Sent by anonymous, written by Pendell Meyers
A man in his 70s presented with acute chest pain, shortness of breath, nausea, vomiting, and diaphoresis. The pain started approximately 4 hours prior to arrival, and was still active at the time of EMS arrival. Vital signs were within normal limits.
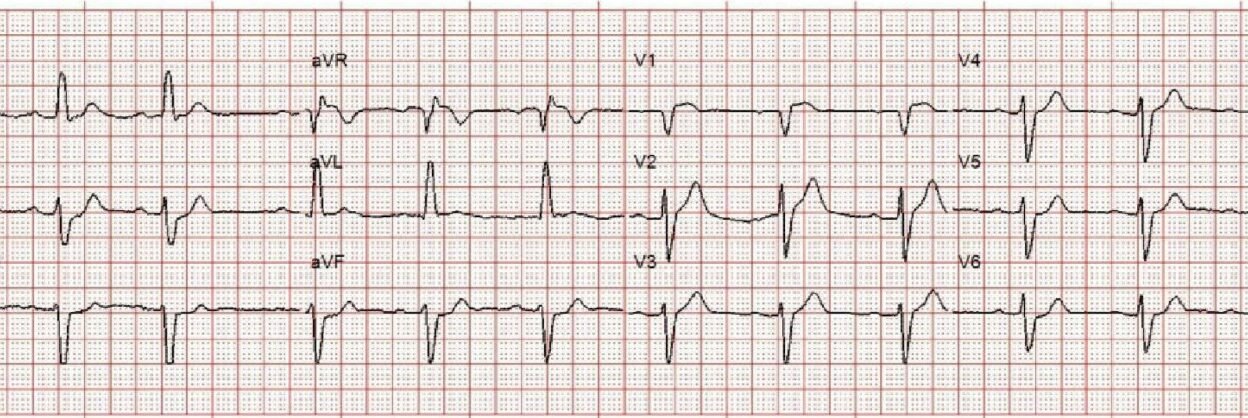
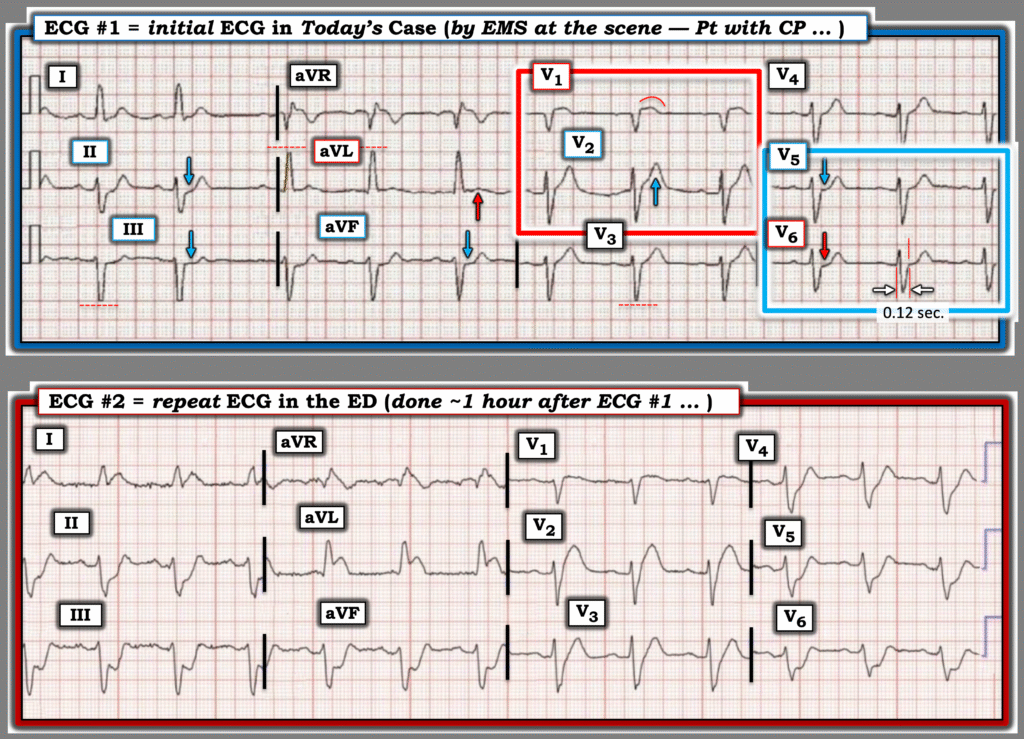
EMS ECG transmitted to ED physician:
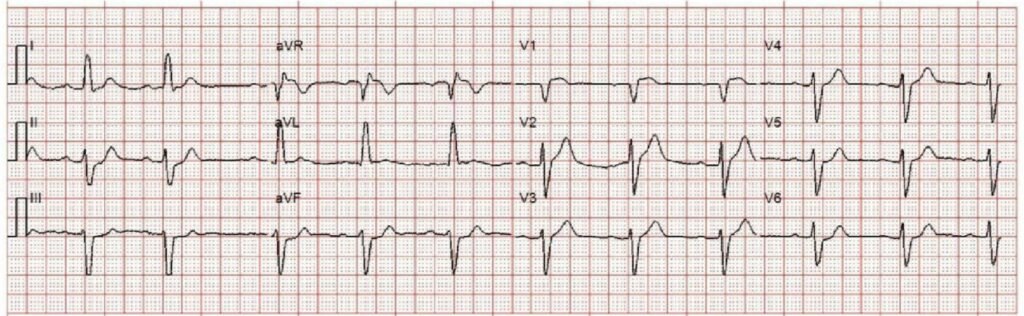
What do you think?
