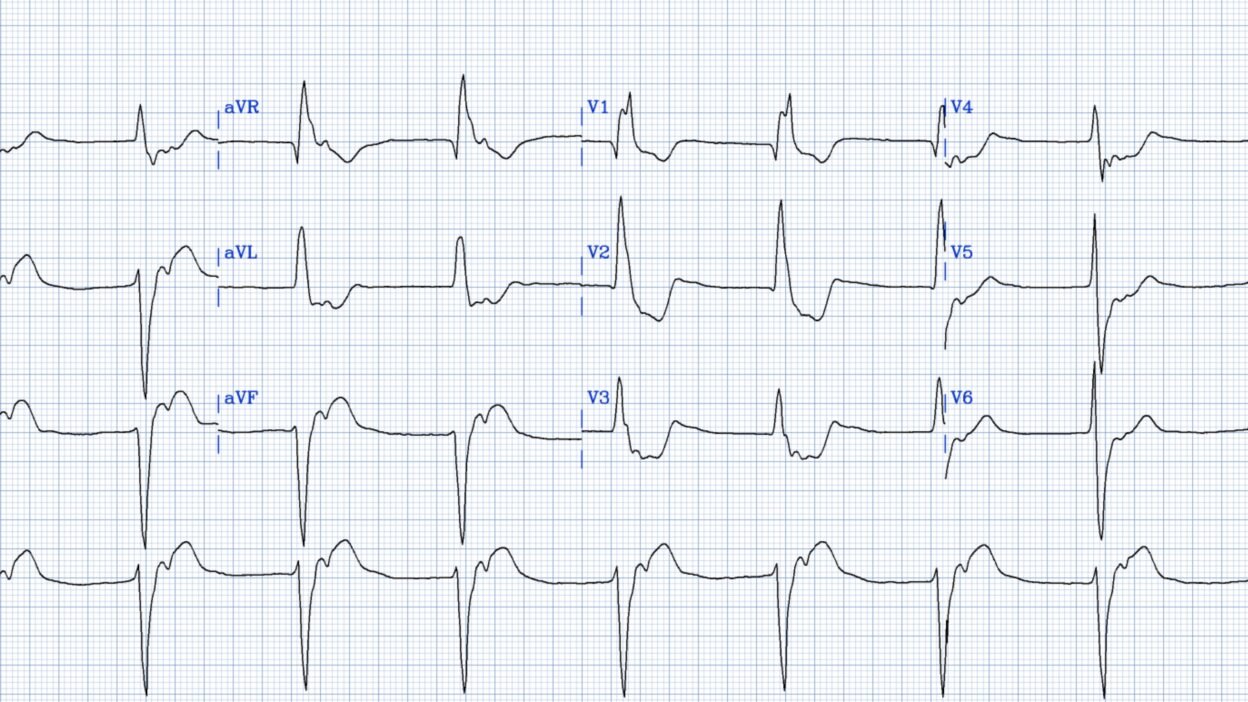
I came across this interesting ECG without clinical context:
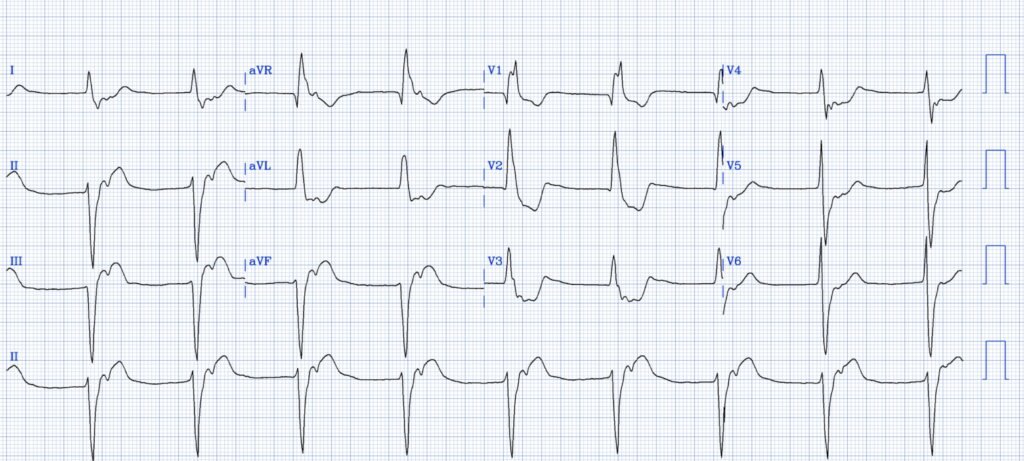
What do you think?
