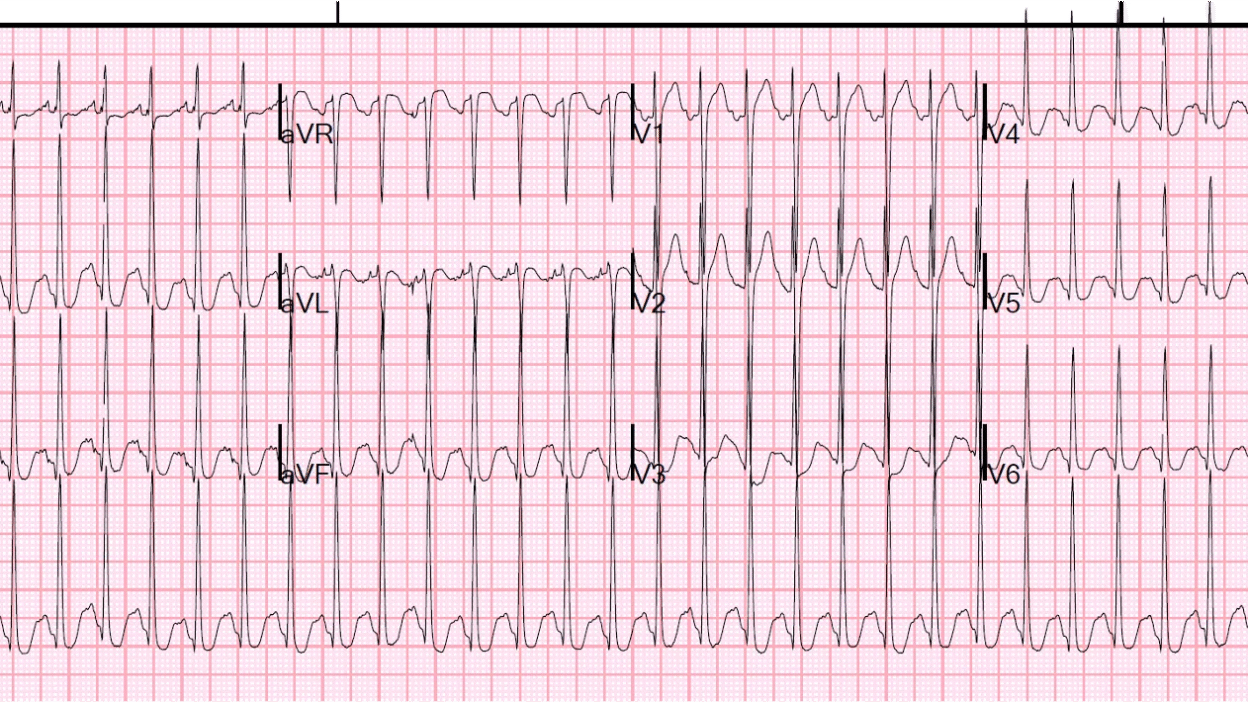
30-something male presented by EMS for evaluation of agitation and tachycardia. Per EMS, patient was running through the street, yelling, and punching cars. EMS measured his pulse from 190-200. They administered 10 mg of droperidol in order to calm the patient sufficiently to record a 12-lead ECG.
What do you think?
