Written by Magnus Nossen
A 69-year-old woman with a 50-year history of smoking contacted EMS due to sudden onset chest pain. The chest pain was substernal and described as dull with an intensity of 8/10. The pain was accompanied by nausea, vomiting, and profuse sweating. The following ECG was recorded by EMS.
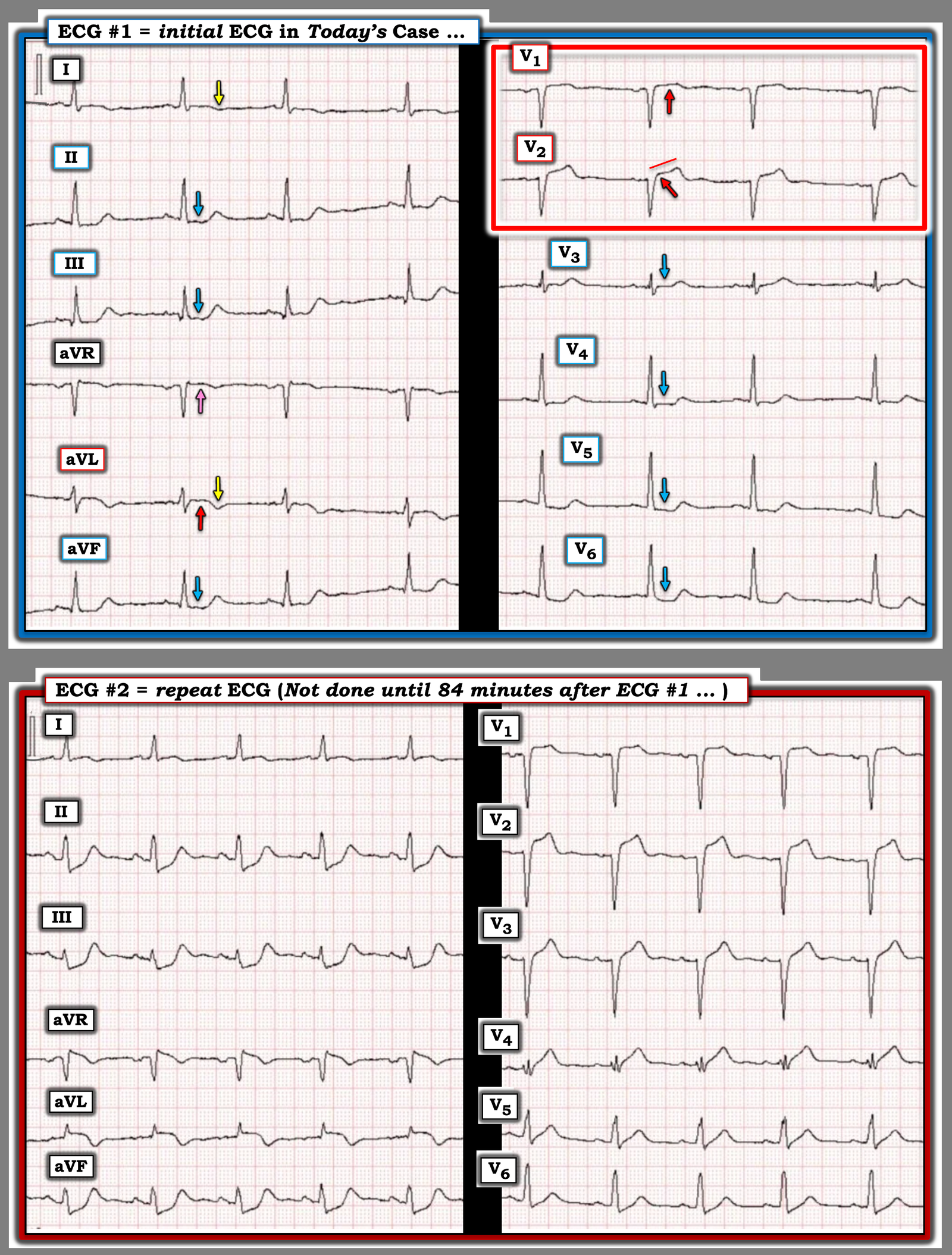
ECG # 1
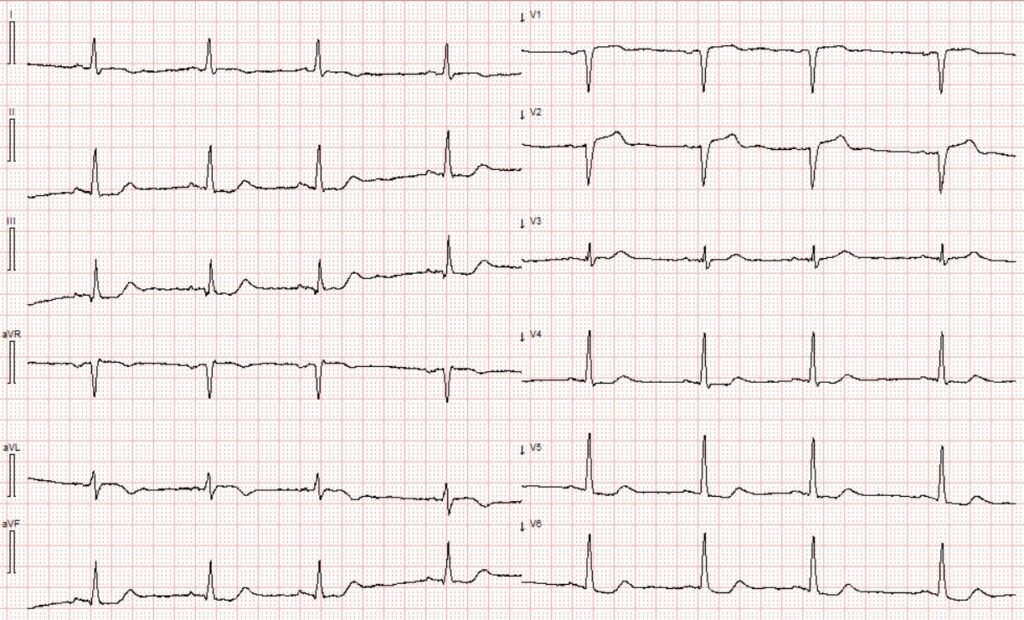
What do you think?
The described clinical scenario in today’s case is textbook for ACS. Based solely on pretest probability and symptoms, cath lab activation is warranted if symptoms persist — and one can make an argument that this patient should go to the cath lab regardless of what the ECG shows.
The ECG was transferred from the ambulance to the local ED where it was interpreted as not showing any significant ST-segment changes. The patient was not considered for STEMI pathway and was transported to the local ED for evaluation.
The ECG shows Precordial Swirl pattern with minimal ST-elevation in the right precordial leads and ST-depression in V4–V6. Most striking perhaps, are the reciprocal inferior ST-depressions with a slight upward-convex ST-segment in aVL. This ECG is diagnostic of LAD occlusion. Unsurprisingly, this was missed.
Smith: The ECG ALSO manifests South Africa Flag sign. There is STE in V2, aVL and I, with reciprocal inferior ST depression.