Rhythm: This appears to me to be accelerated idioventricular rhythm (AIVR) [vs. junctional rhythm/escape with RBBB and LAFB] — (see Ken’s extensive discussion below). There are no P-waves. The ventricle is triggering at a rate faster than a slow sinus node. And you can also see retrograde P-waves following every QRS. How do I know it is AIVR? Wide, regular, slow (cannot be VT). It is escaping with a morphology of RBBB/LAFB, which means that it is escaping from the left posterior fascicle.
What else? Even though precordial leads resemble RBBB, the QRS in limb leads resemble LBBB, and so I would evaluate the limb leads using the Smith Modified Sgarbossa Criteria. Thus, there should be normal proportional (to the QRS) discordant ST Elevation in leads with a negative QRS (e.g., lead III). It is difficult to tell exactly where is the J-point in inferior leads, but I think it is at about 5mm in lead III, which makes the ST/S ratio = 25%. Thus, there is excessively discordant STE in lead III, and excessively discordant reciprocal STD in lead aVL (30%).
In precordial leads, which resemble RBBB, the ST depression in V2-3 is out of proportion (> 30%). The QRS is isoelectric in V4 (R-wave and S-wave the same voltage) and so there should be an isoelectric ST segment. But it is very depressed. Same for V5.
So this is diagnostic of LBBB OMI. The AIVR suggests that this is reperfusing, as AIVR is a reperfusion rhythm.