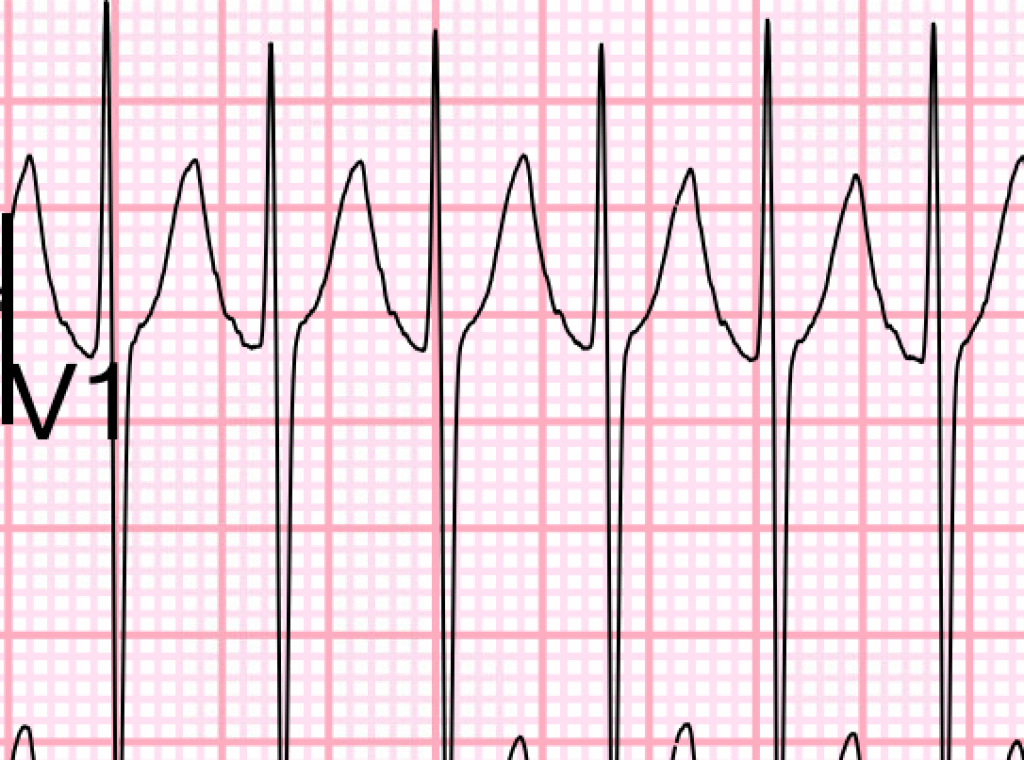
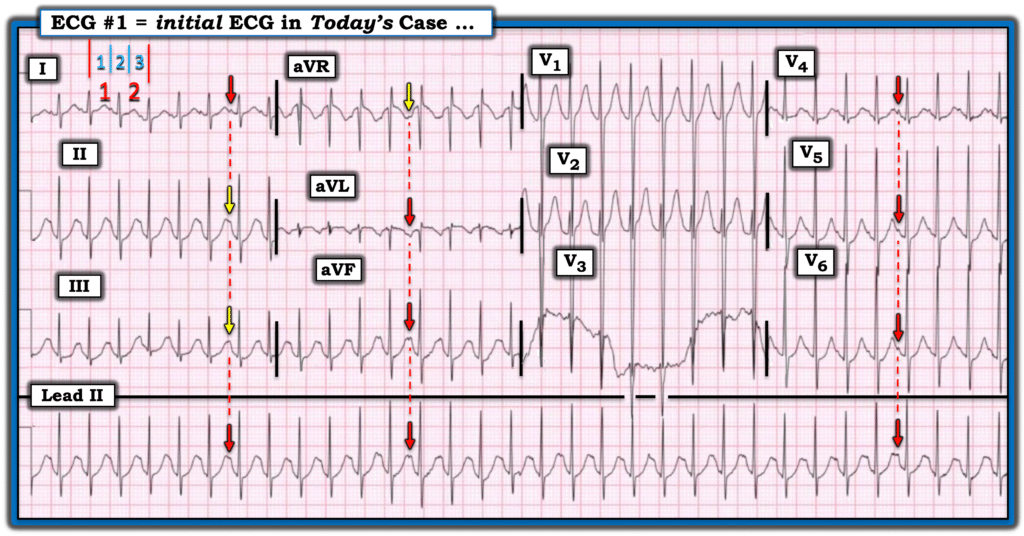
There is a very fast SVT at a rate of about 204 bpm. They administered adenosine 6 mg without terminating the rhythm. They then gave 12 mg adenosine without results. They gave another 12 mg adenosine without termination.
Why did it fail?