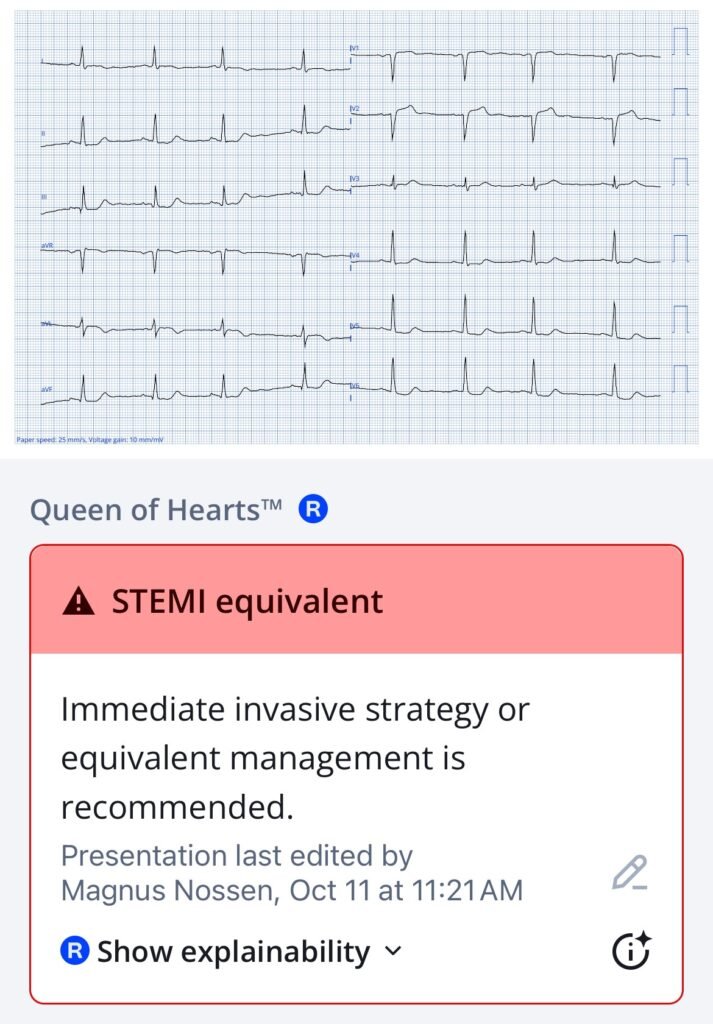
Here is the interpretation of the PMCardio Queen of Hearts AI Model
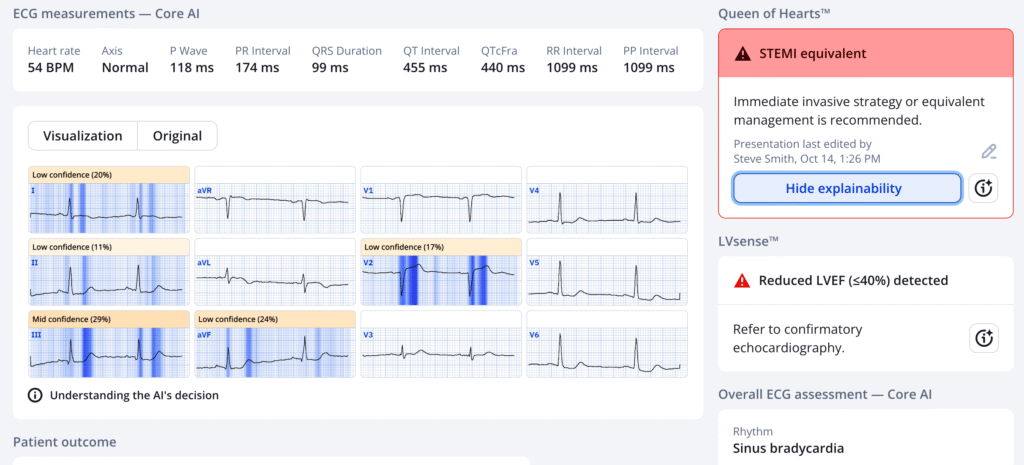
Interestingly, she sees only South Africa Flag sign and NOT the precordial swirl.
New PMcardio for Individuals App 3.0 now includes the latest Queen of Hearts model and AI explainability (blue heatmaps)! Download now for iOS or Android. https://www.powerfulmedical.com/pmcardio-individuals/ It is not yet FDA approved, but is CE approved in the EU.