I don’t know for sure, but I believe that this is the ECG of an inferior posterior OMI that just underwent PCI minutes ago, and there is still a lot of residual ST-T ischemia that I suspect will resolve within minutes.
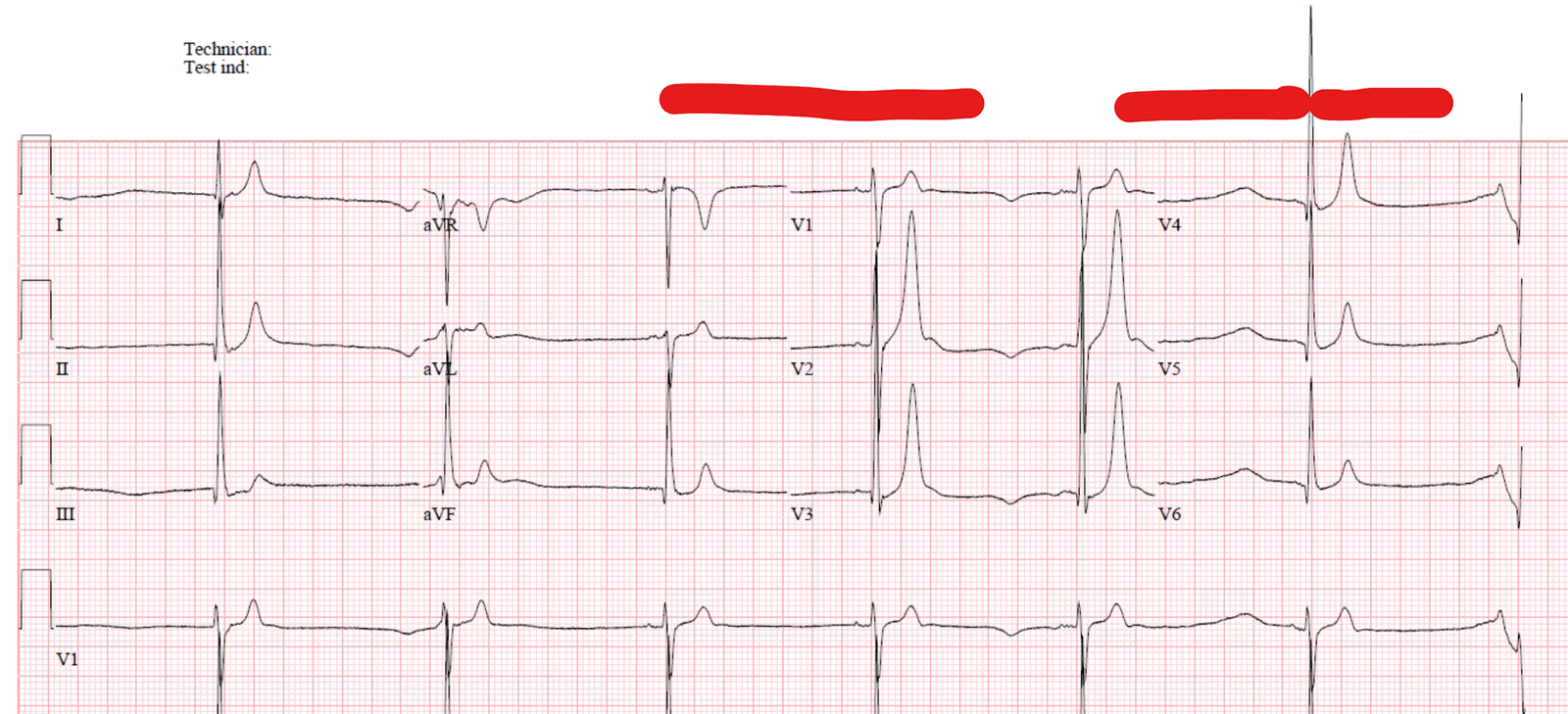
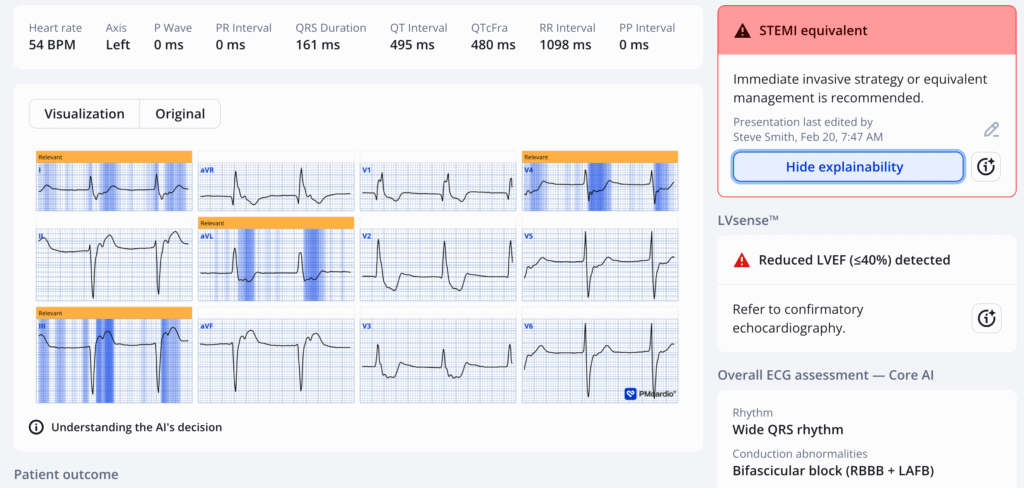
Here is the PMCardio Queen of Hearts interpretation:
= = =
New PMcardio for Individuals App 3.0 now includes the latest Queen of Hearts model and AI explainability (blue heatmaps)! Download now for iOS or Android. https://www.powerfulmedical.com/pmcardio-individuals/ (Drs. Smith and Meyers trained the AI Model and are shareholders in Powerful Medical). As a member of our community, you can use the code DRSMITH20 to get an exclusive 20% off your first year of the annual subscription. Disclaimer: PMcardio is CE-certified for marketing in the European Union and the United Kingdom. PMcardio technology has not yet been cleared by the US Food and Drug Administration (FDA) for clinical use in the USA.
======================================
MY Comment, by KEN GRAUER, MD (2/15/2025):
Clinical interpretation of ECGs requires a history. That history can be brief (usually no more than 1-to-3 lines are all that is needed) — but without a brief relevant history, we are reduced to guessing what the true significance of any tracing might be.
- The above said — many (most) of us at least occasionally encounter a number of tracings that we need to interpret without the benefit of any history.
