By Pendell Meyers
A woman in her 60s with multiple comorbidities presented to the ED with acute chest pain. Vitals were within normal limits. She described “burning” pain in the center of her chest, no radiation, and lightheadedness. Onset was within two hours of arrival.
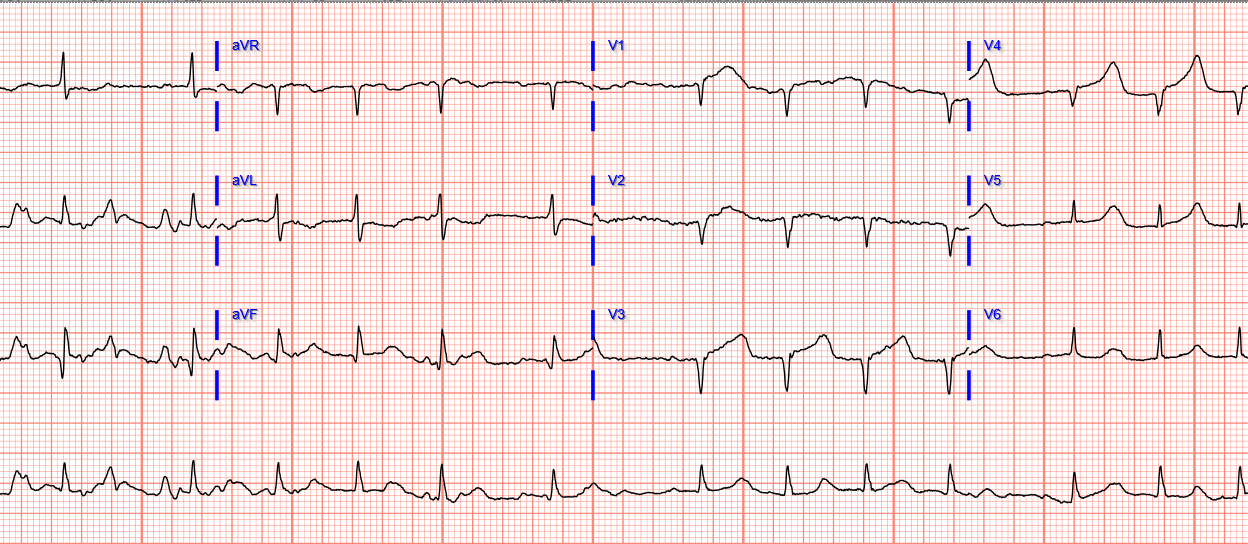
Here is her triage ECG (no prior available for comparison):
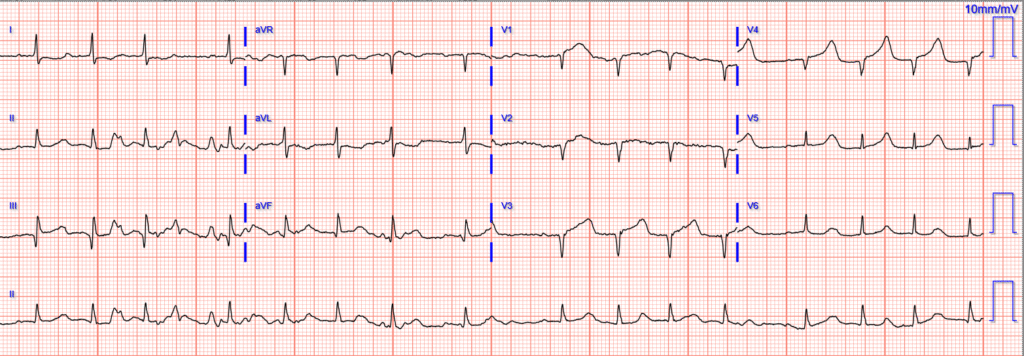
What do you think?
Here is the interpretation by the Queen of Hearts:

“STEMI Equivalent = Occlusion MI (OMI)”
The Queen sees at least anterior OMI with high confidence, with hyperacute T waves and some STE that doesn’t meet STEMI criteria.