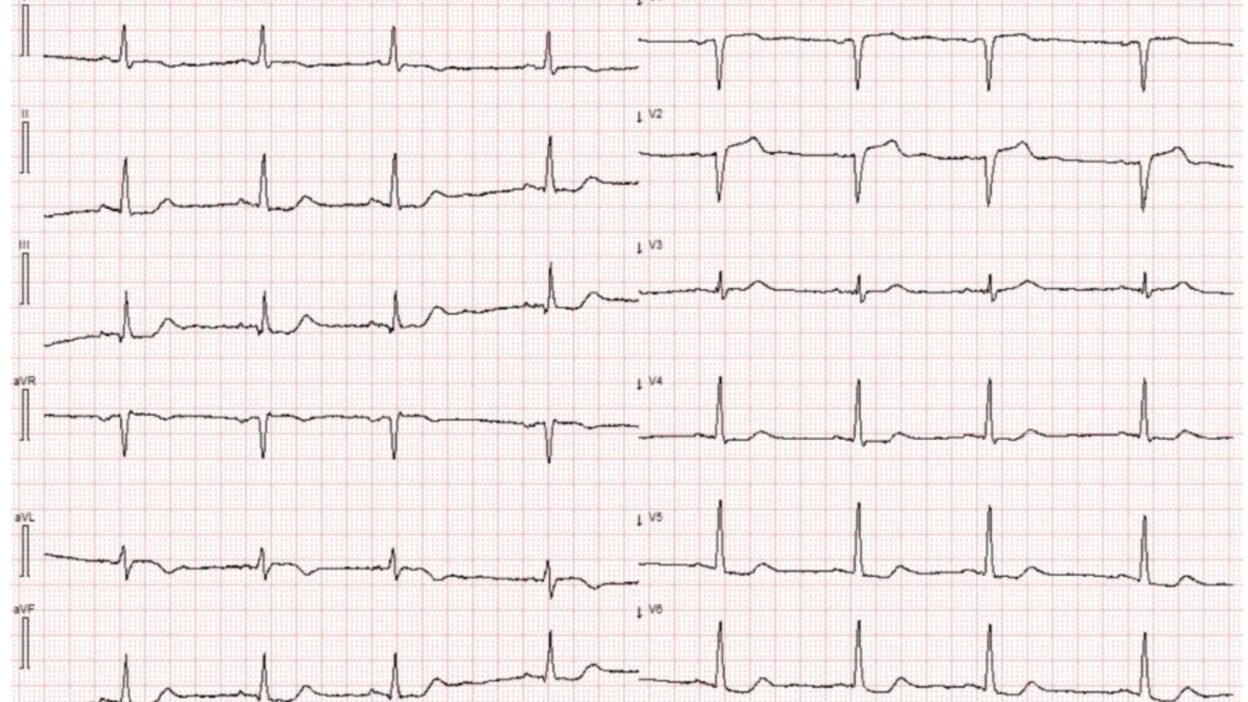
Case continued: Only after the initial troponin I returned elevated at 3285 ng/L, was a repeat ECG performed 84 minutes after the initial ECG. This repeat ECG is shown below.
ECG # 2
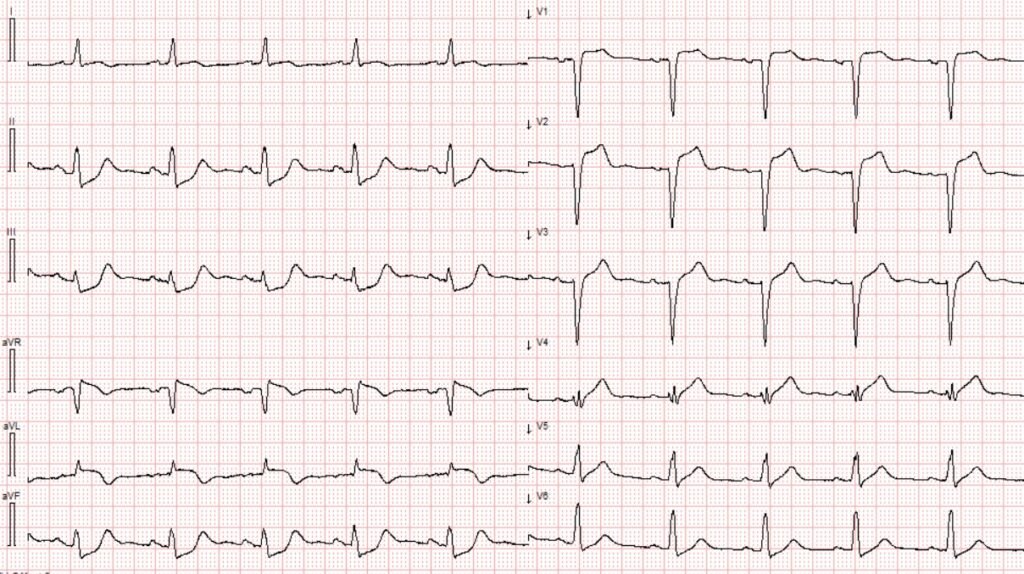
Since the initial ECG, the R waves in V3 have disappeared, with significant R wave loss also noted in leads V4–V6. Inferior ST depression has become even more pronounced. There are hyperacute T waves throughout the precordial leads, along with ST elevation in aVL.