- I view interpretation of such tracings as extremely challenging — as this forces us to envision how our clinical assessment might differ, depending on whether the patient was having acute CP (Chest Pain) — or recently had CP that is no longer present — or — had this ECG done for some other reason.
= = =
There is no history in today’s case.
- So — How did YOU approach interpretation of today’s ECG? Hopefully you challenged yourself before you looked at Dr. Smith’s masterful interpretation . . .
= = =
My Thoughts …
- Suggestion: As for the interpretation of any tracing — I favor beginning with a systematic description of what we see. Doing so does not prolong the process of interpretation. On the contrary, routinely applying a systematic approach is a most time-efficient method for interpretating ECGs, with the added benefit that systematic interpretation prevents overlooking alternative possibilities.
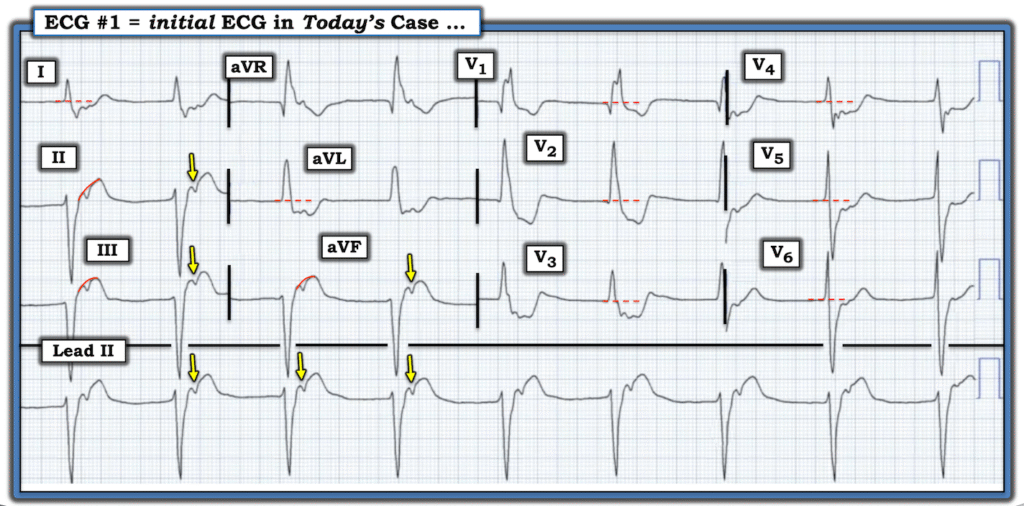
I’ve labeled today’s ECG in Figure-1. By the P‘s,Q‘s,3R Approach that I favor for rhythm interpretation (which I review HERE in ECG Video #1) — My considerations regarding today’s rhythm are as follows:
- NOTE: The sequence for how I address the 5 parameters in the Ps,Qs,3R Approach is not important — and I often vary the order in which I assess for the presence of P waves — QRS width — and the 3Rs (Rate and Regularity of the rhythm — and if atrial activity is present, whether such atrial activity is [or is not] Related to neighboring QRS complexes).
- In Figure-1 — the QRS complex is wide. It might not necessarily look wide in some of the chest leads — but in leads like V1, it is apparent that the QRS easily exceeds 0.12 second in duration.
- The ventricular rhythm is Regular — with an R-R interval of ~5.5 large boxes in duration (ie, at a ventricular Rate of ~55/minute).
- P waves are present — and as per the YELLOW arrows that I’ve drawn in Figure-1, P waves are clearly Related to the QRS complex that precedes them (best seen in the long lead II rhythm strip — which confirms 1:1 retrograde conduction of these P waves by the fixed RP’ interval that is present).
- To Emphasize: The finding of 1:1 V-A (ie, retrograde) atrial activity does not represent “AV dissociation” — because the retrograde P waves in Figure-1 are related to neighboring QRS complexes by the constant RP’ interval. When there is AV dissociation — then P waves are not related in any way to neighboring QRS complexes.
= = =
So WHY is the QRS Wide in Today’s ECG?
I was not initially certain of the answer to this question.
