This was a male in his 20s who was found down, intoxicated presumably with an opiate, perhaps methadone. He awoke very slowly with naloxone, probably because his brain had been hypoxic for a while.
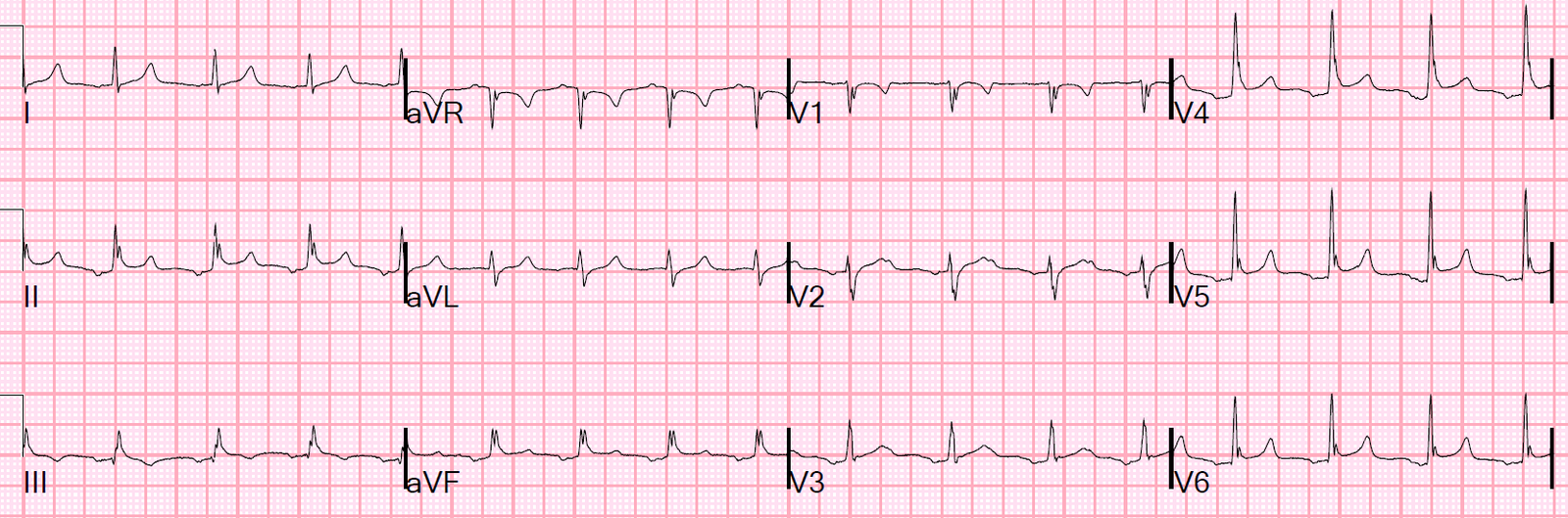
He had an ECG recorded.
 |
| Sinus tachycardia.
Computer reads QRS as 114 ms. What else? |
Notice that at the end of the QRS in leads II and V4-V6 there is a distortion: these “J-waves” are very large. They are, in fact, Osborn waves. They result in the QRS measurement being wide (114 ms).