New PMcardio for Individuals App 3.0 now includes the latest Queen of Hearts model and AI explainability (blue heatmaps)! Download now for iOS or Android. https://www.powerfulmedical.com/pmcardio-individuals/ It is not yet FDA approved, but is CE approved in the EU.
This ECG also meets our formal, explicit, published HATW score criteria in leads V4 and V5.
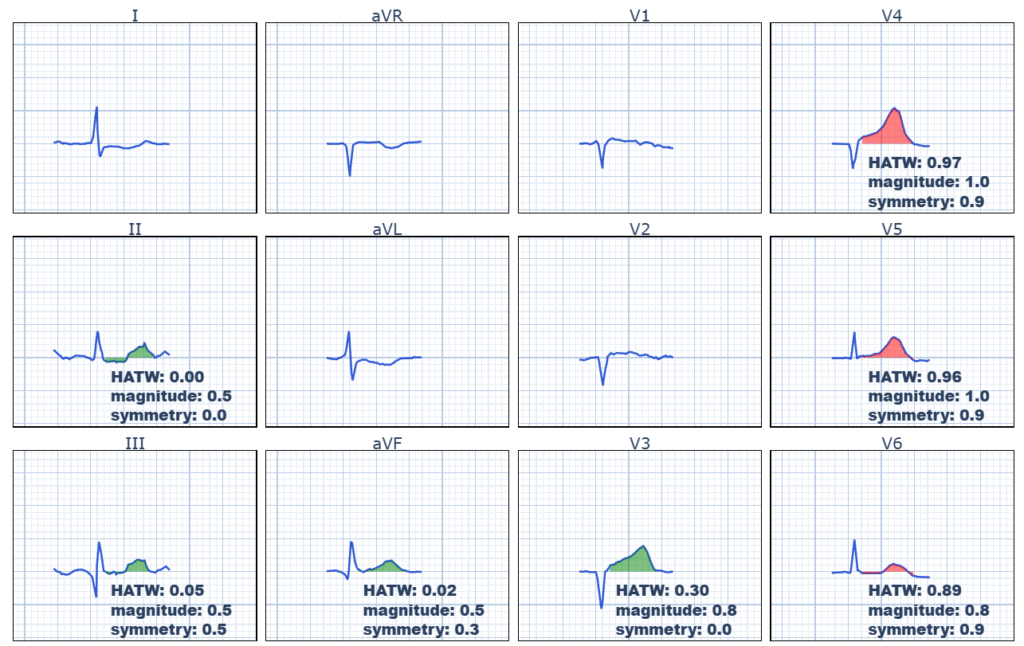
Reference here: Meyers HP, Simancik F, Herman R, Rafajdus A, Frick WH, de Alencar JN, Aslanger EK, Smith SW. Hyperacute T waves are specific for occlusion myocardial infarction, even without diagnostic ST elevation. JACC Adv. 2025. https://www.jacc.org/doi/10.1016/j.jacadv.2025.102120
Back to the case:
Her ECG was of course simply interpreted (correctly, according to the world’s definition of STEMI) as “No STEMI“, as there is not sufficient STE for STEMI criteria. Routine ED chest pain evaluation was begun from triage.
The first troponin returned at 1,410 ng/L.
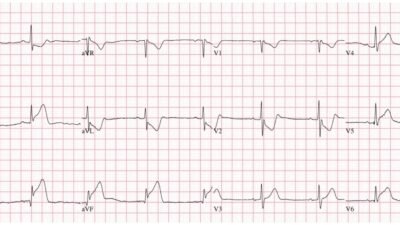
A repeat ECG was obtained at 93 minutes after the first ECG:
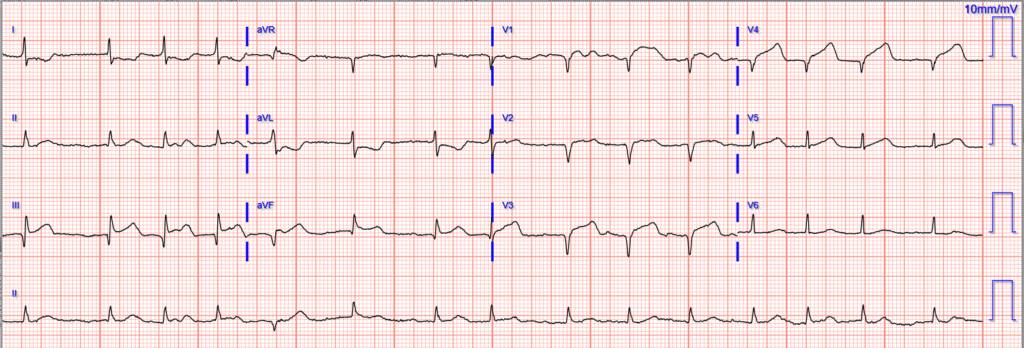
Obvious STEMI(+) OMI.