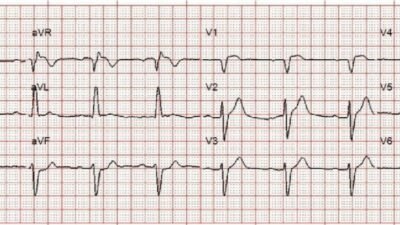
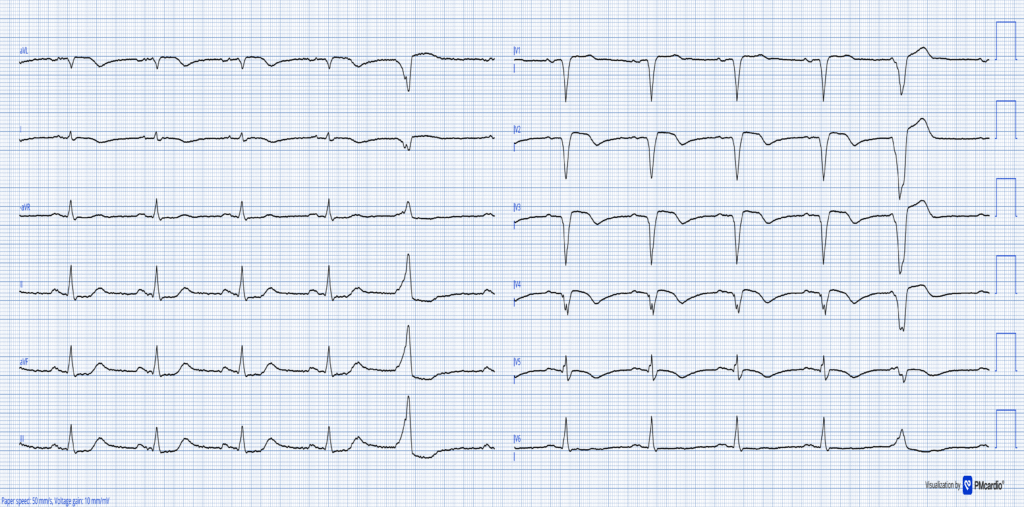
At this point, a bedside echocardiogram was performed, revealing an akinetic anterior wall. The patient was transferred to PCI capable center where a proximal LAD occlusion was opened and stented. During the PCI procedure the patient multiple runs of VT and was shocked back into sinus rhythm. She spent 5 days in the CICU on mechanical circulatory support. Troponin T peaked at 19,767 ng/L a HUGE myocardial infarction. The below ECG was recorded post PCI and shows a completed transmural MI.
Smith: for the same size infarct, troponin I will be 5-10x greater number than troponin T. Therefore, Trop T of 19.767 is extremely high (equivalent to 100,000 – 200,000 of troponin I)
The patient never recovered from the cardiogenic shock died shortly after.
Discussion:
Time is critical for patients with OMI, as even small delays in treatment can be fatal or result in severe morbidity. In this case, the patient experienced an unnecessary and entirely avoidable delay in revascularization, which likely contributed to the development of cardiogenic shock and a tragic outcome. Had the Queen of Hearts AI model been used to interpret the prehospital ECG, the patient could have bypassed the local ED altogether and undergone PCI several hours earlier, potentially leading to a better outcome.
