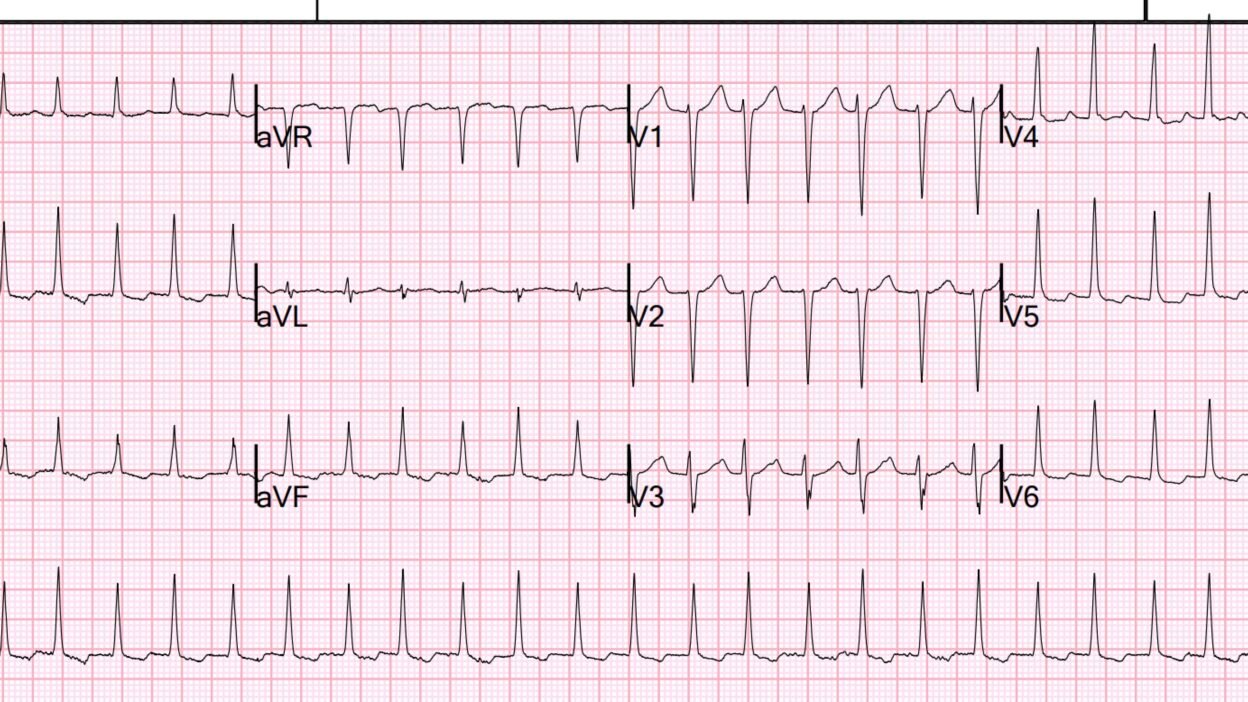
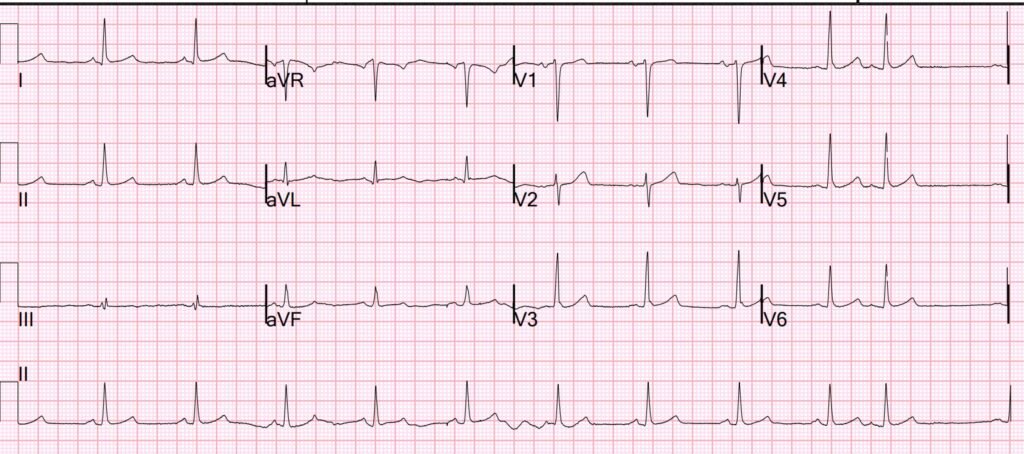
A 50-something male presented with palpitations. He had a fever and hypotension (BP 80/40). His volume status was low by ultrasound (flat IVC), and he had good LV function. He had no B lines. He had a history atrial fibrillaton and ablation, but has been in sinus rhythm recently. IV fluids were given, and because of his heart rate of 190 bpm, this ECG was recorded:
Heart rate 156. What do you think?
