An 80-something year old man with history of metastatic cancer had acute onset of chest pain and called 911.
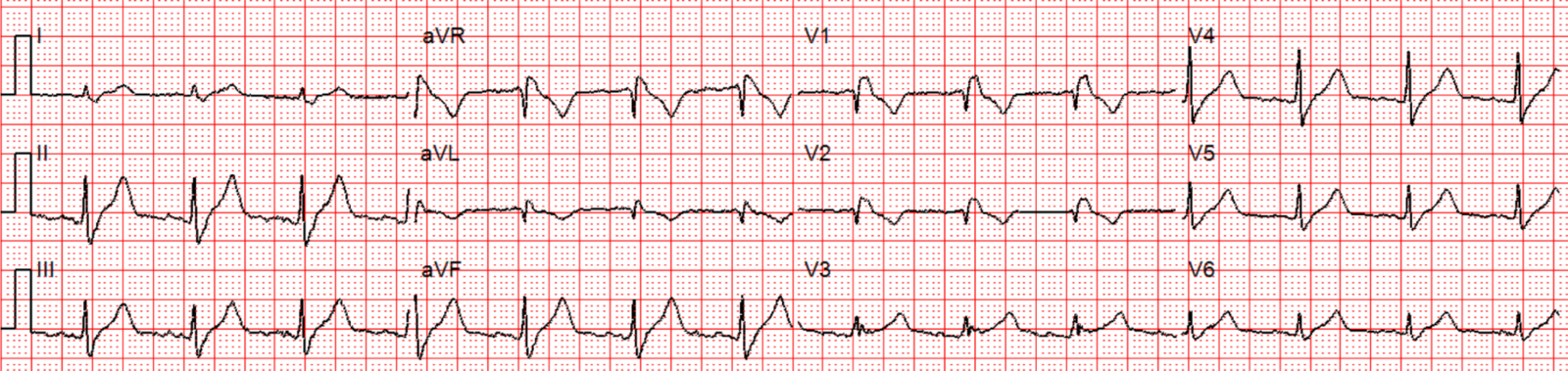
Here is his prehospital ECG:
What do you think?
The computer read ***Anterior STEMI*** along with RBBB.
Smith interpretation: There is Right Bundle Branch Block (RBBB). There is 1 mm of STE in inferior leads and also in lateral precordial leads. As a general rule, RBBB should not have ST Elevation (there are some infrequent patients with RBBB who have non-ischemic STE, usually discordant to the negative S-wave, as in this case). Moreover, the T-waves appear hyperacute.
I would activate the cath lab based on this and the clinical presentation, but I do NOT see any evidence of anterior ***STEMI***
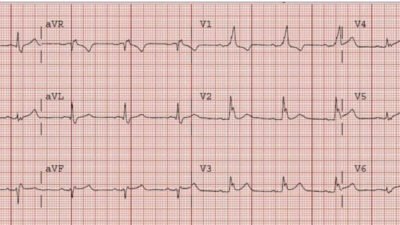
The patient arrived in the ED and had this ECG:
The T-waves are now less hyperacute, but ST Elevation remains.
A bedside echo was done:
This shows a small effusion.
The patient went to the cath lab and had no acute lesion.
He ruled out for acute MI by negative serial troponins.
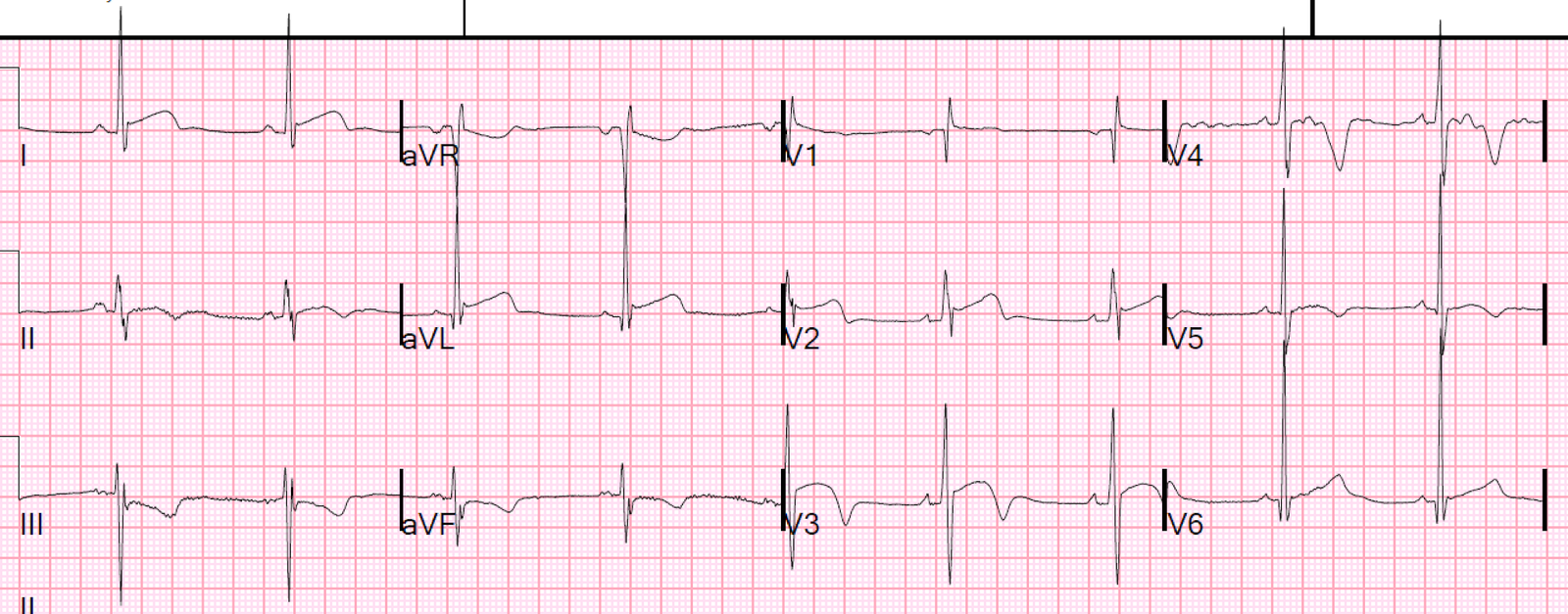
Here is his ECG the next AM:
Some ST Elevation remains. There is no typical evolution of MI (so BOTH EKG evolution, and troponin, proves there was no acute MI)
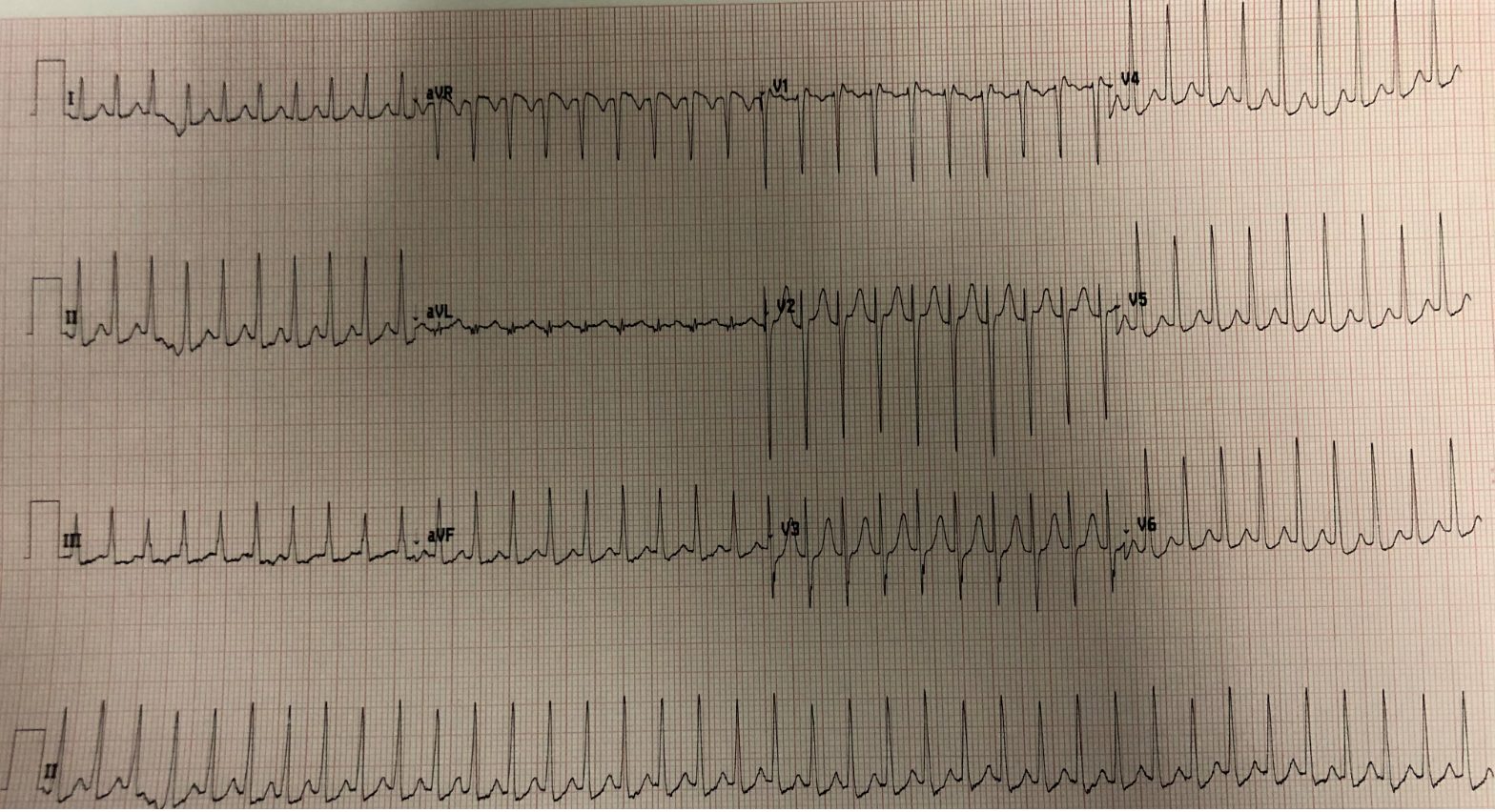
2 weeks later, the patient present with acute chest pain again. Here is his ECG:
No STE at all, and no hyperacute T-waves.
He ruled out for MI by troponins again.
Here was his echo that evening:
Continued
9 hours later: the patient presented with fever and hypotension.
Here was his cardiac echo (remember, done 9 hours after the one above):
Pericardial Effusion with Tamponade physiology, developed within 9 hours.
Here is the ECG:
No ST Elevation
Final Diagnosis: Pericarditis
The fluid was nondiagnostic as to etiology of pericarditis.