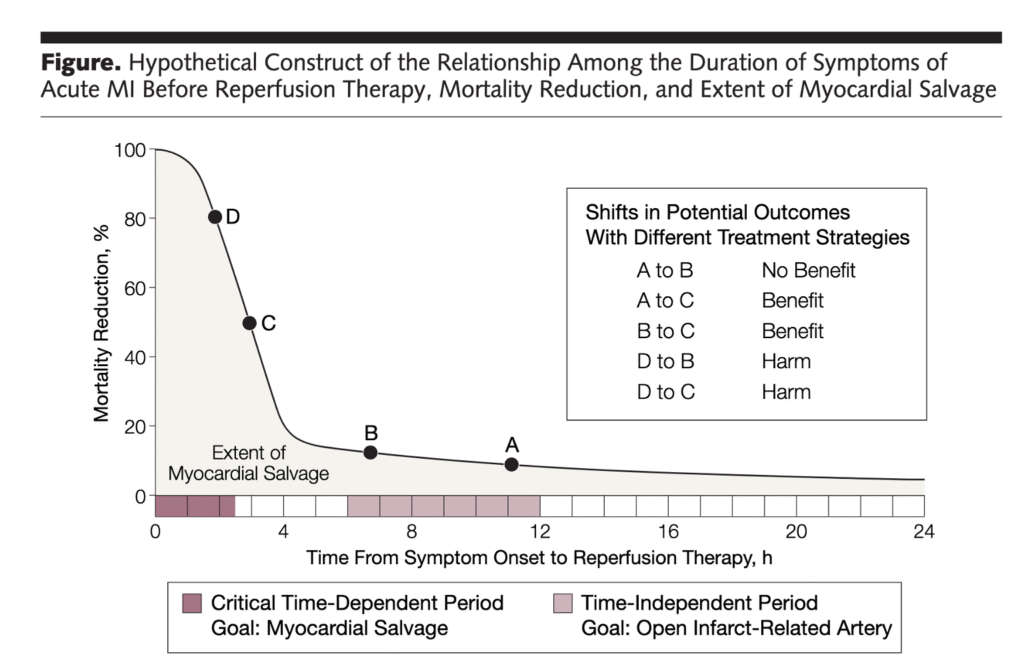
Smith: This graphic shows how a 2 hour delay in reperfusion results in 60% more myocardium infarcted. EVERY MINUTE COUNTS!! This is why we must dispose of the murderous NonSTEMI diagnosis!!
Queen of Hearts with explainability
ECG # 1
Learning points
- Time is critical for patients with acute myocardial infarction. Time to reperfusion is the single most important predictor of outcome in OMI
- The Queen of Hearts would have identified this patient from the prehospital ECG which would have significantly reduced time to PCI.
= = =
======================================
MY Comment, by KEN GRAUER, MD (10/23/2025):
As a primary care educator for the duration of my academic career — I find it difficult to review cases like the one presented today. This shouldn’t happen. As is our purpose in presenting cases on this ECG Blog — Lessons need to be learned. Hopefully the feedback from today’s case is passed on.
= = =
My Thoughts:
- As per Dr. Nossen — the clinical presentation of today’s case is “textbook” for ACS (Acute Coronary Syndrome) = a 69-year old longterm smoker who presents with sudden-onset severe CP (Chest Pain), associated with nausea, vomiting and diaphoresis. To quote Dr. Nossen, “If CP persists — this patient should go to the cath lab regardless of what her ECG shows.”
- The corollary to this, is that if for any reason the cath lab is not immediately activated — extremely close and ongoing follow-up is essential to ensure that this is not ACS (ie, Regardless of how the initial ECG is interpreted — the initial ECG should be repeated within 15-to-30 minutes). An actively evolving ACS in a patient with ongoing CP will often show “dynamic” ST-T wave abnormalities within this window of time.
- Instead — the ECG was not repeated until the initial Troponin came back significantly elevated. As we have often emphasized in Dr. Smith’s ECG Blog — Troponin provides a “rear-view mirror” indication of what has already happened — without telling you what is about to happen — which means that the first 1 or 2 Troponin values may be normal despite a developing acute event. As a result — it makes no sense to wait for Troponin results to tell you if (as well as when) the initial ECG should be repeated.
- Unfortunately — the initial ECG was not repeated for 84 minutes without indication as to whether this patient was still having CP (and if so, how severe) at the time ECG #2 was recorded. This clinical correlation between serial tracings and the patient’s symptoms is easy to document — and critical for understanding the clinical course of any patient who presents to the ED with CP.