There is a narrow complex tachycardia without P waves (you must look carefully for P waves!! Especially in a patient with fever (thus, supraventricular tachycardia, or SVT). It could be Atrial flutter, AVNRT, AVRT (WPW), or atrial tachycardia. There are no flutter wavies. It is not irregularly irregular, so it is NOT atrial fibrillation. It is however, regularly irregular, as there are 2 different RR intervals (and each with its own voltage amplitude!). One RR interval is 360 ms, the other is 400 ms. I don’t see any P-wave or even retrograde P-waves, and sinus tach at 190 would be very unusual for a 50-something.
An aside, not critical to management: The differing RR intervals suggests PSVT (paroxysmal SVT) due to AVNRT with triple AV nodal pathways. See this amazing case of dual AV nodal pathways in addition to a 3rd pathway which is an accessory pathway (WPW) and an explanation and diagram of what it means. All AVNRT has 2 pathways, one fast and one slow. In this case, in order to have 2 different speeds, and since there is no accessory pathway, the third pathway is within the AV node. There is likely one fast pathway and 2 slow ones. See this article: Typical Atrioventricular Nodal Re-Entry Tachycardia Masquerading as Atrial Fibrillation.
What would you do?
Adenosine is a good choice, and so is electricity. Electricity requires deep sedation, which takes more time than adenosine, so I would start with adenosine.
The providers gave adenosine. It converted to sinus rhythm, and then rapidly reverted to the above rhythm.
What would you do now?
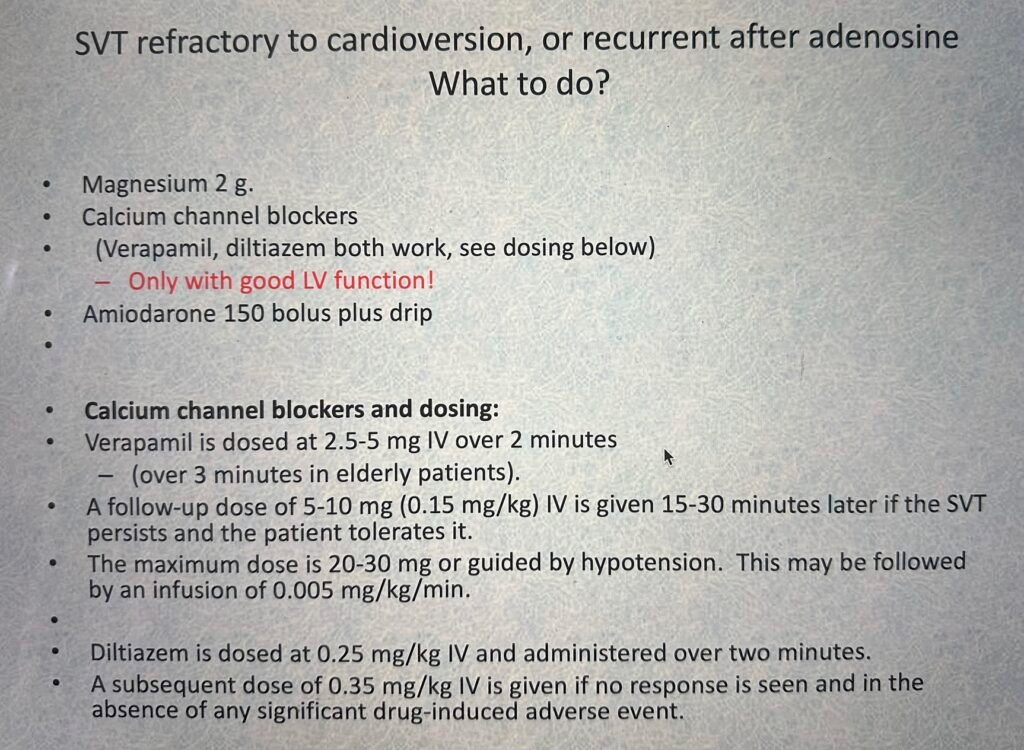
Because it reverted, there is no point in giving a treatment that only lasts seconds, as it will just revert AGAIN. This means that neither electricity nor adenosine will result in sustained sinus rhythm.