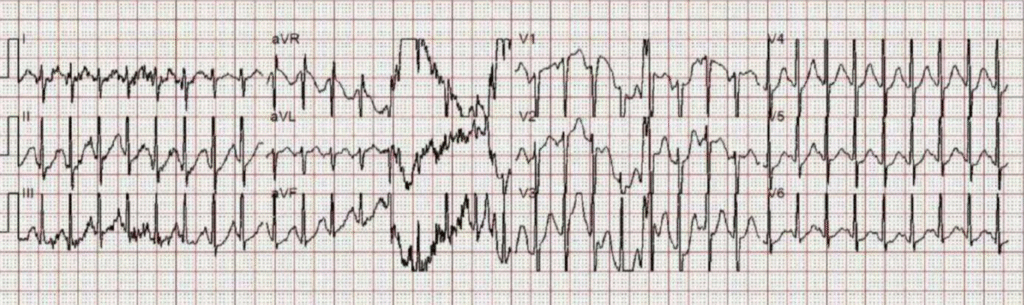
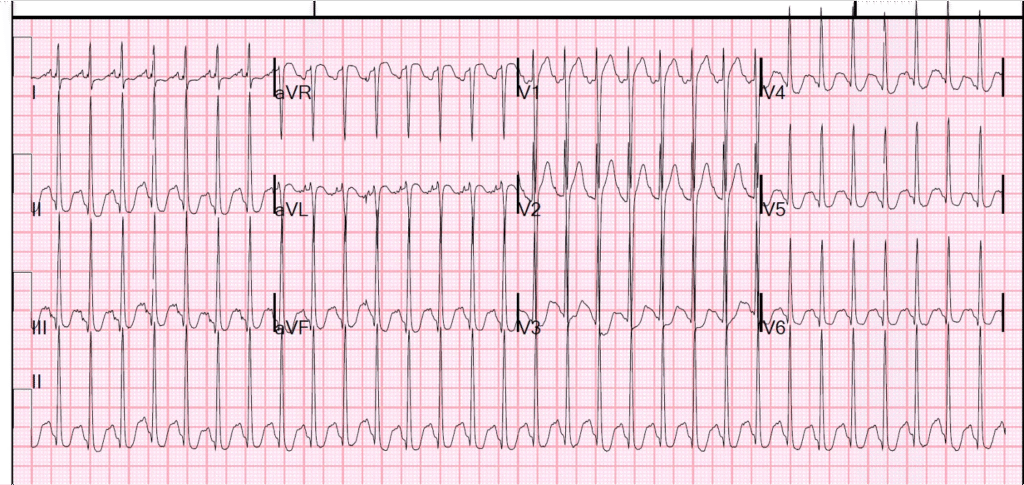
The patient arrived in the ED and had another ECG recorded:
What do you want to do?
This is SVT at a rate of 194. But remember that sinus tachycardia is a form of supraventricular tachycardia (SVT). So whenever you see “SVT”, look for P-waves because it might NOT be “Paroxysmal” SVT (PSVT), which would be AVNRT or AVRT (AVRT from WPW). Atrial flutter or Atrial tach are 2 other SVTs to think about.
The ED providers assumed PSVT and gave another dose of adenosine 12 mg without terminating the tachycardia.
(By the way, if you really think it is PSVT, and 12 mg fails twice, you can try 18 mg). But this case is simpler than that)
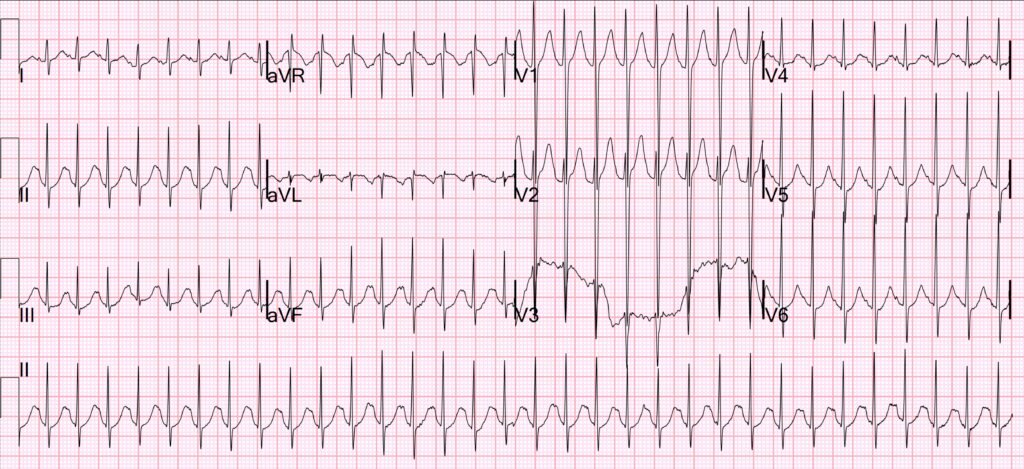
There are definite P-waves in multiple leads. Another clue to sinus tachycardia is that the patient was very agitated, which could be due to sympathomimetic overdose which causes sinus tach.
