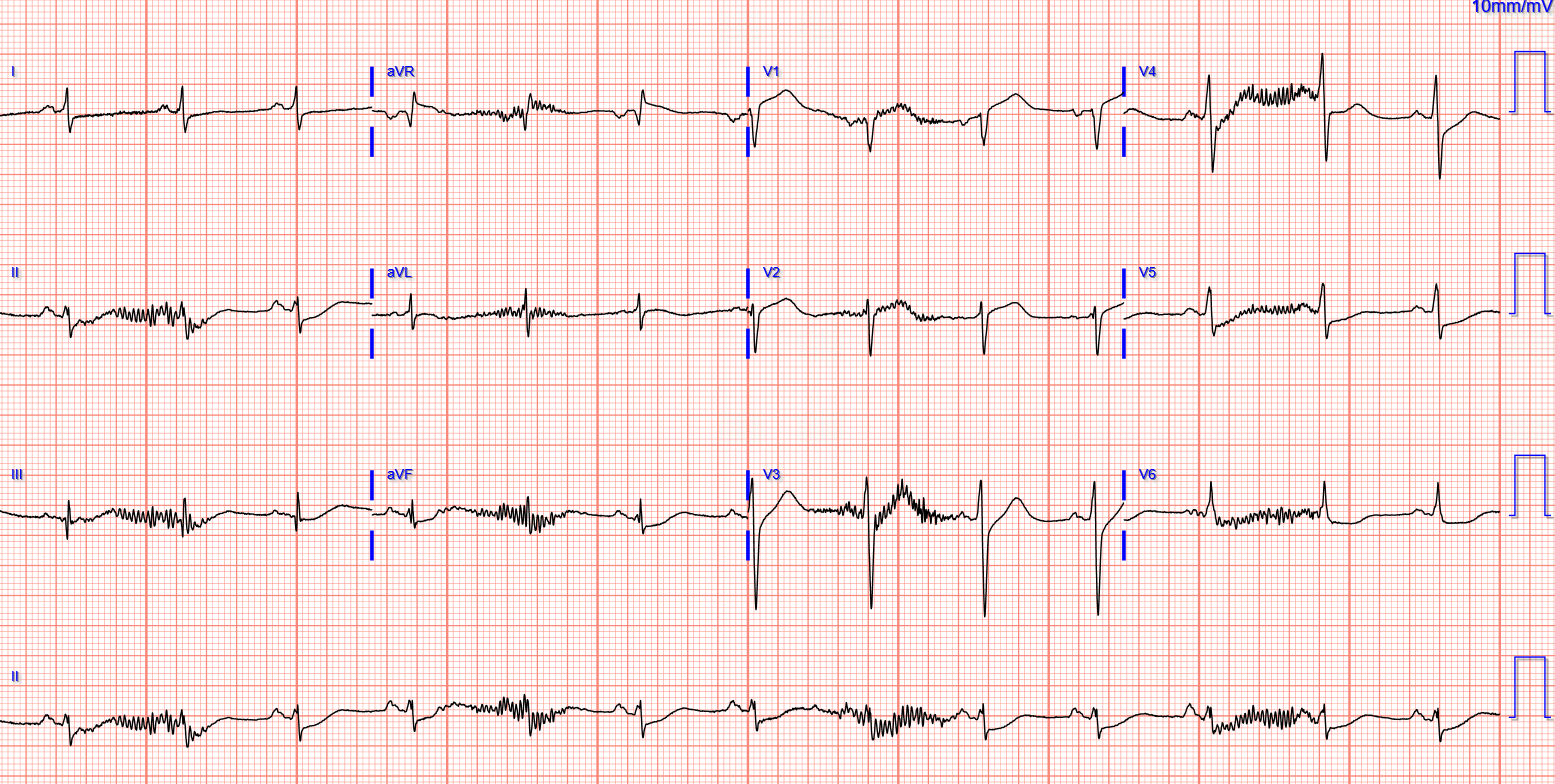
For comparison, see this similar case of a 60 year old with chest pain, with cath lab activated from the field:
Also diagnostic of LAD occlusion, with anterior hyperacute T waves, precordial swirl, and subtle inferior ST depression. The patient also had a 100% proximal LAD occlusion, with a peak troponin of 100,000 ng/L. But because Code STEMI was cancelled on arrival and the patient had delayed angiography, the discharge diagnosis was ‘non-STEMI’ despite having the exact same pathology.
Rather than calling the first ‘STEMI’ because of rapid reperfusion and the second ‘non-STEMI’ because of delayed reperfusion, both should be called what they are: OMI – and then we can learn from both.
The new ACC
expert consensus explains that: “STEMI ECG criteria on a standard 12-lead ECG
alone will miss a significant minority of patients who have acute coronary
occlusion. Therefore, the ECG should be closely examined for subtle changes
that may represent initial ECG signs of vessel occlusion, such as hyperacute T
waves or ST-segment elevation <1 mm, particularly when combined with
reciprocal ST-segment depression.” But if STEMI criteria is a poor surrogate marker,
and if what we care about is acute coronary occlusion, then discharge diagnoses
should change to reflect a new classification of OMI/NOMI rather than
STEMI/Non-STEMI.