There is sinus rhythm with left anterior fascicular block. There is STE in V1 and V2 which does not meet STEMI criteria. There is precordial swirl pattern LAD OMI, and the suggestion of nearly concordant STE in aVL (there should instead be appropriately discordant STD at baseline in this QRS context). There is concordant reciprocal STD in II, III, and aVF, further confirming the high lateral findings. The LAF is always supplied by the LAD. This ECG is diagnostic for acute LAD occlusion.
____
Smith:
LAFB alone should not have a wide QRS, so this is really intraventricular conduction delay (IVCD, QRS >/= 120 ms) with an LBBB-like morphology and left axis deviation which does look like LAFB. For this IVCD, just like in LBBB, there should be discordant ST/T. As Pendell mentioned, in aVL, the ST is concordant. It is concordant by less than 1 mm, but it should be discordant by approximately 10%, which would be 1 mm. Thus, there is more than 1 mm of RELATIVE ST elevation. And there is concordant reciprocal ST depression in inferior leads.
As for the precordial swirl (see this paper): one might not think there is ST depression in V5-6, as required by precordial swirl, but, again, there should be ST elevation discordant to the wide, negative, S-wave. So there is probably RELATIVE ST depression in V5-6. Our very specific rule for precordial swirl requires a T-wave to S-wave ratio of 0.40 or greater; here it is 7/9 = 0.77. In this case, there is also ischemic ST Elevation in V1 (ST/S > 25%)
____
Thus the ECG is diagnostic of LAD Occlusion, LAD OMI.
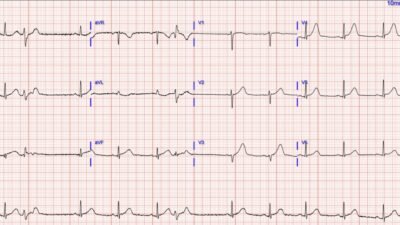
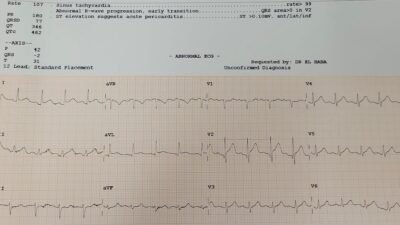
Here is the Queen of Hearts interpretation (she agrees, and notice she sees hyperacute T-wave in V2 and STE in V1, in addition to aVL with reciprocal findings in inferior leads):

New PMcardio for Individuals App 3.0 now includes the latest Queen of Hearts model and AI explainability (blue heatmaps)! Download now for iOS or Android. https://www.powerfulmedical.com/pmcardio-individuals/ It is not yet FDA approved, but is CE approved in the EU.
The ED physician documented “the EMS ECG does not meet criteria for STEMI.”
