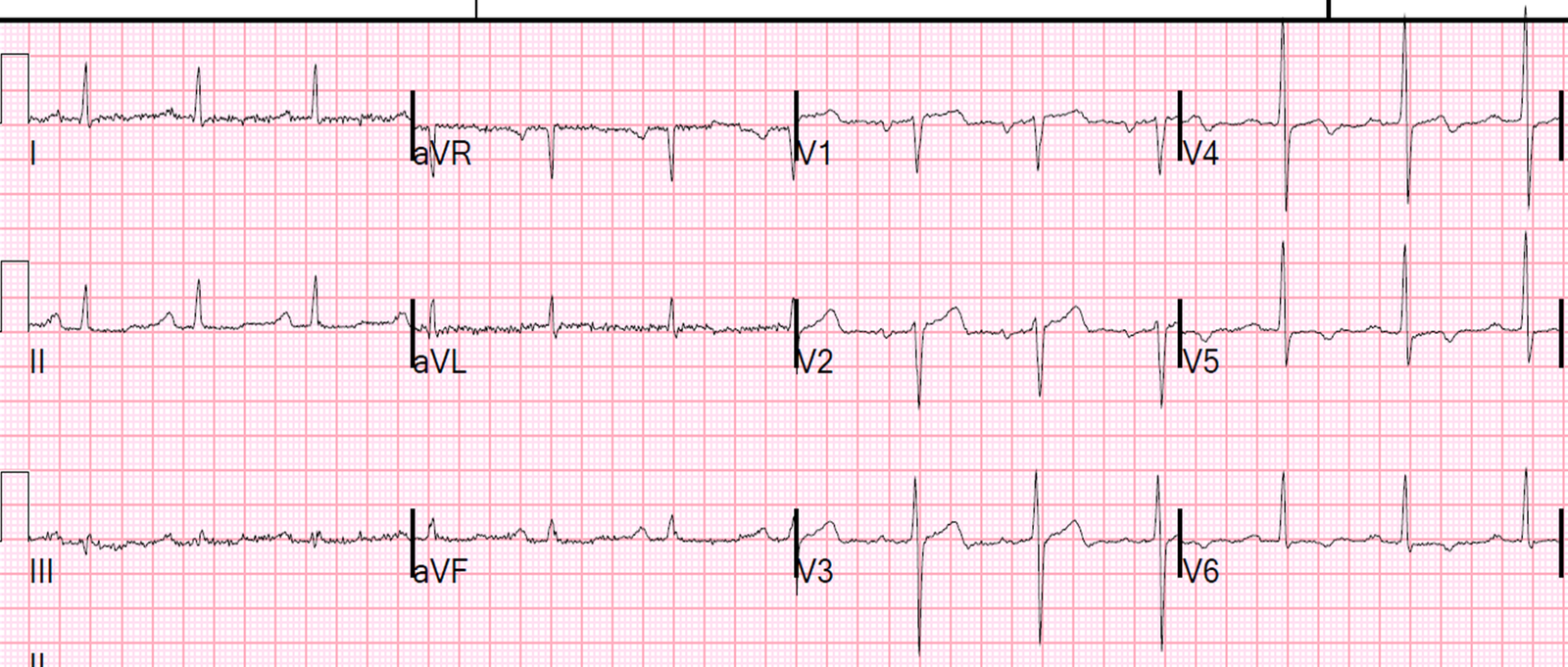
A 56 year old diabetic male with
family history of young MI and prior CAD with stent was awoken by typical
substernal chest pain. He had this ECG recorded.
Here are precordial leads enlarged:
Strictly speaking, the formula
should not be used because there is terminal QRS distortion, which by itself
makes STEMI almost certain: “Emergence of the J point ≥50% of the R wave
in leads with qR configuration, or disappearance of the S wave in leads
with an Rs configuration)”
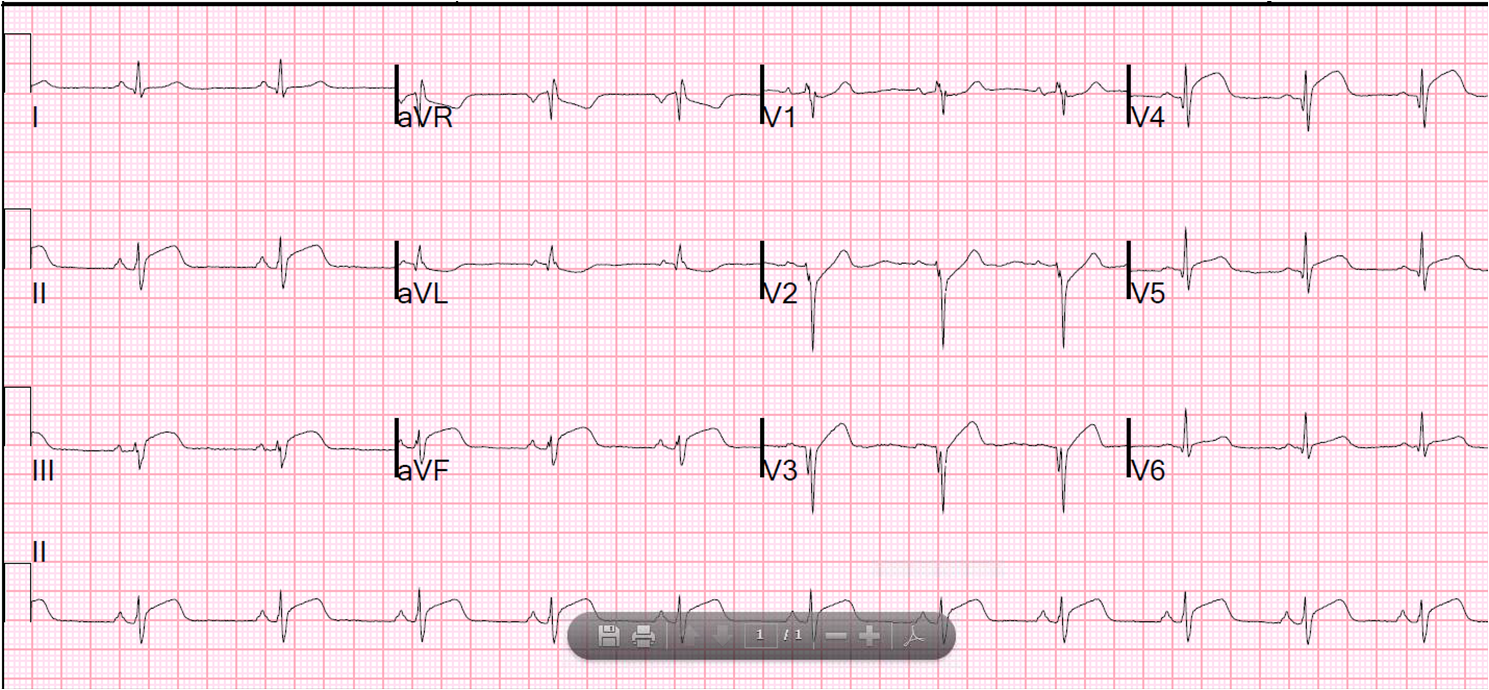
They gave him nitro and morphine and
his pain resolved. The ED ECG is below, 27 minutes after the prehospital ECG, and few minutes after resolution of pain.