The K at this point was 4.6 mEq/L.
His rectal temp was taken and it was 33.2 C.
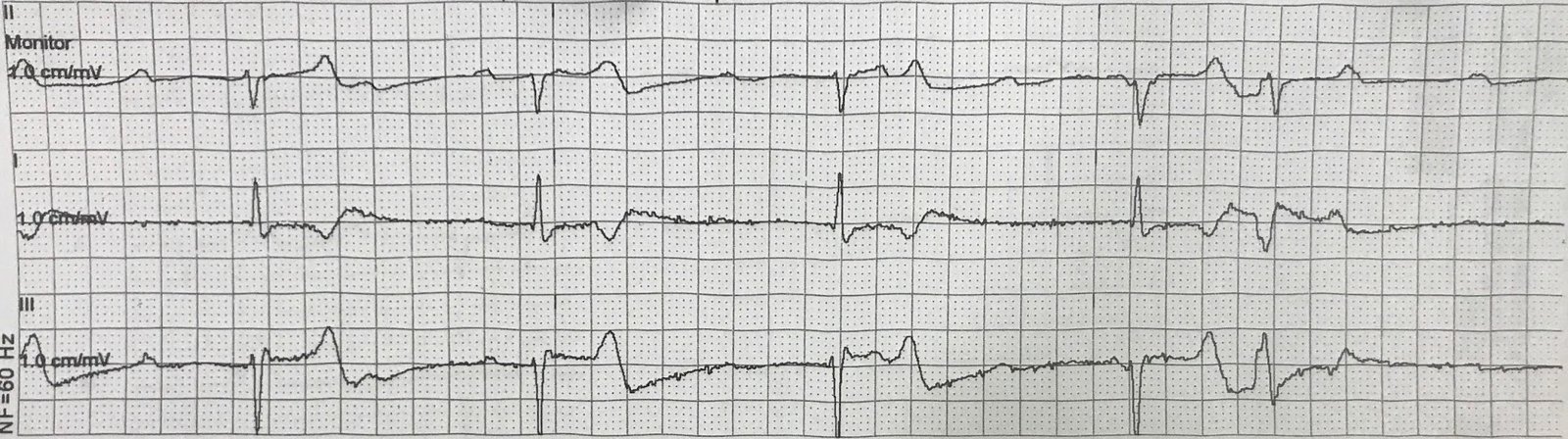
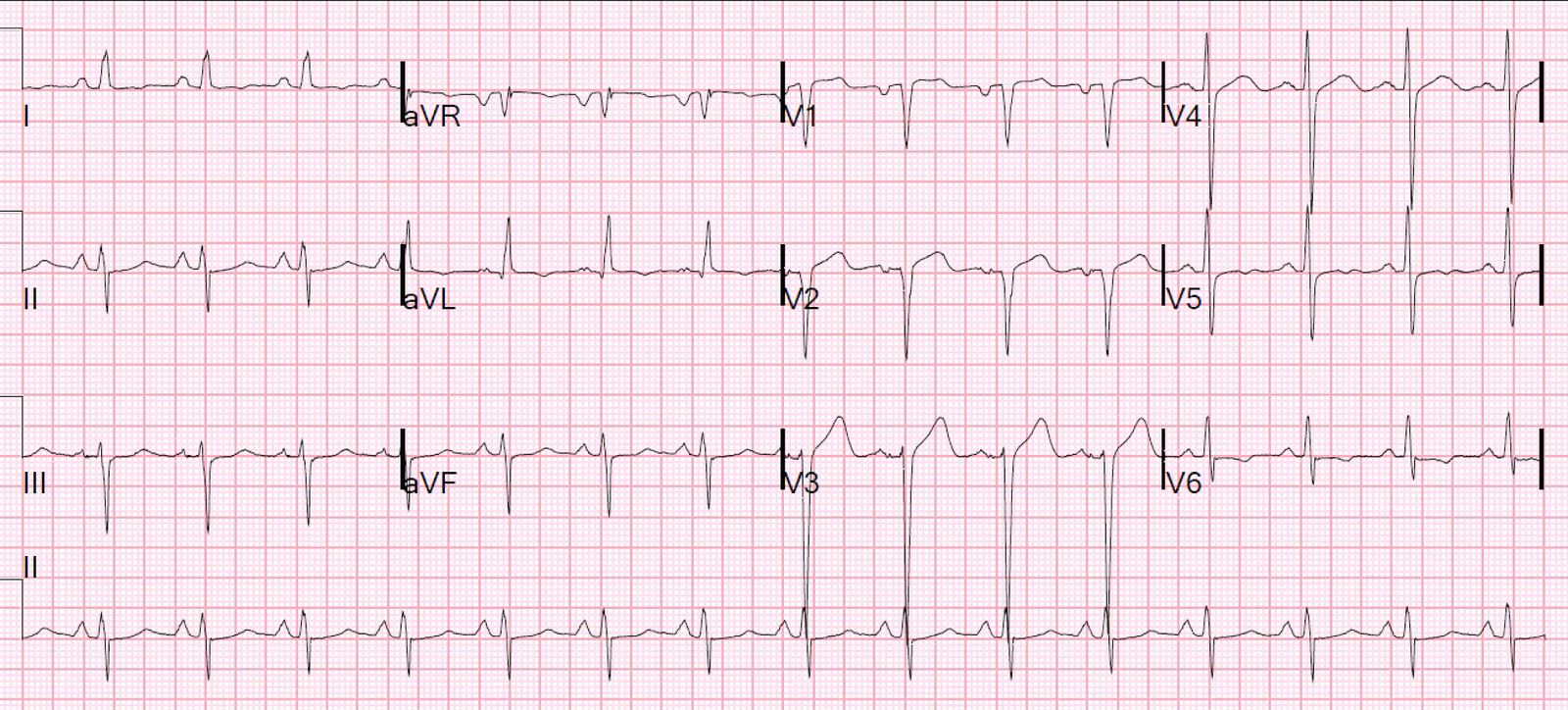
He was externally warmed. He became hypotensive and was resuscitated, and another ECG was recorded at a temp of 34.5 degrees C:
Only one thing: There is a negative P-wave axis now. So there is now either a low atrial rhythm or a high junctional rhythm (both will have negative P-waves that are see before the QRS — a low junctional rhythm with result in P-wave in, or after, the QRS.