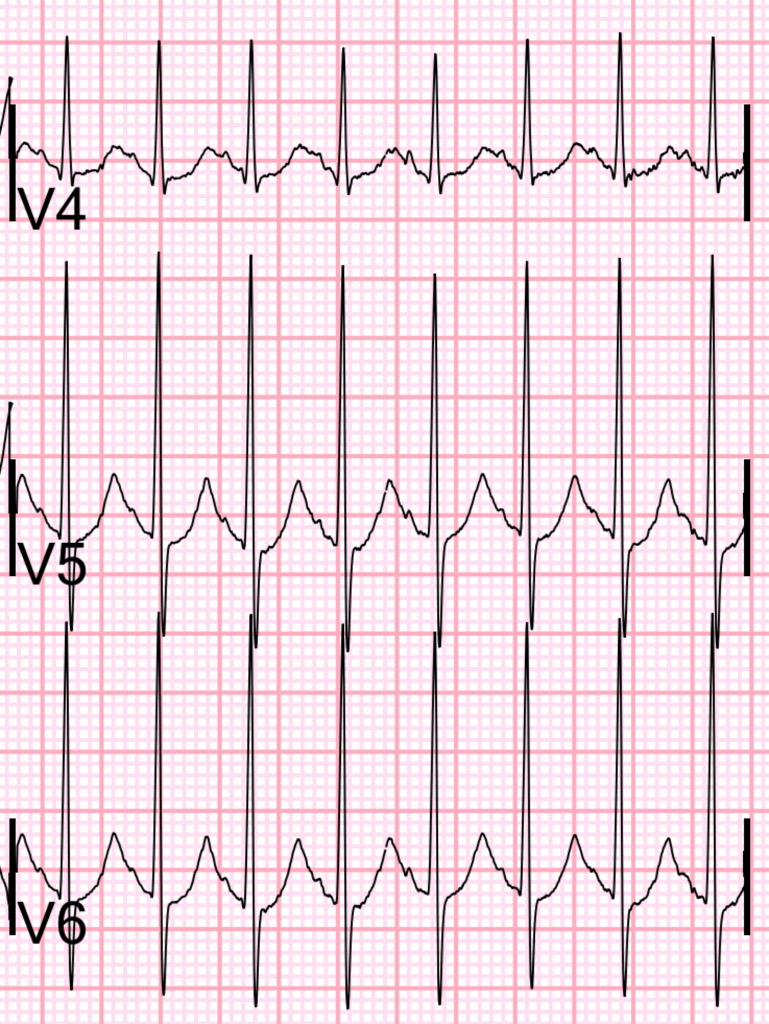
If we magnify the complexes, the are P-waves are obvious in leads I-III:
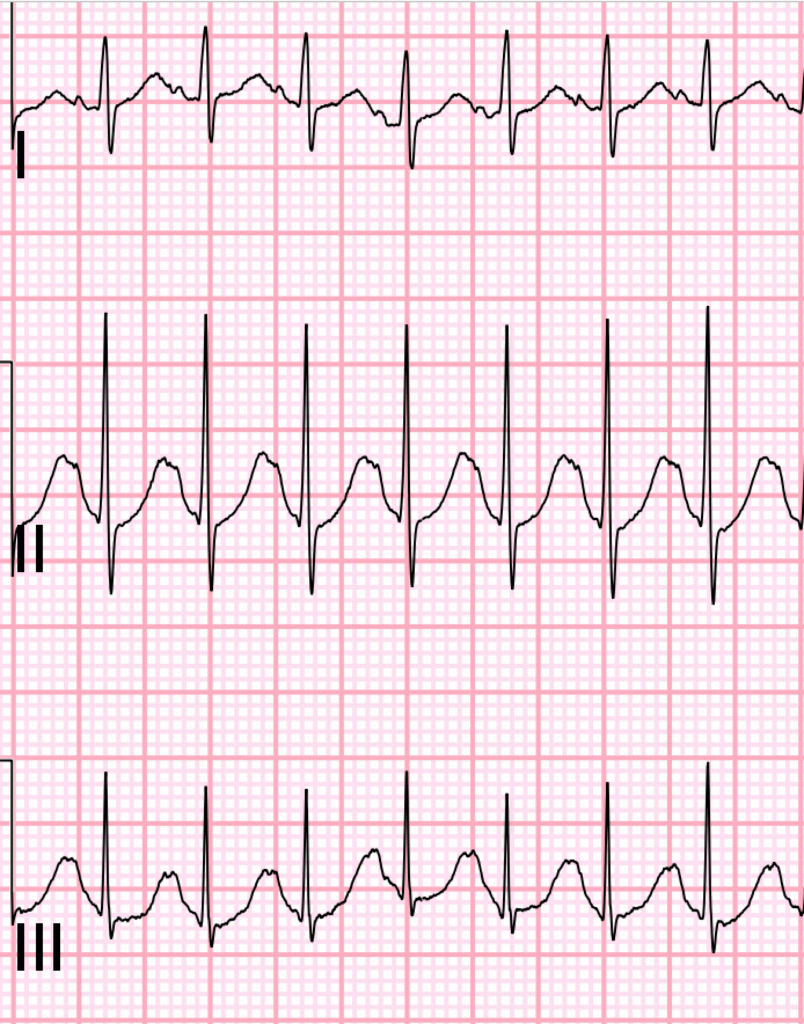
Lead V1:
And leads V4-6:
If you don’t see P-waves when there is SVT, then other signs of sinus tach are:
- Lewis leads. See this post for how to record Lewis Leads (this can be done using the monitor, NOT just the 12-lead ECG):
- A varying rate. re-entrant rhythms like PSVT stay at a constant rate. Automatic rhythms such as sinus tach vary from moment to moment.
- Give fluids. Usually this will decrease the rate.
- If you suspect sympathomimetic overdose, give benzodiazepines.
Case continued:
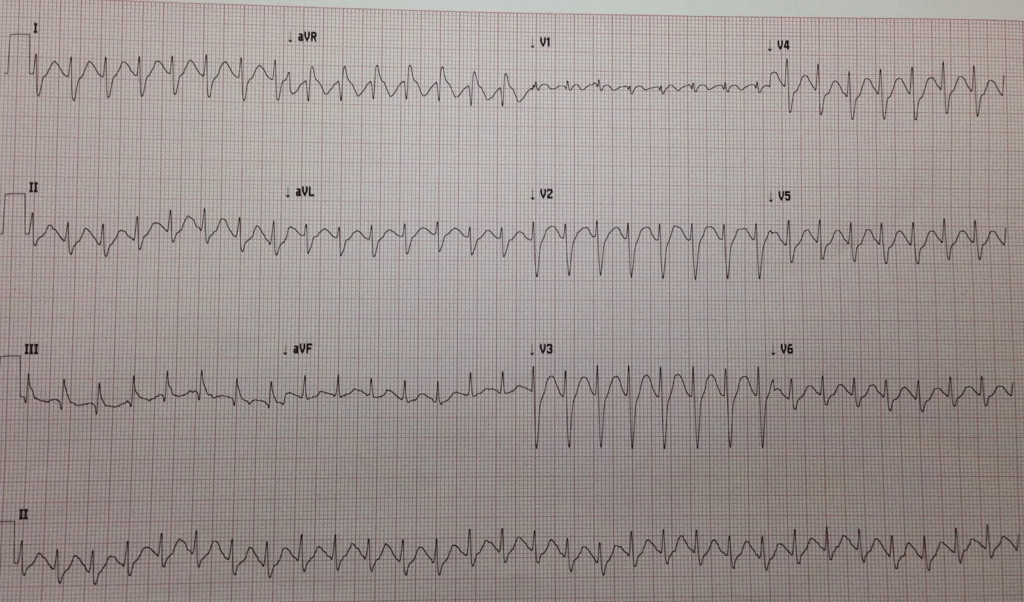
The patient was given fluids and benzodiazepines and the rate gradually decreased.
Cardiac function was good.
Drug screen confirmed amphetamines and cocaine.
Other cases of sinus tach mistaken for PSVT:
A young man with tachycardia. Should We Try Adenosine?
And this case:
= = =
======================================
MY Comment, by KEN GRAUER, MD (8/13/2025):
The history in today’s case is KEY:
- A 30-something man was transported to the ED for evaluation of marked agitation (ie, running through the street — yelling — and punching cars).
As per Dr. Smith — initial providers assumed the rhythm in this patient’s initial ECG was a reentry SVT rhythm — for which several doses of Adenosine were given “without terminating the tachycardia”.
- For clarity in Figure-1 — I’ve reproduced and labeled this initial ECG.