The providers tried adenosine 2 more times, and each time the rhythm converted to sinus then reverted to SVT. They then tried electrical cardioversion (this is pointless!). Both times it converted then reverted. Cardiology was consulted and they recommended amiodarone bolus and drip. This had no effect.
The patient remained hypotensive after fluids.
I came on duty in the ED at this point in time. My practice is that, when SVT reverts, I first make certain that the K and Mg are replenished and if this does not prevent reversion, and if there is good LV function, then I want to give an AV nodal blocker that will persist (adenosine and electricity are both gone quickly). That means a calcium channel blocker (verapamil or diltiazem). When I first started EM, there was no adenosine and we always gave verapamil for SVT. It works and the data shows it is pretty safe (a meta-analysis with 4% hypotension vs. 1% with adenosine).
Only give a calcium channel blocker if LV function is good!! They diminish contractility and can lead to shock in a patient with poor LV function.
The patient was already on amiodarone drip and bolus. So I suggested we first try electrical cardioversion to see if the amiodarone would keep the patient in sinus. The patient converted to sinus and again reverted within seconds to SVT.
So we stopped the amiodarone. We started a phenylephrine infusion for the hypotension prior to giving a calcium channel blocker which could exacerbate hypotension. We used phenylephrine in order to avoid the beta stimulation of norepinephrine – beta stimulation could make it more difficult to control SVT). After the BP increased to 105/70, we gave a diltiazem bolus (not verapamil only because we do not stock it in the ED) and there was immediate and sustained conversion to sinus rhythm.
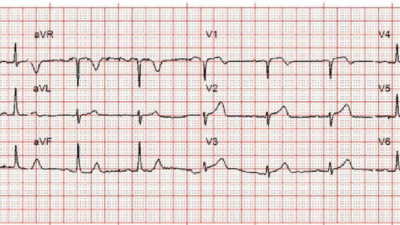
= = Sin=Sinus rhythm at a rate of 66.
A diltiazem infusion was also started.
A Chest X-ray confirmed pneumonia. The patient remained hypotensive. Notice there is absence of appropriate reflex sinus tachcardia, as one would both desire (in order to improve cardiac output) and expect (as happens is sepsis with hypotension). This relative sinus bradycardia is of course due to the diltiazem, which slows the sinus rate. Because of this, the patient continued to require phenylephrine for blood pressure support.
The patient ultimately did well.
Here are some guidelines for SVT management. Then see the other cases below:
Here is a case that had sustained sinus rhythm after giving magnesium. Good literature review here.
Here is a case in which I tried beta blockade (esmolol) but it failed and amiodarone did work. (I should have given a calcium channel blocker)
= = = =
======================================
MY Comment, by KEN GRAUER, MD (1/7/2026):
Today’s case by Dr. Smith highlights a series of important points regarding assessment and management of reentry SVT (SupraVentricular Tachycardia) rhythms. These points include the following:
- The history may be insightful. The patient in today’s case had AFib in the past — that was successfully ablated. As noted by Romero et al (Heart Rhythm 4(11):1637-1646, 2017) — Catheter ablation of AFib may predispose to the subsequent development of a reentry SVT rhythm (ie, AVNRT, AVRT) by altering conduction pathway properties, thereby potentially facilitating development and maintenance of a reentry circuit.
It’s EASY to overlook the underlying pattern of today’s rhythm. For example, when you first saw today’s rhythm — Did YOU think the rhythm was regular?
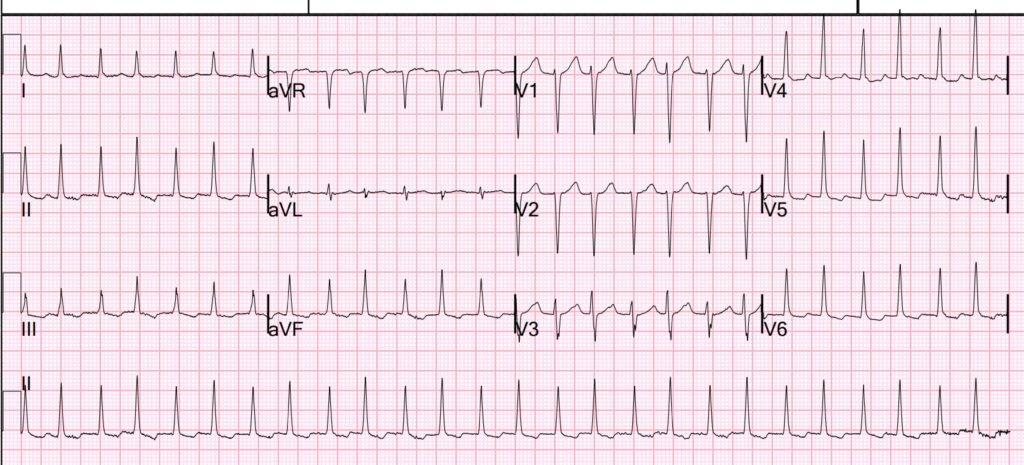
- As per Dr. Smith — Today’s rhythm is not regular. Instead — there is a regular irregularity, in the form of a repetitive pattern in which slightly longer R-R intervals alternate with slightly shorter R-R intervals (ie, R-R intervals in Figure-1 that begin with even-numbered beats are slightly longer than R-R intervals beginning with odd-numbered beats).