All I see is the change in P-wave axis, and that is what is interesting: in the time between ECGs, the K had risen to 7.6 mEq/L. The patient had rhabodmyolysis and was rapidly releasing potassium into the circulation.
Other than the change in P-wave axis, I could not find any evidence of hyperkalemia on this ECG, compared to the previous. And I cannot prove that the change in P-wave axis is due to hyperkalemia.
We treated with calcium and shifting: intramuscular terbutaline, insulin, glucose, furosemide, and precious bicarbonate because there was rhabdomyolysis. We placed a dialysis catheter in anticipation of continued release of potassium and possible severe kidney injury.
Rhabdomyolysis patients can have a huge continued ongoing release of potassium that sometimes even dialysis cannot keep up with.
The patient did well in spite of a CK rise to above 100,000.
Learning Points:
1. Recognize Osborn waves.
2.
Significant hyperkalemia can (rarely) be nearly invisible on the ECG,
even with a previous ECG for comparison. In this case, the only
possible clue was a change in P-wave axis, and I cannot even
3. Beta-2 Agonists are useful in lowering K, but only in high nebulized doses or parenteral administration.
Parenteral Beta Agonists for Hyperkalemia (Terbutaline, Albuterol)
Previous post with more references:
Terbutaline and Albuterol for Lowering of Plasma Postassium
–0.5 mg of IV albuterol reduces K by about 1.2 mEq/L.
–A 20 mg neb (most for bronchospasm are only 2.5 mg) lowers it by about 1.0 mEq/L.
–A 10 mg neb lowers it by about 0.6 mEq/L.
I give 0.25 mg of IM terbutaline to an adult, but only if it is critical, and add nebulized albuterol also.
I’ve never given it IV, as I’m a bit reluctant to risk the cardiac irritability.
Here are a couple abstracts on beta agonists in hyperkalemia:
hyperkalemia is a frequent and potentially life-threatening medical
problem in patients on maintenance hemodialysis therapy. beta-Adrenergic
receptor (betaAR) stimulation causes potassium cellular influx and a
decline in plasma potassium concentrations. Therefore, betaAR agonists
are used in the treatment of patients with hyperkalemia. The goal of
this study is to evaluate the utility of weight-based subcutaneous
terbutaline dosing to reduce plasma potassium concentrations in a group
of subjects with chronic kidney disease (CKD) requiring hemodialysis.
subjects with CKD receiving long-term hemodialysis were administered
terbutaline, 7 microg/kg, subcutaneously. Heart rate measurements and
blood samples for potassium concentration determinations were made
serially for 420 minutes. Effects of terbutaline on heart rate and
potassium responses were determined in each subject.
Results: Terbutaline significantly reduced plasma potassium concentrations and significantly increased heart rates during the time course of the study. Mean reduction was -1.31 +- 0.5 mEq/L and increase in peak heart rate was 25.8 +/- 1, both highly significant. No adverse events were reported.
CONCLUSION: Administration
of subcutaneous terbutaline obviates the need for intravenous access
and should be considered as an alternative to nebulized or inhaled
beta-agonists to treat acute hyperkalemia in patients with CKD. As with
the use of any beta-adrenergic agonist, close cardiovascular monitoring
is necessary to avoid or minimize toxicity during therapy.
effects of intravenous infusion or nebulization of salbutamol in
patients with chronic renal failure: comparative study.
examine and compare the efficacy and safety of different routes of
administration of salbutamol in treating hyperkalemia, 15 patients with
chronic renal failure (blood urea nitrogen>80 mg/dL, serum
creatinine>8.0 mg/dL) were enrolled to sequentially receive either
intravenous infusion (0.5 mg) or nebulization (10 mg) of salbutamol.
Five of these patients (33.3%) did not respond to the intravenous
salbutamol and were excluded from the study. Both treatments
significantly decreased plasma potassium in 10 patients and the decrease
was sustained for at least 3 hours. After infusion, the maximal
reduction in plasma potassium levels was 0.92 +/- 0.10 mEq/L and
occurred after 30 minutes. On the other hand, the maximal reduction in
plasma potassium after nebulization (0.85 +/- 0.13 mEq/L) was similar to
that after infusion, but it occurred after 90 minutes. Insulin and
blood glucose increased, whereas blood pH, PCO2, sodium, osmolality, and
blood pressure did not change after either treatment. Heart rate
increased significantly after both treatments, but less after
nebulization than after infusion. It is concluded that both infusion and
nebulization are simple, effective, and safe therapeutic modalities for
the treatment of hyperkalemia in patients with chronic renal failure.
Infusion should be used in patients requiring a rapid decrease in plasma
potassium; nebulization, on the other hand, should be used in patients
with coronary artery diseases.