 |
||
| Pretty much normal |
The ED physician activated the cath
lab and the cardiologists were in disagreement but took the patient to the cath
lab.
He had a 95% thrombotic LAD that was
stented. Troponin I peaked at 2.4 ng/ml.
Here is his 30 hour ECG:
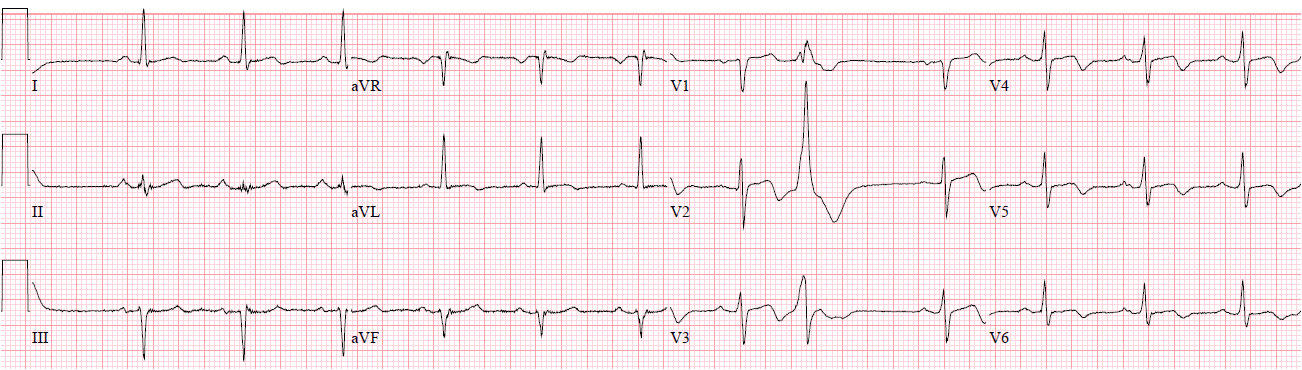 |
| Sinus with PVC. Classic Wellens’ syndrome ECG |
These things are clear:
1. During the prehospital ECG, the
LAD was occluded, or flow was limited to the point where there was ST elevation
(injury due to subepicardial, transmural, ischemia)
2. The pain resolved (a key
criterion for Wellens’)
3. The repeat ECG was normal
4. The artery had clearly reperfused
and had adequate flow to the anterior wall (another key criterion for Wellens’)
5. The patient needed an angiogram
and PCI at some point
6. The next day ECG was identical to
Wellens’ ECG
This is a great demonstration of
something I have promoted for years, but without proof:
That Wellens’ syncdrome is the
result of the aftermath of spontaneously reperfused LAD occlusion that went
unrecorded during the episode of pain.
This idea is supported by these
characteristics of Wellens’ syndrome:
1. Wellens’ syndrome is always after
resolution of pain
2. There are always preserved
R-waves
3. The LAD is always open, or there
is good colllateral flow
4. The T-wave inversion of Wellens’
is identical to the pattern of T-wave inversion that occurs after therapeutic
reperfusion of LAD occlusion.
See this study by
Doevendans et al.
See this study by
Wehrens et al.
5. Cases like this
Emergent Cath Lab Activation
Questions
1. Should the cath lab be emergently
activated for Transient ST Elevation?
2. Should it be activated emergently
for Wellens’ syndrome?
I don’t think there is any
evidence-based answer to these questions. I would argue that Wellens
syndrome is a result of transient ST elevation that was not recorded.
However, the artery is open. Both conditions are very high risk for
re-occlusion.
The standard answer for someone who
had that ST elevation recorded (Question 1), as in this
case, is to go to the cath lab. Here is what can happens if you make the mistake I did and
do not activate the cath lab.
The standard answer for Question
2 would be “No”, but I would argue strongly that it is very high
risk and it requires maximum antiplatelet and antithrombotic therapy and continuous
12-lead ST segment monitoring. One cannot depend on symptoms to guide
the recording of subsequent ECGs, and I will show an example of this in the
next post.