Submitted and written by Rachel Plate M.D., with some edits by Smith and Meyers
A man in his 60s with history of type 2
diabetes, obesity, obstructive sleep apnea requiring nightly CPAP, and hypertension
presented for evaluation following a witnessed syncopal episode at home. The
patient noted this occurred after standing and he did have prodromal symptoms
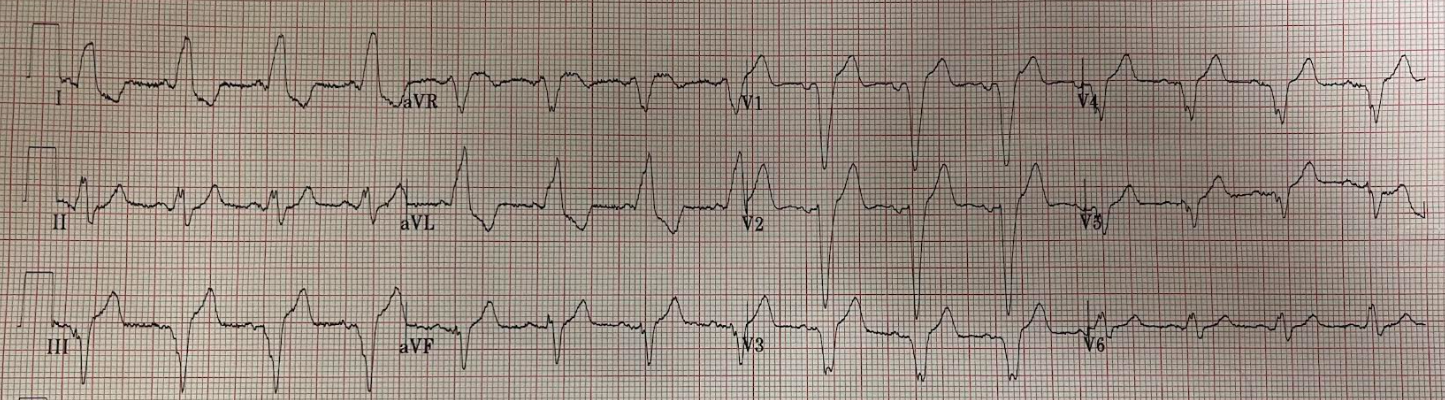
including lightheadedness. EKG was obtained and shown below.
 |
| What do you think? |
The ECG shows sinus rhythm a bifascicular block,
both a right bundle branch block and a left anterior fascicular block. The P waves are hard to discern with the artifact present, but I believe there is also likely a prolonged PR interval, also called first-degree AV block (when this is present with bifascicular block, some people use the misnomer “trifascicular block”).
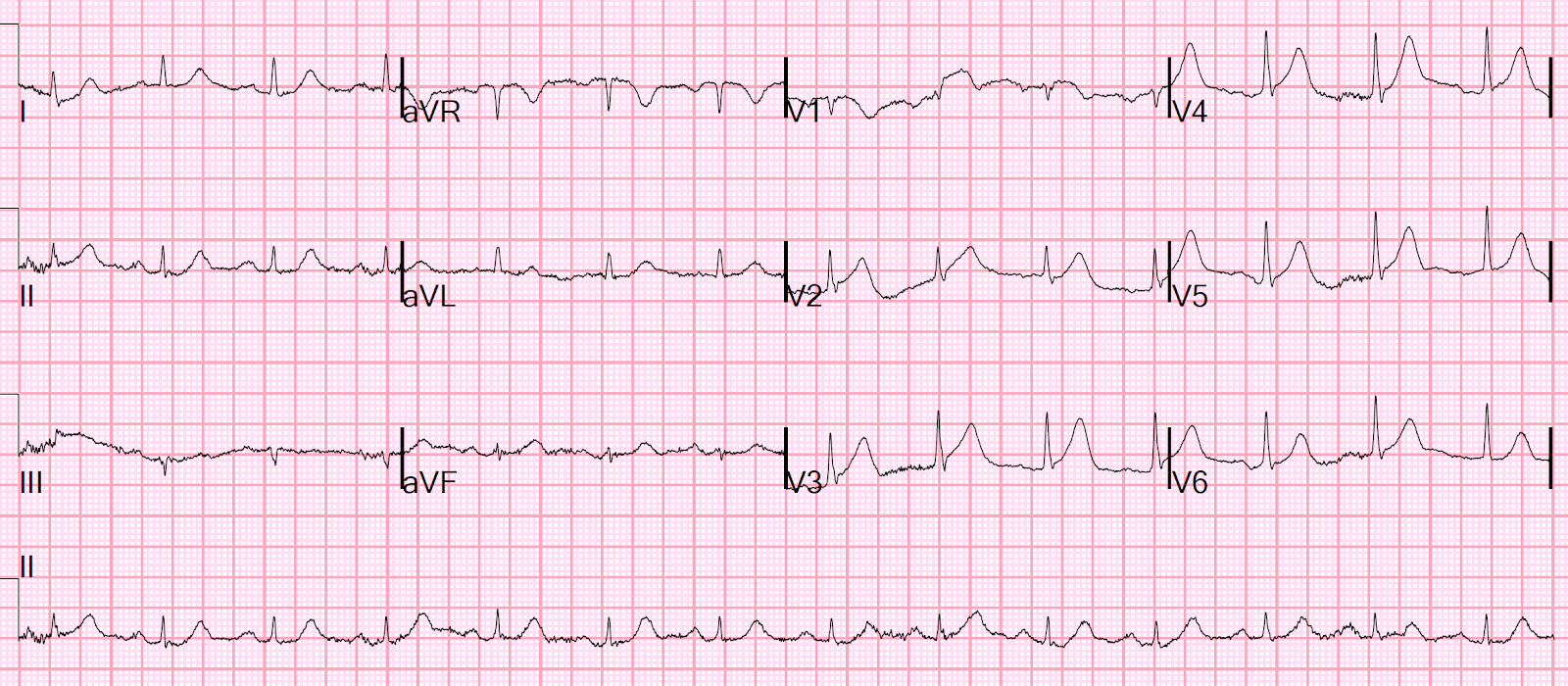
There was an old ECG on file from years ago:
 |
| Only LAFB here, no RBBB. So the RBBB is new compared to prior. |