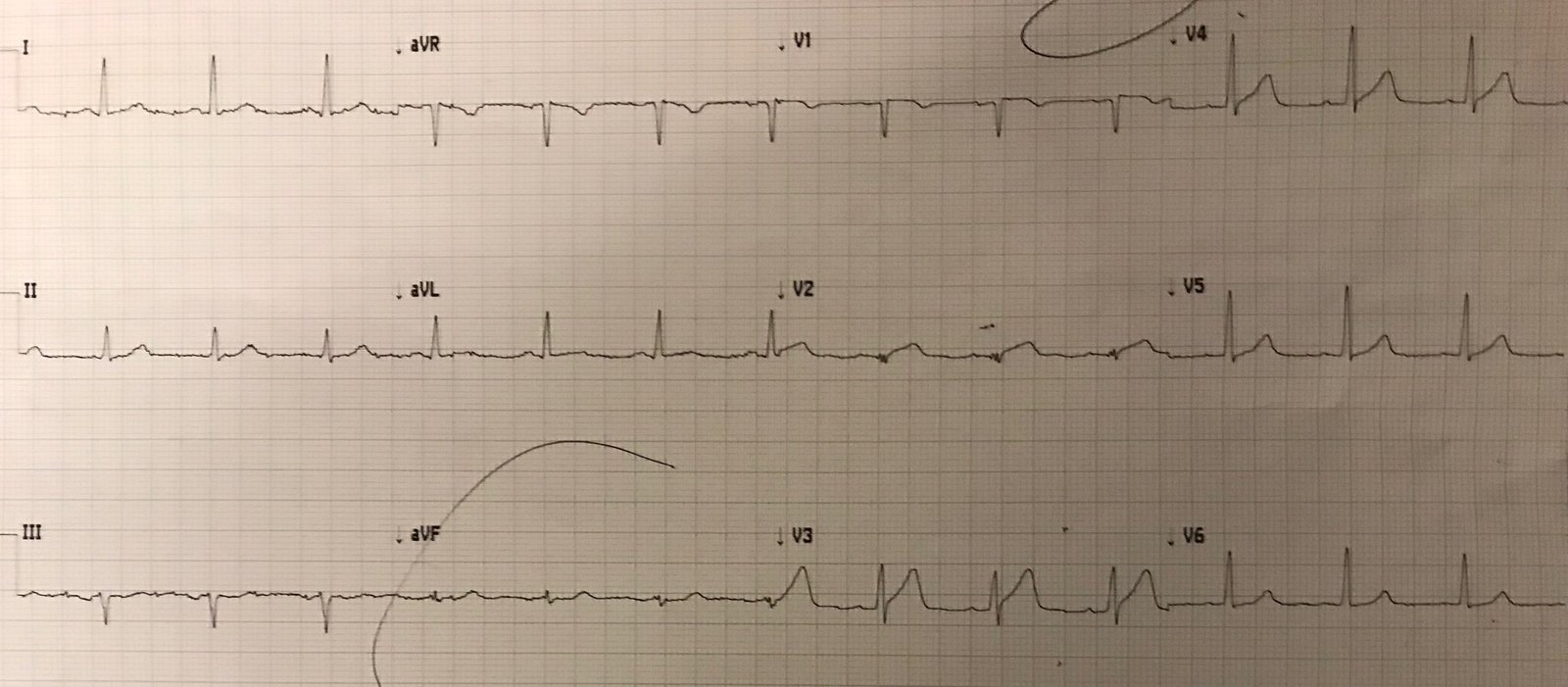
- 1:1 retrograde conduction can be seen with either ventricular or supraventricular rhythms. As a result — I could not rule out the possibility of a junctional rhythm in today’s ECG, in which there is preexisting bifascicular block ( = RBBB/LAHB).
- The above said — I completely agree with Dr. Smith’s assessment, in that in the absence of a prior ECG for comparison — a ventricular etiology seems far more likely because: i) The very wide QRS with no more than a small terminal S wave in lead I, and no more than tiny initial r waves in the inferior leads — “looks” much more like a ventricular rhythm; — and, ii) As per Dr. Smith — the presence of a slightly accelerated ventricular rhythm is most commonly seen as a reperfusion arrhythmia following a recent MI.