Around 1 hour later, a repeat ECG was performed in the ED:
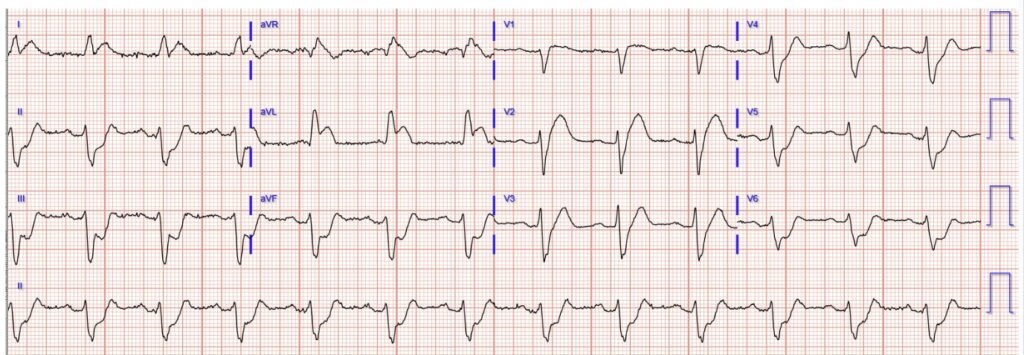
Hopefully an easy one for everyone.

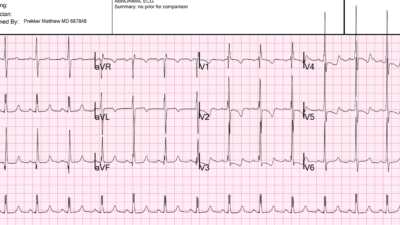
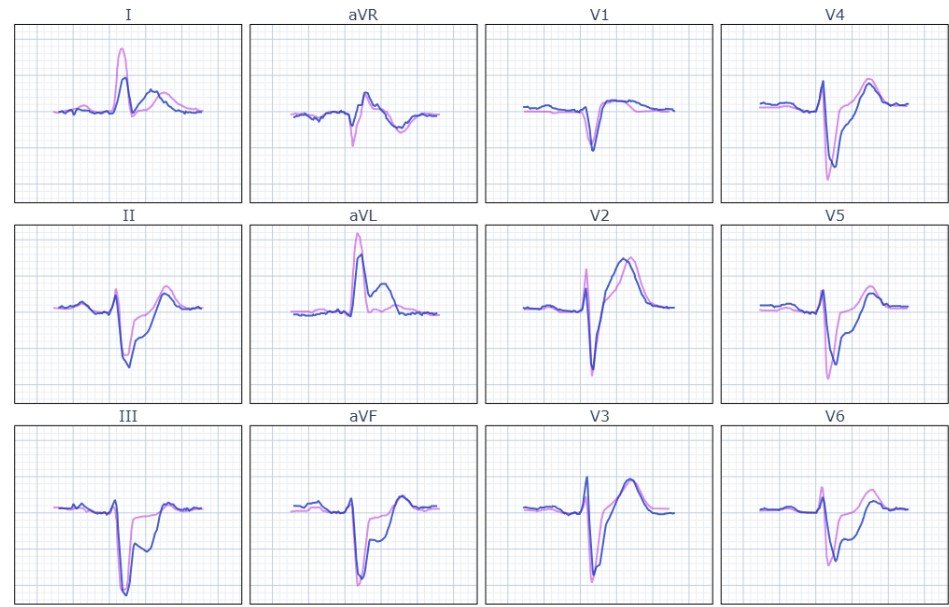
For interest, here are the two ECGs superimposed on each other, both equally diagnostic.
At this point, code STEMI was called.
Angiogram showed culprit total occlusion of the proximal LAD.
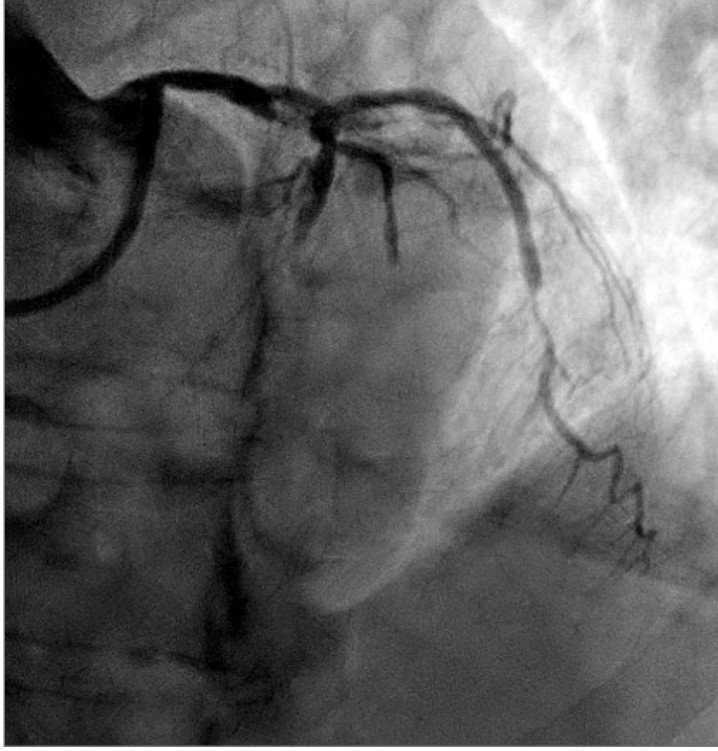

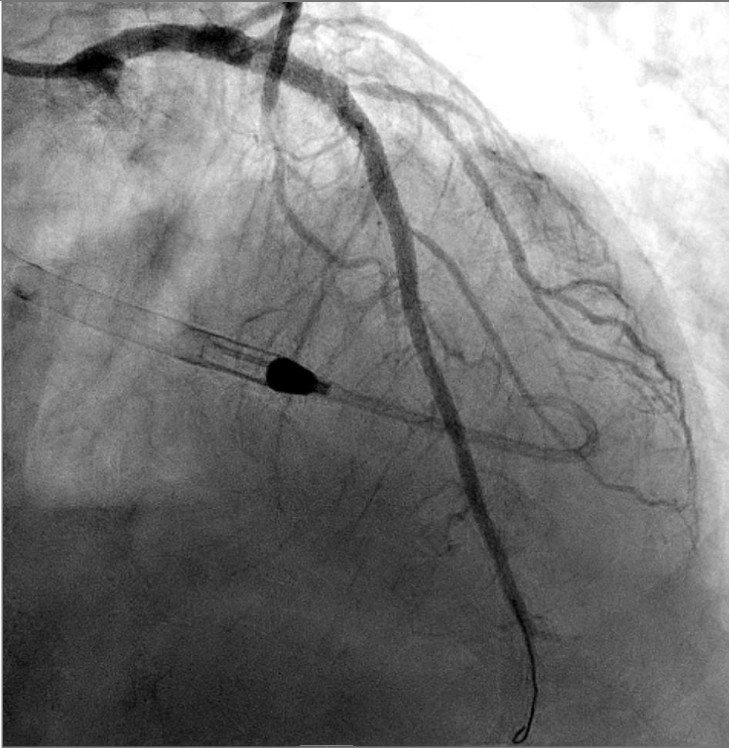
Despite PCI, cardiogenic shock progressed on the cath lab table. Impella was used, and the patient was intubated for progressive respiratory failure.
Ultimately he died.
Although his mortality risk was high even before arrival, there was an hour of misdiagnosis. One hour delay can results in loss of up to 50% of the mortality benefit of reperfusion. It is possible he could have had a better outcome if he had reperfusion 1 hour earlier.
Thought that STEMI criteria was good at finding complete proximal LAD occlusions? Think again:
Meyers HP, Sharkey SW, Herman R, de Alencar JN, Shroff GR, Frick WH, Smith SW. Failure of standard contemporary ST-elevation myocardial infarction electrocardiogram criteria to reliably identify acute coronary occlusion of the left anterior descending coronary artery. EHJ: ACC (2025) 00,1-9. https://doi.org/10.1093/ehjacc/zuaf037
Here are many more examples of precordial swirl
= = =
======================================
MY Comment, by KEN GRAUER, MD (10/27/2025):