“STEMI” was diagnosed and the cath lab was activated.
Culprit was the mid LAD with TIMI 1 flow, which was stented.
Next troponins were
5k, 10k, >25K
Unfortunately, her cardiogenic shock progressed despite intervention and she died. Would 93 minutes earlier intervention have made a difference in this case?
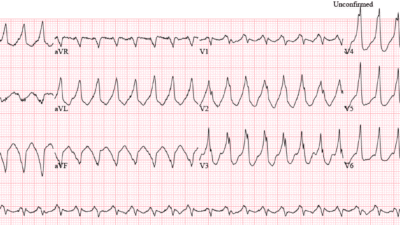
This case is not uncommon. We recently published this study showing that, of 808 cases of suspected ACS, 53 had total LAD occlusion. Only 33 met STEMI criteria on the first ECG; 20 did not. NONE of the 20 without STE ever developed diagnostic STE. 17/20 had hyperacute T-waves on the first ECG. In blinded reading, all 20 were identified on the first ECG by both Smith and by the Queen of Hearts.
Meyers HP, Sharkey SW, Herman R, de Alencar JN, Shroff GR, Frick WH, Smith SW. Failure of standard contemporary ST-elevation myocardial infarction electrocardiogram criteria to reliably identify acute coronary occlusion of the left anterior descending coronary artery. EHJ: ACC (2025) 00,1-9. https://doi.org/10.1093/ehjacc/zuaf037
= = =
======================================
MY Comment, by KEN GRAUER, MD (10/12/2025):
I found it difficult to review today’s case. While we do not know if prompt recognition of today’s 1st tracing, followed by immediate cath lab activation might have altered the unfortunate outcome — the need to learn from events in this case begs review regardless.
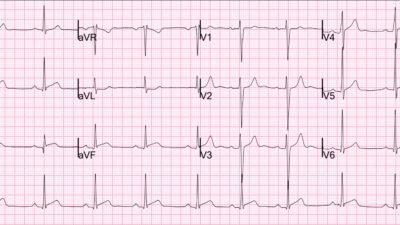
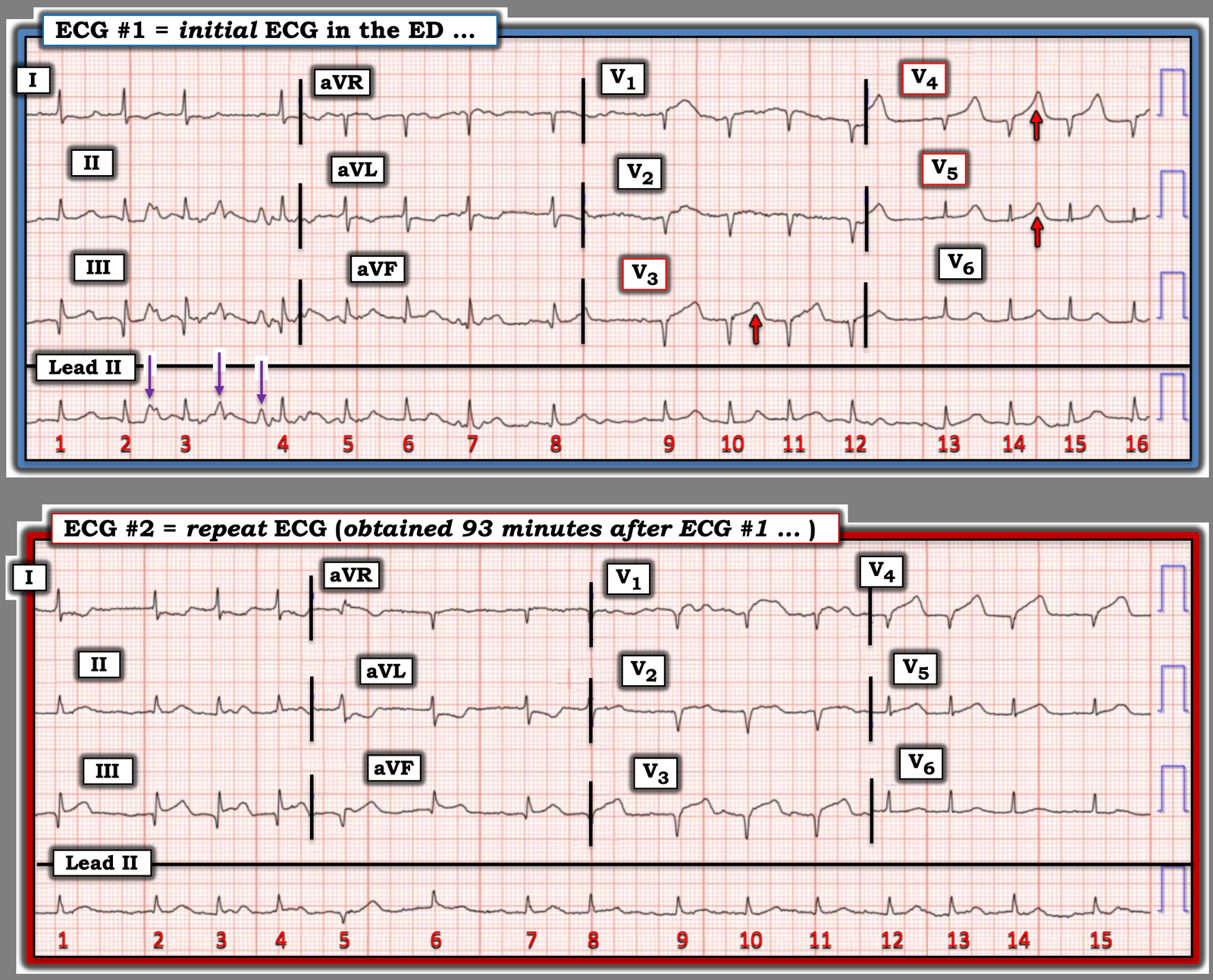