= = =
How to Define AIVR:
Distinction between an idioventricular “escape” rhythm — vs — AIVR ( = an Accelerated IdioVentricular Rhythm) — vs — VT (Ventricular Tachycardia) — is best made by attention to: i) The clinical setting; — and, ii) The rate of the ventricular rhythm.
- AIVR is an “enhanced” ventricular ectopic rhythm that occurs faster than the intrinsic (idioventricular) ventricular escape rate (which in adults is ~20-40/minute) — and slower than hemodynamically significant Ventricular Tachycardia (ie, VT that generally presents at rates >130-140/minute).
- The usual rate of AIVR is therefore between ~60-110/minute (with an area of “overlap” between AIVR and fast VT at ~110-130/minute).
- Conclusion: The rhythm in today’s case is therefore best described as AIVR — with a ventricular rate that is clearly faster than the usual 20-40/minute “escape” rate — yet noticeably slower than the usual ≥130-140/minute that generally marks the threshhold for hemodynamically signficant VT.
= = =
Evidence in Today’s Case for a Recent MI:
Although it is clearly more difficult in a ventricular rhythm to recognize and assess the potential significance of abnormal-appearing ST-T waves — there are times when such changes are diagnostic of an acute OMI! (See My Comment at the bottom of the page in the April 8, 2022 post and in the April 6, 2025 post). This most probably also reflects what we are seeing in today’s case:
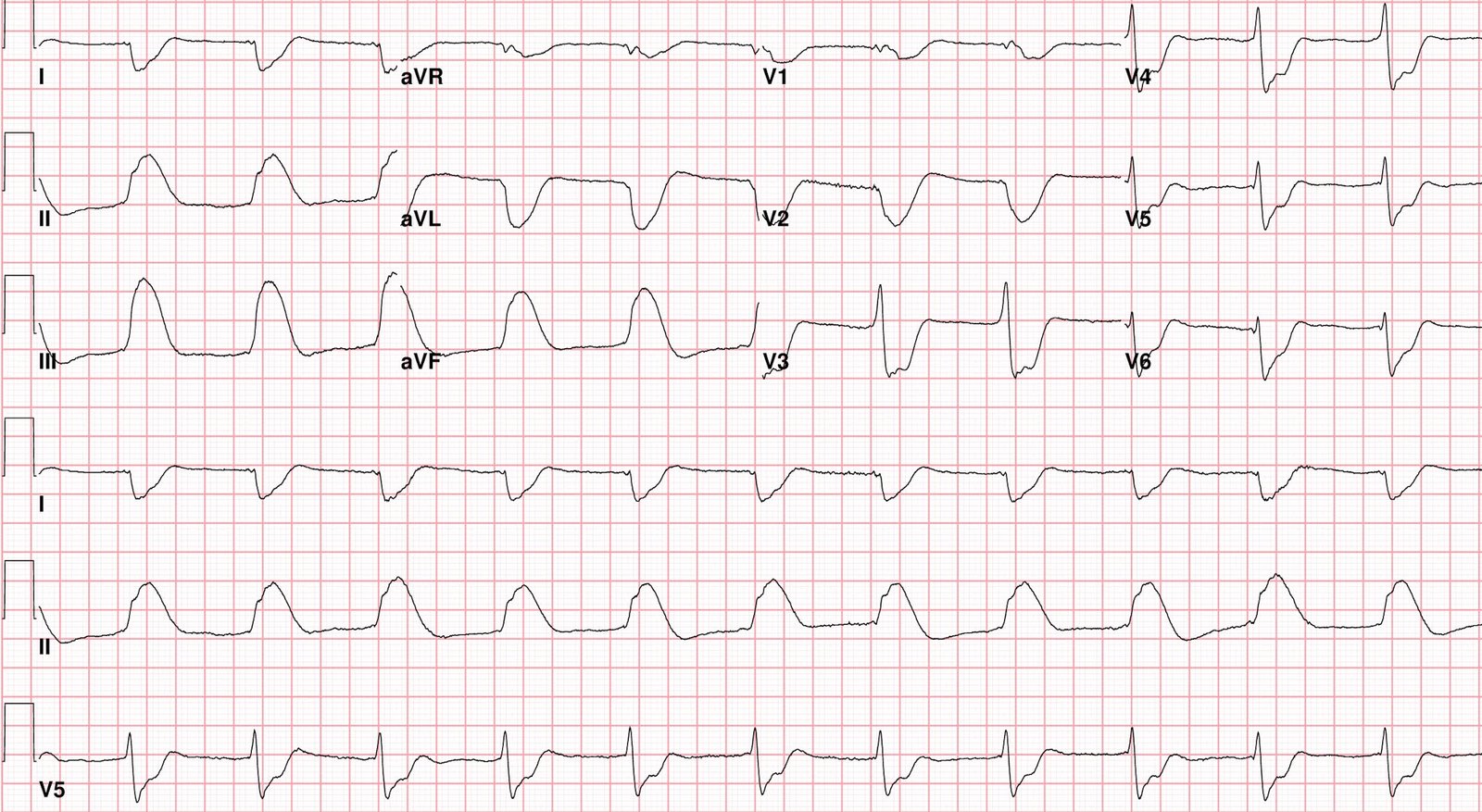
- Most impressive in Figure-1 — is the excessive ST depression in the chest leads that is maximal in leads V2,V3,V4. This is strongly suggestive of posterior OMI.