Today’s case is unfortunate in that failure to recognize the acute OMI from today’s initial ECG resulted in a 1-hour delay in performing cardiac cath with PCI. As emphasized by Dr. Meyers — we have no idea if earlier recognition of acute coronary occlusion would have made a difference in the ultimate outcome of this high-risk case. That said — retrospective review of the clues that were present in ECG #1 will hopefully provide insight for the interpretation of future cases.
===
The Initial ECG: Some General and Advanced Points
For clarity and ease of comparison in Figure-1 — I’ve put together the 2 ECGs in today’s case. My thoughts below highlight some additional points to those discussed above by Dr. Meyers:
- Looking at ECG #1 systematically — I favor starting with the rhythm. Although we lack a long lead rhythm strip — the overall rhythm looks to be fairly regular, albeit with slight variation in the R-R interval ( = sinus arrhythmia).
- Regarding Intervals — I measure the PR interval = 0.21 second, which I consider as still “within normal” for an older adult. But the QRS complex is wide (clearly 0.12 second in duration — as shown in lead V6 in Figure-1). Moreover, the QRS “looks” to be wide.
- NOTE #1: In most cases — an isolated LAHB (Left Anterior HemiBlock) does not widen the QRS by more 0.01-0.02 second, such that true QRS widening will usually not be seen as a result of LAHB alone. Strictly speaking — I favor classification of QRS morphology and QRS duration in ECG #1 as IVCD (IntraVentricular Conduction Delay), here with LAD (Left Axis Deviation).
