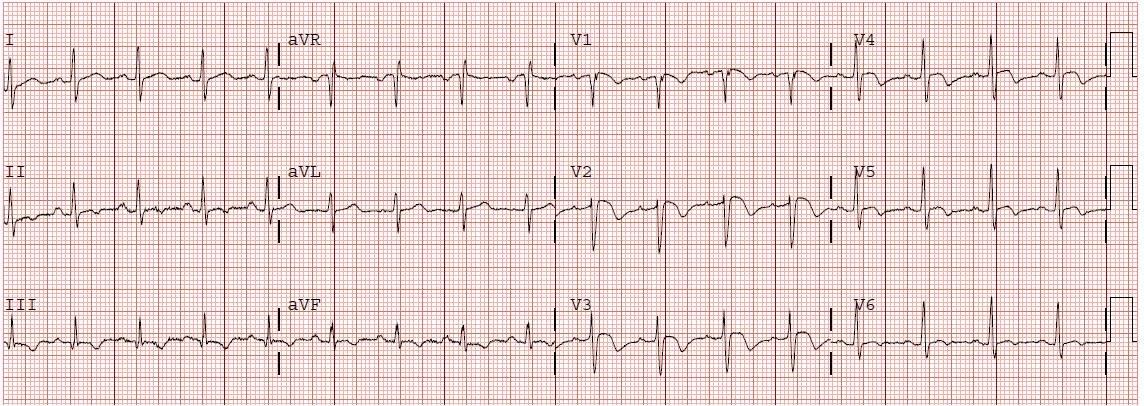
A 32 year old male presented with a 4 day history of dyspnea, cough, palpitations, and chest pain. He had an ECG done immediately (shown above). This showed anterior T wave inversions, a QTc of 431, and also T inversion in lead III. There is sinus tachycardia and an S1Q3T3. This is all highly suspicous for pulmonary embolism.
.
Oxygen saturation was 95%, there were some end expiratory wheezes. D dimer was 3000. A CT pulmonary angio confirmed large central PE.
.
Kosuge et al. (Am J Cardiol 2007;99:817-821) compared patients with ACS and PE who had precordial T wave inversions in V1-V4. They found that in this select population, negative T waves in lead III were observed in only 15% of patient with ACS, compared with 88% of patients with Acute PE.
.
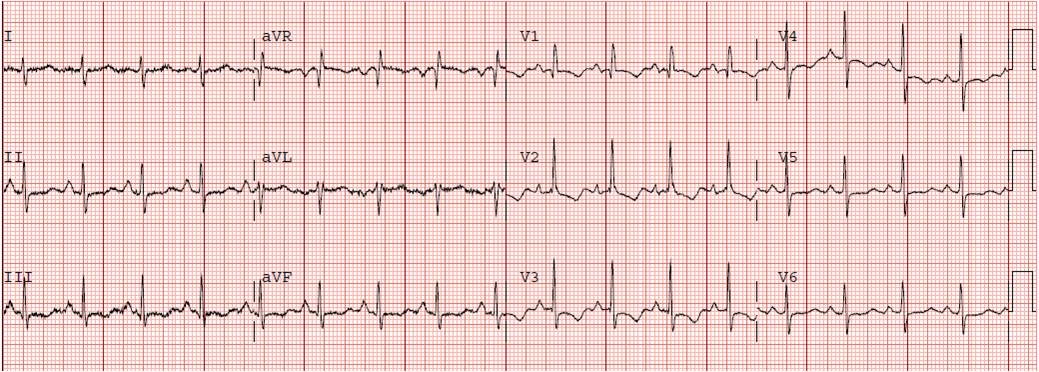
It is tempting to diagnose Wellens’ syndrome with anterior T wave inversions, but Wellens’ T waves simply look different, should have a longer QTc, generally don’t extend out to V6, and, most importantly, don’t have T inversion in lead III.
.
Of course the clinical scenario is most important.
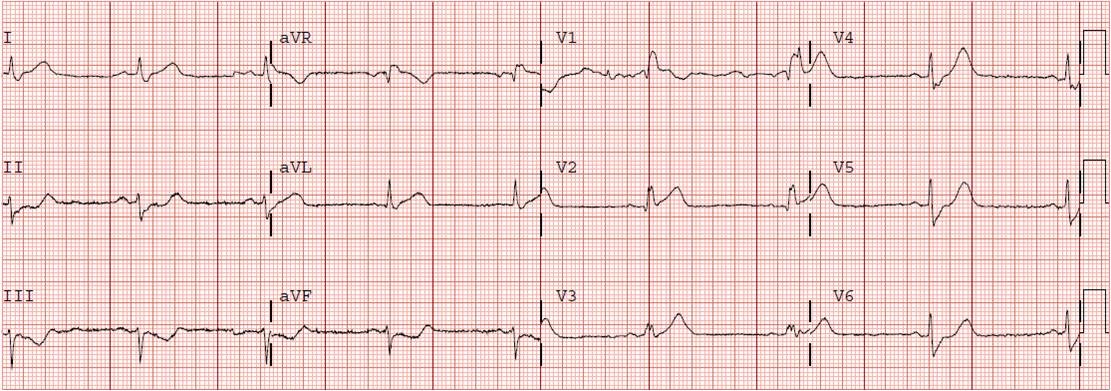
This morphology can be seen in any acute right heart strain, including asthma, see here:
https://drsmithsecgblog.com/2011/04/is-it-pulmonary-embolism.html