- For clarity and ease of comparison in Figure-1 — I’ve put the 2 ECGs in today’s case next to each other.
= = =
QUESTIONS:
Take another LOOK at today’s initial ECG in Figure-1:
- What do the PURPLE arrows in Figure-1 represent?
- Did today’s patient have a previous anterior MI?
- After seeing the initial ECG — What are your thoughts regarding today’s case?
= = =
Figure-1: Comparison between the 2 ECGs in today’s case …
= = =
My Thoughts regarding the above Questions:
Looking first at the initial ECG in Figure-1:
- I generally favor beginning my assessment with a quick look at the long lead rhythm strip. Doing so — I was initially confused by the 3 pointed, upright deflections highlighted by PURPLE arrows between beats #2-to-#4. Although these deflections look large enough to be QRS complexes — their placement would not make physiologic sense if this were true, given that there are 2 of these complexes between beats #3-4, with subsequent occurrence of beat #4 shortly thereafter.
- Instead — I was struck by: i) Near equal size for these deflections in leads II and III — but no hint of any deflections in simultaneously-recorded lead I; — and, ii) Total disappearance of these deflections after beat #4 in the long lead II rhythm strip. The above observations tell us that the 3 PURPLE arrows in ECG #1 represent artifact — most likely arising from some brief movement in the left foot that resolved after beat #4 (See My Comment in the December 5, 2022 post re determinal of the “culprit” extremity — and click HERE if interested in a series of additional examples of artifact).