= = =
We Must Do Better!
Today’s patient died. While there is no way to know if she could have been saved — the outcome may have been different IF the initial ECG would have been correctly interpreted and immediately acted on. The reality is that all-too-many emergency providers are not adequately trained in the basics of recognizing the ECG of ACS. In 2025 — this needs to change. Such change can be effected in a number of ways.
- EMS units have the capability of recording and transmitting on site ECGs. Receiving centers need to have an Attending physician on site who is skilled in ECG interpretion. And, if they don’t — it should take no more than 1-2 minutes to transmit an ECG to a remote expert. Everyone has a cell phone — and clinician experts in ECG interpretation should be readily reachable anywhere!
- As we routinely illustrate on Dr. Smith’s ECG Blog — the QOH (Queen-Of-Hearts) application instantly assesses ECGs with amazing accuracy as to whether or not acute OMI is likely. More widespread use of QOH could help both with acute decision-making, as well as with education for improving ECG provider competence.
- Simple steps can make a big difference. Many of the oversights that have been reviewed on this ECG Blog since Dr. Smith began posting cases in 2008 — could have been avoided by simple measures such as: i) Respecting the clinical history (ie, Appreciating that the history in today’s case immediately places this patient in a high risk category for having an acute event — such that even minimal ECG changes merit close attention); — ii) Being sure to obtain serial ECGs in timely fashion (ie, Not waiting hours to repeat the initial tracing); — iii) Routinely indicating whether CP is present (and if so — how severe?) at the time each serial ECG is recorded (as this is easy to do at that time — and when correlated to serial tracings, provides insight as to whether the “culprit” vessel is still occluded, or has spontaneously opened); — iv) Realizing that a single normal Troponin does not rule out an acute event; — and, v) Accepting that the STEMI paradigm is outdated, and misses ~30% of OMIs (not to mention the many cardiac caths that are delayed for hours until OMIs that were obvious on the initial ECG finally develop enough ST elevation to satisfy STEMI criteria).
= = =
Today’s Initial ECG should Not be Overlooked!
All 12 leads on today’s initial ECG are abnormal!
- In a patient with new-onset severe CP — my “eye” was immediately drawn to the ST segment straightening with 1.5 mm of J-point ST elevation in lead V2 (the RED arrow in lead V2 of Figure-1). In the context of this lead V2 finding — the more subtle ST segment straightening and elevation in lead V1 is also clearly abnormal (within the RED rectangle). Of note — QS complexes of uncertain duration (New or old?) are present in both V1,V2.
- In stark contrast to this ST elevation in leads V1,V2 — is the ST segment flattening and depression that is present in the remaining 4 chest leads (BLUE arrows in leads V3,V4,V5,V6).
- Similar ST segment flattening and depression is seen in leads II,III,aVF
- ST segment coving with slight ST elevation and terminal T wave inversion is seen in lead aVL — with ST flattening and slight terminal T wave inversion in lead I (YELLOW arrows highlighting terminal T wave inversion in leads I and aVL).
- The remaining lead = lead aVR — shows ST coving with slight elevation.
Impression: All 12 leads in this initial ECG show ST-T wave abnormalities. At the very least — the shelf-like ST depression present in 7 leads (BLUE arrows) — in association with the subtle ST elevation in lead aVR suggest DSI (Diffuse Subendocardial Ischemia), that in a patient with new CP — most probably indicates severe and/or multi-vessel coronary disease.
- Given that ECG #1 was recorded relatively early during the course of this patient’s acute event — ST elevation is modest in amount and limited to 3 leads in ECG #1 (leads aVL,V1,V2). That said — the contrast in morphology of between the leads with ST elevation that are right next to the 7 leads with shelf-like ST depression in this patient with new 8/10 CP makes for an “ECG picture” that needs to be recognized.
- Considering the dramatic evolution in ECG #2 — “dynamic” ST-T wave changes would almost certainly have been seen had the repeat ECG been recorded within 15-to-20 minutes after ECG #1.
= = =
Figure-1: I’ve reproduced the first 2 tracings in today’s case.