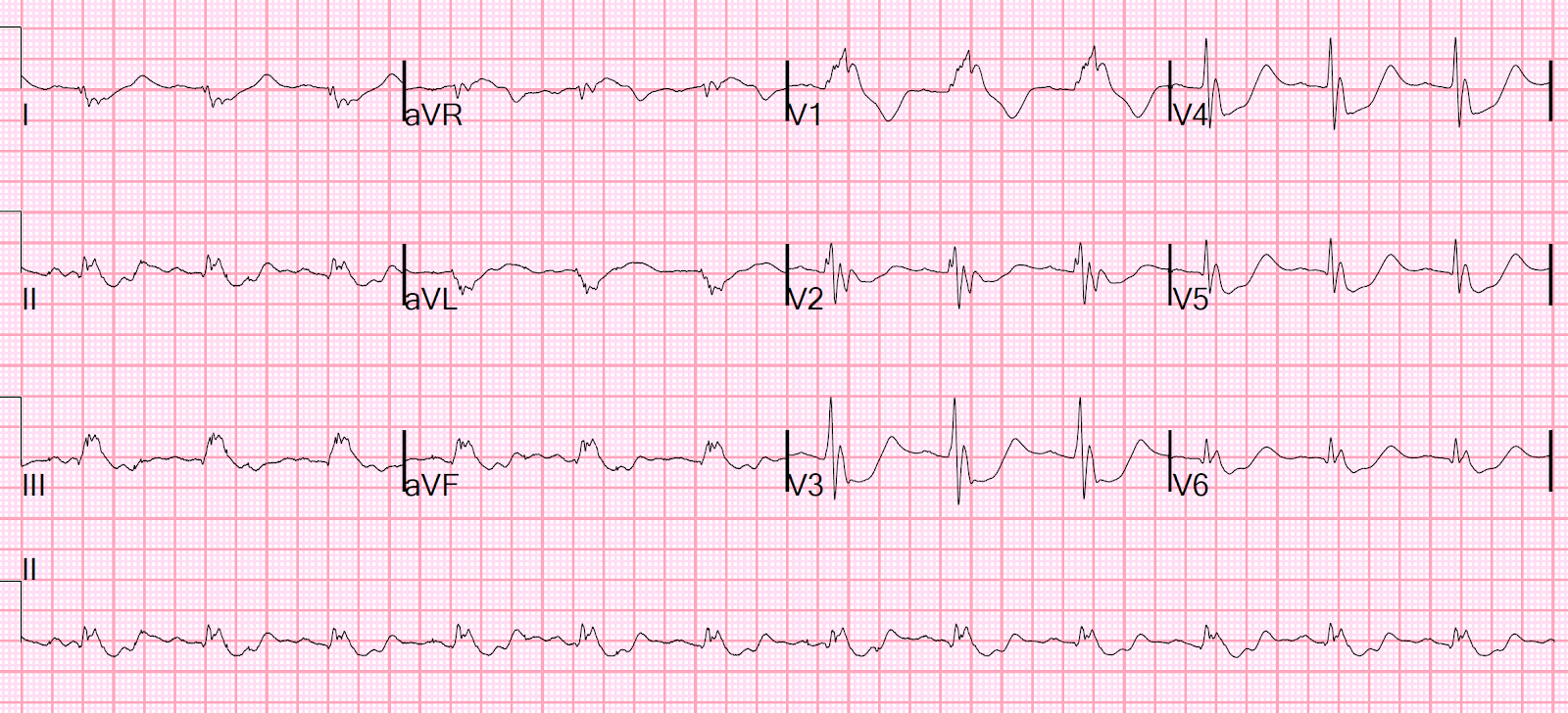
Two days later he had another syncopal episode at home, woke up on the floor, and again called 911. This time his ventricular rate was notably in the 30s in the ambulance. The
following EKG was obtained.
The distinction between high grade second degree AV block and third degree (complete) heart block is not very important, as this patient has already demonstrated high risk to deteriorate into fatal bradyarrhythmia.
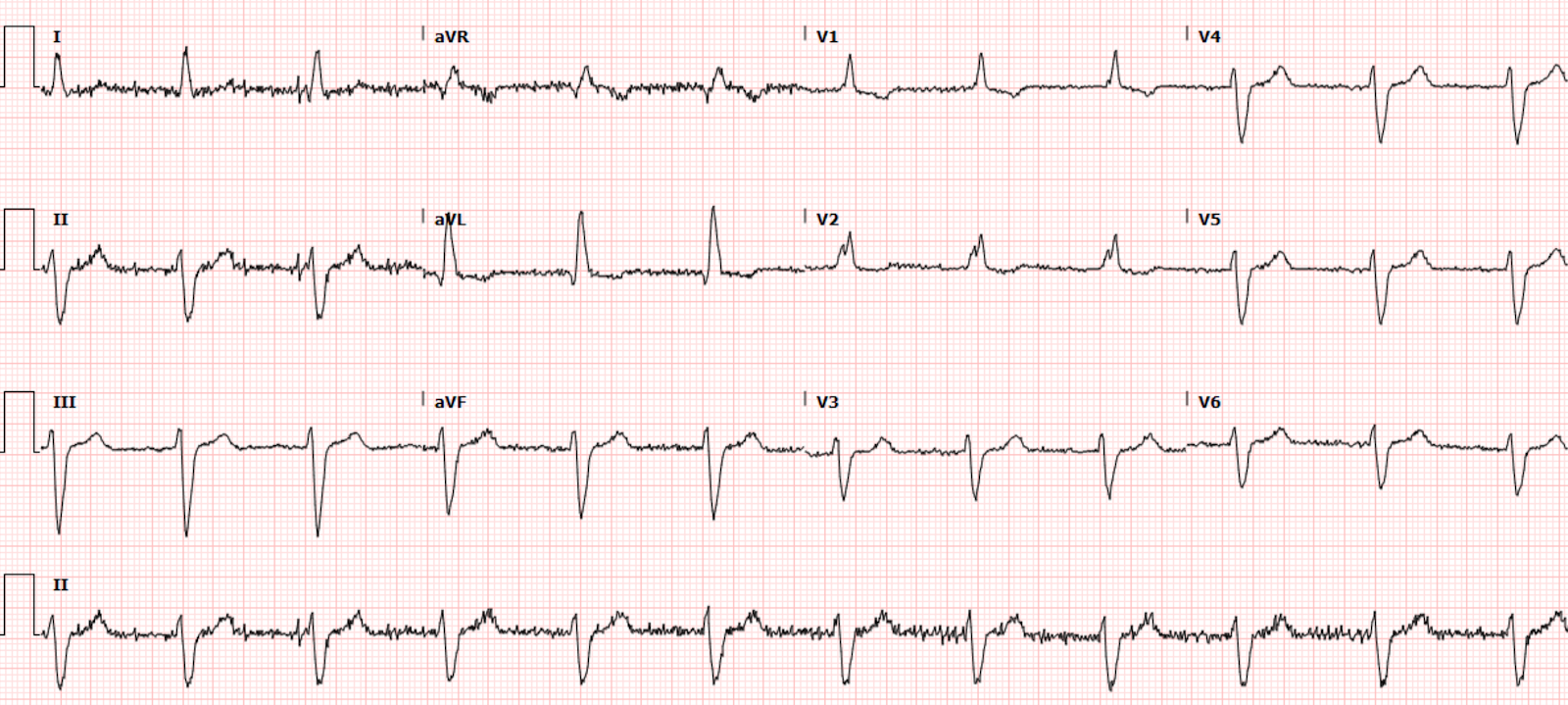
While the team was preparing atropine and
transcutaneous pacing, the patient’s ventricular rate spontaneously improved.
This EKG was obtained.
Now, we again note a bifascicular block with
1st degree AV block.
However, an hour later, he subsequently had
another syncopal episode associated with asystole lasting 30
seconds after which he spontaneously reverted to complete heart block.
No ECG or monitor strip was obtained during asystole.
Following, cardiology was able to place a