Proceding with interpretation of ECG #1 — now that we’ve determined that the 3 PURPLE arrow deflections represent artifact:
- The rhythm in this initial ECG is irregularly irregular with intermittent baseline deflections, but no P waves. This is AFib (Atrial Fibrillation) with a controlled ventricular response.
- A deep but narrow Q wave is seen in lead III, with a smaller Q wave in lead aVF. That said — I was uncertain about the significance of these findings given the large amount of baseline artifact in these limb leads (old or recent MI?). ST depression with shallow T wave inversion in leads I and aVL increased my concern — but I thought these findings were non-diagnostic and difficult to assess.
- The most remarkable findings in ECG #1 are in the chest leads. QS complexes are present in leads V1-thru-V4 — which clearly indicates anterior infarction at some point in time.
- That said — it is the T waves in leads V3,V4,V5 that need to “catch our eye” (RED arrows in these leads). These are clearly hyperacute T waves (ie, disproportionately taller-than-they-should-be — and — much wider-at-their-base than expected, especially given very modest size of the QRS complexes in these leads).
= = =
My Impression of ECG #1:
- Given the history in today’s case (ie, a woman in her 60s with multiple comorbidities — who presents to the ED with acute chest pain that began 2 hours earlier) — this initial ECG is extremely worrisome.
- Unfortunately — no prior ECG was available for comparison at the time ECG #1 was recorded. As a result — we don’t know if this patient had a previous inferior and/or previous anterior infarction. That said — there is no way that the T waves in leads V3,V4,V5 can be normal. Given the history of CP that began just 2 hours earlier — this has to be assumed as acute LAD occlusion until proven otherwise (ie, with call for acute cath lab activation).
- NOTE: Although the deep QS complexes that we see in leads V1-thru-V4 usually take more than the 2 hours that this patient has had CP for to develop — on occasion, even large Q waves can develop in as little as a few hours. But regardless of whether there is a new anterior MI superimposed on a previous anterior MI — vs no previous MI, but instead a single new extensive ongoing infarction — the approach to management is the same = the need for prompt cath lab activation.
- That said — Should there be any doubt about acuity of the ST-T wave changes that we see in ECG #1 — then a repeat ECG should have been done long before the 93 minutes that transpired until ECG #2 was obtained (ie, given new-onset CP of only 2 hours duration and the hyperacute T waves that we evident in leads V3,V4,V5 — a repeat ECG should have been ordered in no more the 15 minutes after ECG #1 was done).
- P.S.: Be aware that IF this patient’s AFib is new — the occurrence of this arrhythmia as a result of an acute MI is an additional worrisome prognostic factor that may predispose to heart failure and shock. Effort should be made to expedite obtaining this patient’s prior medical record (especially the most recent previous ECGs to see if anterior infarction and AFib are new or old).
= = =
Comparison with ECG #2:
Optimal assessment of serial ECGs is best achieved by placing both tracings next to each other as shown in Figure-1 — and then looking lead-by-lead for changes:
- The rhythm in ECG #2 is again AFib — with a similar ventricular response as was seen for ECG #1. Beat #5 is a PVC.
- Artifact is negligible in this repeat ECG. We can now clearly appreciate that ST elevation in leads II and III is real — and accompanied with more pronounced reciprocal ST depression in leads I and aVL. This is diagnostic of acute inferior MI.
- Comparison between the 2 tracings of chest lead ST-T wave changes in leads V3,V4,V5 is insightful as to the evolving morphology of a large anterior infarction in progress (ie, Note how the overly tall hyperacute T waves from ECG #1 — have now in ECG #2 increased the amount of J-point ST elevation and inflated the previously concave up ST segments from ECG #1 into full, tombstone-like coving in leads V3,V4 of ECG #2).
- Learning Points: In today’s patient who presented with new CP — the “picture” of the T waves in leads V3,V4,V5 of ECG #1 should be recognized as hyperacute. This finding should have been more than enough to initiate immediate cath lab activation regardless of whether or not STEMI criteria are satisfied. And if providers have any doubt — the initial ECG should be repeated within 15 minutes (and will almost certainly show additional diagnostic changes).
= = =