- Even without calipers — this irregular irreglarity can be appreciated if you focus for a moment on the long lead II rhythm strip that appears below the 12-lead ECG in Figure-1.
- Recognition that this narrow complex (therefore supraventricular) tachycardia has a repetitive pattern — immediatelly limits the differential diagnosis by ruling out sinus tachycardia and atrial fibrillation.
- AFlutter and ATach are also unlikely — since although Wenckebach conduction may be associated with these 2 SVT rhythms, the subtle every-other-beat variation in R-R interval at the rapid rate seen in Figure-1 is much more typical of a reentry SVT (either AVNRT or AVRT).
= = =
Figure-1: I’ve reproduced today’s ECG — with my proposed laddergram.

= = =
Is there Atrial Activity?
- Normal sinus P waves are clearly absent in Figure-1. However, there is beat-to-beat variation in the ST segments that to me suggests that there may be some form of atrial activity hidden within.
- I thought a pattern of alternate beat ST segment variation was best suggested in lead V3 (within the BLUE rectangle in Figure-1) — albeit this pattern is not consistently seen in other leads.
- In addition to this hint of retrograde atrial conduction — there appears to be electrical alternans in a number of leads in Figure-1 (ie, alternate beat variation in QRS morphology seen best in lead V3 — but also consistenly seen in leads II,aVF; and in V4,V5,V6 in the form of alternating QRS amplitude).
- As I review in detail in the November 28, 2022 post of Dr. Smith’s ECG Blog (in My Comment at the bottom of the page) — the presence of electrical alternans increases the likelihood of a reentry SVT rhythm.
= = =
The Mechanism of Today’s Rhythm
Why then do we see alternating R-R intervals in today’s reentry SVT?
- Against Wenckebach conduction is the lack of a dropped beat.
- Instead — I suspect the presence of dual AV Nodal pathways, each with its own speed of retrograde conduction is the reason for persistence of alternating R-R intervals in today’s rhythm.
- The theoretical laddergram I propose in my above Figure-1 illustrates one pathway with slightly slower retrograde conduction (PURPLE broken lines) alternating with a second pathway with slightly faster retrograde conduction (RED broken lines).
= = =
KEY Points in Management:
Dr. Smith’s above discussion highlights the relevance of recognizing that today’s rhythm is indeed a reentry SVT.
- Adenosine was given — and promptly converted the SVT (as it almost always does for reentry SVT rhythms). Sometimes this is all that is needed. However, in today’s case — the rhythm promptly reverted to the reentry SVT.
- The immediate conversion of today’s rhythm after the initial dose of Adenosine strongly supports the premise that the rhythm is a reentry SVT (AVNRT or AVRT).
- Rapid reversion back to the reentry SVT tells us that neither repeat Adenosine doses nor cardioversion will succeed in maintaining sinus rhythm. Instead — a longer-acting drug ( = IV Diltiazem in today’s case) will be needed to maintain sinus rhythm.
PEARL: Remember to always record a long lead rhythm strip for the 60-to-90 seconds after giving Adenosine! This is because things happen quickly after you give Adenosine — and it is EASY to miss the important fact that the Adenosine did its job and converted the rhythm to sinus unless you have a hard copy recording that you can look at.
- Otherwise, all the “action” will be over in seconds and you may easily miss the momentary conversion to sinus rhythm because your eyes were on the patient.
- The moment we see that Adenosine did its job — but that the patient immediately reverted back to the SVT — we know it’s time to stop giving Adenosine, and instead use a long-acting agent.
= = =
= = =