temporary pacing wire and then a permanent pacemaker later the same morning.
The patient was discharged after an uncomplicated hospital course on hospital
day 2.
Learning
Points
Syncope +
new onset bifascicular block + historical concern for cardiac syncope
warrants consideration that the cause of syncope could have been transient further deterioration of the conduction system, including complete heart block and/or asystole.
Such a high-risk syncope patient should be recognized and admitted on telemetry for observation of further episodes and consideration of a permanent pacemaker. Deadly bradydysrhythmias due to conduction system failure is an especially preventable cause of death with the availability of the pacemaker.
I teach the “WOBBLER” mnemonic to my learners for syncope ECG evaluation. I believe this mnemonic is attributed to Cliff Reid at Resus.me (https://resus.me/wobbler/). I find this to be an excellent way to keep the important ECG syncope findings in mind, and systematically search each of the many many syncope/lightheadedness/palpitations ECGs I see each shift.
WOBBLER stands for:
WPW
Obstructed AV pathway (meaning AV blocks)
Brugada
Bifascicular block
LVH (including HOCM and other entities with LVH such as aortic stenosis)
Epsilon wave (ARVC)
Repolarization (both short and long QT)
Dr Smith wrote this fantastic post back in 2015 which I highly recommend for a review of the entire approach to ED syncope:
Emergency Department Syncope Workup: After H and P, ECG is the Only Test Required for Every Patient…..
In this post he describes many high risk features in syncope on the ECG, including:
Long QT (at least 480-500 msec)
Brugada morphology
RV dysplasia (including epsilon wave)
WPW
HOCM
Non-sinus rhythm
SVT or VT (obviously)
AV blocks
Sinus pauses of 2 seconds or more
RBBB with hemiblock (bifascicular block)
LBBB
Any acute ischemia
Pathologic Q waves
LVH or RVH
Click here for 2 more trifascicular block cases:
https://drsmithsecgblog.com/search/label/Trifascicular%20block