Take home
1.STEMI criteria has poor sensitivity
for acute coronary occlusion
2.Other signs of occlusion
include hyperacute T waves, deWinter pattern, precordial swirl, and ST depression reciprocal to subtle ST elevation/hyperacute T
3. Discharge diagnoses and MI
classification should reflect patient outcomes of Occlusion vs non-Occlusion MI,
not arbitrary STE vs Non-STE criteria, or rapid vs delayed time to cath. All OMIs can then be reviewed to
identify which were missed and which were rapidly reperfused, in order to learn
from both
===================================
MY Comment, by KEN GRAUER, MD (7/7/2024):
===================================
Today’s post by Dr. McLaren is an important one — in that emphasizes by means of 2 clinical example cases, shortcomings of the outdated and problematic STEMI paradigm.
- Regular followers of Dr. Smith’s ECG Blog will be well familiar with scores of cases we’ve presented illustrating the trials and tribulations of the millimeter-based STEMI paradigm. All-too-many clinicians (including cardiologists) — remain “stuck” on this STEMI paradigm out of force of habit and failure to appreciate the now well-defined pathophysiology of what happens during the course of an evolving ACO (Acute Coronary Occlusion) — which is what we call an OMI (Occlusion Myocardial Infarction).
- As per the 2 cases presented today by Dr. McLaren — the consequences of this current fallacious approach are many and far-reaching.
An expanding literature has now convincingly shown the following:
- Rigid adherence to millimeter-based STEMI criteria misses at least 1/3 of OMIs (Meyers, Smith et al — Ann Emerg Med 74(4): S26, 2019 — and — Meyers, Smith et al — Int J Cardiol Heart Vasc, 2021).
- We know STEMI criteria are problematic — because clinicians trained to assess other ECG parameters (instead of relying solely on a given amount of millimeters of ST elevation) — are able to accurately identify OMIs that adherence to STEMI criteria will miss (McLaren, Meyers, Smith — Canad J Emerg Med 24: 250-255, 2022) — and — Westafer L — ACEP Now, Dec., 2022 — and — Kontos et al; 2022 ACC Expert Consensus — JACC 80(20):1925-1960, 2022).
- More than simple failure to identfy STEMI-/OMI+ cases — adherence to the outdated STEMI paradigm may result in delayed diagnosis of many patients with acute coronary occlusion who did not manifest enough ST elevation to “qualify” for a STEMI at the time they were seen.
- The clinical reality of this delayed diagnosis distorts data in the literature by overestimating the accuracy of the STEMI paradigm. This happens because some patients who are STEMI- initially — eventually do develop enough ST elevation to “qualify” as a STEMI — yet delay by a period of hours (and sometimes delay for up to a day or more!) — means significant loss of viable myocardium in these OMI+ patients, who should have been recognized and treated with PCI long before they finally developed “enough” ST elevation to qualify as a STEMI (McLaren, Meyers, Smith — J Electrocardiol 76: 39-44, 2023).
- Another way in which the current literature is distorted in favor of the failed STEMI paradigm — is that there are no false negatives among STEMI- patients (McLaren, Meyers, Smith — J Electrocardiol 76: 39-44, 2023). This is because failure to satisfy millimeter-based STEMI criteria is erroneously accepted as the absence of acute coronary occlusion — and then misclassified as a “NSTEMI”. Unfortunately, this methodological flaw perpetuates false conclusions about the overrated accuracy of STEMI criteria.
Clinicians and the STEMI Paradigm both ignore OMI Pathophysiology:
Based on cases submitted to us at Dr. Smith’s ECG Blog — the overwhelming majority of clinicians (including cardiologists) ignore the basic pathophysiology of what happens during the course of an acutely evolving OMI. Consider the following:
- Not uncommonly — the “culprit” artery may suddenly occlude — then spontaneously reopen (sometimes prior to the patient seeking medical attention) — and on occasion, continue to open and close spontaneously a number of times. Interpreting serial ECGs that are correlated to the patient’s History — can tell us the state of the “culprit” vessel (thereby helping us greatly to understand and interpret ECGs that may not be showing frank ST elevation).
- With acute occlusion — the patient typically develops CP (Chest Pain) — and — ST segments over the area of infarction tend to elevate, while in opposite areas of the heart, there is typically reciprocal ST depression.
- With spontaneous reopening of the “culprit” vessel — CP decreases (or resolves) — and — ST segment deviations (elevation and depression) improve or normalize.
- KEY Point: What spontaneously opens — may just as easily (and at any time) spontaneously reclose. It is for this reason that even if a patient who had ST elevation is now pain-free and now without ST elevation — that prompt cath with PCI is still indicated, because that patient may still at any time spontaneously reocclude.
- CAVEAT: Even a recent STEMI may fail to show ST elevation at the time the ECG you are looking at was done IF — prior to this, there has been an ongoing process of intermittent occlusion, followed by spontaneous reopening. Remember that in between the phase of acute ST elevation and development of reperfusion T waves (with T wave inversion) — may come a phase of pseudo-normalization, in which the ECG may look surprisingly unremarkable.
- Many of these patients with positive troponin and unremarkable or nonspecific changes on ECG at the time their tracing was recorded — are misdiagnosed as having had a “NSTEMI” — when in fact they had acute coronary occlusion. Failure to correlate symptoms with each ECG (stemming from a failure to appreciate the pathophysiology described above, of an acutely evolving OMI) is the reason for gross overuse of the term, “NSTEMI”.
- Finally, depending on WHEN the cath was done during the course of a “transient” STEMI — the “culprit” artery may not always still be occluded at the time of cardiac catheterization (ie, a less than totally occluded artery on cath might still be the “culprit” artery that caused the infarction).