- Advanced Points (Beyond-the-Core): Without use of a systematic approach — it’s easy to overlook QRS widening in this initial ECG. For me — appreciation of IVCD in this initial tracing was of more than academic significance — as it clued-me-in to additional reasons why the ST-T waves in leads I and aVL are suspicious in this ECG #1 (ie, This QRS widening with predominant positivity in leads I,aVL resembles lbbb conduction — which is normally associated with ST-T wave depression, but which is missing in these leads).
- = = =
- NOTE #2: For “My Take” on the importance of using a Systematic Approach to 12-lead ECG interpretation — See My Comment in the October 17, 2022 post.
- NOTE #3: For review of “My Take” regarding a user-friendly way to diagnose the type of conduction defect in less than 5 seconds — CLICK HERE for my ECG Video on this subject.
- NOTE #4: It’s important to be aware that QRS amplitudes are truncated in ECG #1 because this is a pre-hospital tracing (and at least in the U.S. — many pre-hospital systems automatically truncate positive and negative QRS deflections at ~10 mm). From comparison of QRS amplitudes in the non-truncated ED ECG #2 — we can see that this pre-hospital truncation effect did not make much of a difference in today’s initial tracing — BUT — Awareness of the phenomenon of automatic QRS truncation of pre-hospital ECGs sometimes can make a huge dfference in our interpretation! (See My Comment in the June 20, 2020 post).
= = =
ECG Findings of Acute OMI:
The presence of IVCD often makes recognition of an acute OMI much more challenging — as it may be harder to predict what non-ischemic ST-T wave changes should look like. As a “Rule of Thumb” — I look for ST-T wave changes that shouldn’t be there.
- In today’s initial ECG — my “eye” was immediately drawn to the 2 leads within the RED rectangle ( = leads V1 and V2).
- Regardless of QRS widening — the ST segment coving and disproportionate amount of ST elevation in lead V1 is clearly abnormal (given the small size of the QRS in this lead).
- I found it interesting that the shape of the ST-T wave in neighboring lead V2 is very different from the ST coving in lead V1 — but as per Dr. Meyers, the disproportionate “bulkiness” of the ST-T wave in lead V2 from this 70s man with new CP (Chest Pain) qualifes as a hyperacute T wave.
- I found it harder to assess ST-T wave appearance in neighboring leads V3,V4 — but there clearly is ST segment straightening in V5,V6, with slight ST depression in lead V6 (within the BLUE rectangle).
- As I highight in My Comment at the bottom of the page in the October 15, 2022 post — the diagnosis of Precordial Swirl (due to a very proximal LAD occlusion) is immediately suggested in ECG #1 by: i) ST elevation in leads V1,V2 — with the ST elevation in lead V1 manifesting a different shape than expected; — and, ii) ST depression with a flattened shape in lead V6 (and often also in lead V5).
- In support of a proximal LAD occlusion in ECG #1 — is the finding of i) Reciprocal ST depression in the inferior leads; — and, ii) The unexpected ST-T wave positivity in leads I,aVL that I describe above in this patient with IVCD.
= = =
Figure-1: Comparison between the 2 ECGs in today’s case.
= = =
What We Learn from the Repeat ECG in the ED:
Extensive anterior infarction is obvious in ECG #2. That said — there is more to be learned from careful lead-by-lead comparison of the 2 tracings in Figure-1.
- The BEST way to improve your ability to recognize subtle acute ECG findings — is to go back after the diagnosis becomes obvious to Take Another LOOK at the initial ECG when findings were much more subtle.
- The concern that I had about the atypical ST-T wave appearance in leads I,aVL of ECG #1 (given QRS widening with lbbb-like morphology in these leads) — is validated by the obvious hyperacuity and ST elevation seen in leads I and aVL in ECG #2.
- The subtle ST flattening and depression in the inferior leads of ECG #1 — was clearly a harbinger for the marked ST depression that followed in ECG #2.
- DeWinter-like T waves have now developed in the mid-chest leads of ECG #2 — with marked ST depression in leads V5,V6 (this extreme lateral chest lead ST depression being a reciprocal change from the very proximal LAD occlusion).
- Finally — Finding a prior ECG on today’s patient would have been especially insightful in our retrospective review (especially regarding whether the QRS was wide or narrow on this patient’s baseline tracing — vs new QRS widening being another early sign of acute ischemia).
= = =
= = =