- Retrograde P waves in the inferior leads distort the ST segments in leads II,III,aVF (YELLOW arrows in these leads). To compensate for this — I’ve drawn RED arcs in these inferior leads to show what the ST segments would have looked like if there was no retrograde conduction (ie, inferior lead ST segments would be coved, elevated and look hyperacute).
- In association with disproportionate ST depression in high-lateral leads I,aVL (ie, reciprocal ST-T wave changes) — these hyperacute inferior lead changes serve to confirm the limb lead impression of inferior OMI.
- As per Dr. Smith — this ECG evidence of infero-postero OMI in association with AIVR strongly suggests a reperfusion rhythm as the reason for QRS widening in today’s case.
= = =
Figure-1: I’ve labeled today’s ECG.
= = =
More on AIVR …
AIVR generally occurs in one of the following Clinical Settings: i) As a rhythm during cardiac arrest; ii) In the monitoring phase of acute MI (especially in association with inferior MI); — or, iii) As a reperfusion arrhythmia (following thrombolysis, acute angioplasty, or spontaneous reperfusion). It may also occur in patients with underlying coronary disease, cardiomyopathy, and/or with digoxin toxicity.
- AIVR is often an “escape rhythm” — in that it arises because both the SA and AV nodes are not normally functioning. IF treatment is needed (which could occur if loss of the atrial “kick” results in hypotension) — Atropine is the drug of choice (in hope of speeding up the SA node enough to resume its pacemaking function). AIVR should not be shocked nor treated with antiarrhythmic medication such as Amiodarone/Procainamide — since doing so might result in asystole.
- NOTE #1: On rare occasions — AIVR may occur intermittently in otherwise healthy subjects without underlying heart disease. If such subjects are asymptomatic during episodes — then no treatment is needed.
- NOTE #2: When AIVR occurs in otherwise healthy individuals — it is usually due to an increase in vagal tone that is able to exert its influence on the ectopic ventricular focus (this is especially true when AIVR is seen in athletes).
- NOTE #3: When AIVR is seen as a reperfusion arrhythmia in association with acute or recent MI — it is usually transient and asymptomatic, and not in need of treatment.
BOTTOM Line: The importance of distinguishing between AIVR (ie, “slow VT” ) — vs “fast VT” (heart rate generally ≥130/minute) — is that active treatment of AIVR is usually not needed (provided the patient is hemodynamically stable and tolerating the rhythm) — whereas the opposite is true for sustained VT.
- “Benign neglect” ( = observation) is usually the most prudent approach for AIVR (in addition to ensuring adequate oxygenation, normal electrolytes, etc.) — since this form of ventricular rhythm is far less likely to deteriorate to fast VT/VFib.
- To Remember: An intermediate ( = “gray zone” ) rate range exists, in which the ventricular rhythm is in between ~110-130/minute — for which clinical judgment is needed (depending on the scenario) for determining whether active treatment of the ventricular rhythm is (or is not) likely to be needed.
Finally — For readers interested in serial laddergram illustrations of a complex AIVR rhythm — Check out My Comment at the bottom of the page in the October 3, 2023 post.
= = =
= = =