= = =
Additional Thoughts on Today’s CASE:
As per Dr. Smith — the term, “SVT” is a generic one that is all-too-often misunderstood and misused.
- The term, “SVT” stands for, SupraVentricular Tachycardia. This term therefore encompasses any tachycardia (ie, rhythm with a rate of ≥100/minute) — that is “supraventricular (ie, a rhythm originating from at or above the AV node).
- By this definition, the term “SVT” encompasses not only the common reentry SVT rhythms (AVNRT, AVRT) — but also AFib and AFlutter (if the ventricular rate of these rhythms is ≥100/minute) — Atrial Tachycardia — MAT — junctional tachycardia — and sinus tachycardia.
- Initial providers in today’s case made the mistake of “premature closure” — both in terms of diagnosis, as well as for treatment in the use of Adenosine.
- KEY Point: Far better than jumping to a specific rhythm diagnosis — is the approach of first describing the rhythm — then considering the differential diagnosis — and only then determining how comfortable you can be with your diagnostic impression. I do this in “real time” — which is as fast as any clinician who jumps to their diagnosis, and far more accurate.
= = =
Describing Today’s Rhythm:
The rhythm in Figure-1 is fast and regular.
- The QRS is narrow — so the rhythm is supraventricular.
- By the every-other-beat Method — the rate is ~200/minute (In Figure-1 — it takes 3 large boxes to record 2 beats — which means that half the rate = 300÷3 = 100/minute X 2 = 200/minute — See below for a brief Video Review of this Every-Other-Beat Method as the fastest way I know to accurately estimate rapid heart rates).
- Impression: The rhythm is Figure-1 is a regular SVT at ~200/minute. To remember that in addition to Atrial Tachycardia, Atrial Flutter and reentry SVT rhythms (AVNRT, AVRT) — the differential diagnosis of a regular SVT should always include Sinus Tachycardia!
= = =
Are P Waves Present in Figure-1?
As per Dr. Smith — P waves are present in Figure-1. Reasons it is so challenging to identify P waves in today’s tracing are: i) The very rapid heart rate; and, ii) That the 2 leads that are usually best for identifying P waves ( = lead II and lead V1) do not clearly show sinus P waves.
- The above said — P waves are seen in other leads (RED arrows in Figure-1). I’ve used YELLOW arrows for highlighting where I think P waves are also probably present.
- KEY Point: The fact that vertical time lines (dotted RED lines in Figure-1) line up perfectly for suspected atrial activity deflections in simultaneously-recorded leads confirms that my colored arrows are indeed sinus P waves.
= = =
Can Sinus Tachycardia be this Fast?
Most of the time in adults — sinus tachycardia in a non-exercising individual will not exceed ~170/minute.
- To Emphasize: There definitely are exceptions to this rate limit for sinus tachycardia in adults. In addition to hyperthyroidism and use of stimulant drugs — a previously healthy young adult who presents acutely ill may be under enough intrinsic catecholamine stimulation to manifest sinus tachycardia rates as fast (or even faster) than that seen in today’s case.
- All bets are off in kids! Although sinus tachycardia faster than ~170/minute is not commonly seen in non-exercising adults — the heart rate of sinus tachycardia in infants and young children can be surprisingly fast (ie, well over 200/minute).
- KEY Point: Today’s patient presented with marked agitation (ie, running through the street — yelling — and punching cars) — so clearly possible for him to develop an exceptionally rapid sinus tachycardia. And then the drug screen came back, confirming amphetamines.
= = =
Final Thought on Today’s Case:
We are told that several doses of Adenosine were given “without terminating the tachycardia”.
- Things happen FAST after Adenosine is given. The rate may slow — the SVT may convert and/or “telltale” P waves may appear, only to disappear seconds later. For this reason — it is essential to record the entire 60-to-90 seconds that follow administration of IV Adenosine — so that you have a hard copy record of what happened. I would bet that a hard copy recording after giving IV Adenosine in today’s case would reveal enough rate slowing to more clearly reveal the previously hidden sinus P waves.
= = =
=
Figure-1: I’ve labeled the initial ECG in today’s case.
=========================
Video Review — of the Every-Other-Beat Method for rapid determination of very fast heart rates. (NOTE: The first 1:25 of this video reviews rate determination in general. Start at 1:25 in this 3-minute video if you want to jump to the part for estimating very fast heart rates).
=