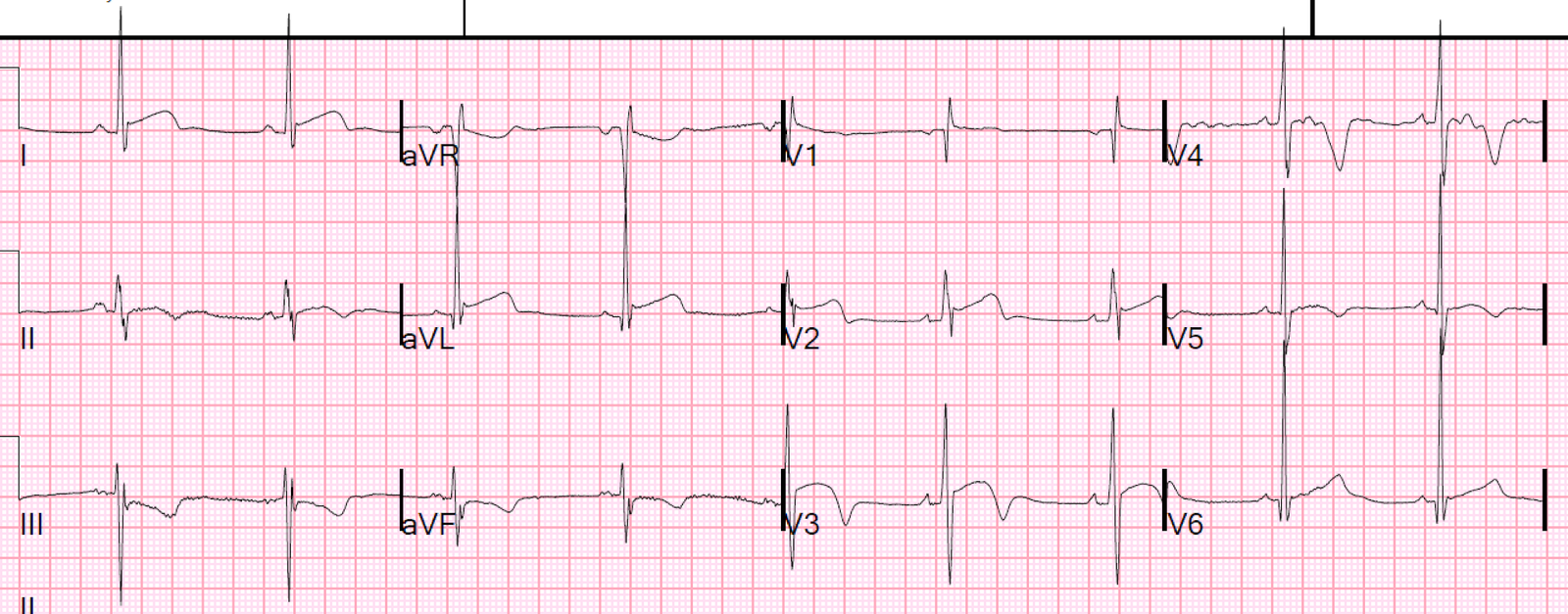
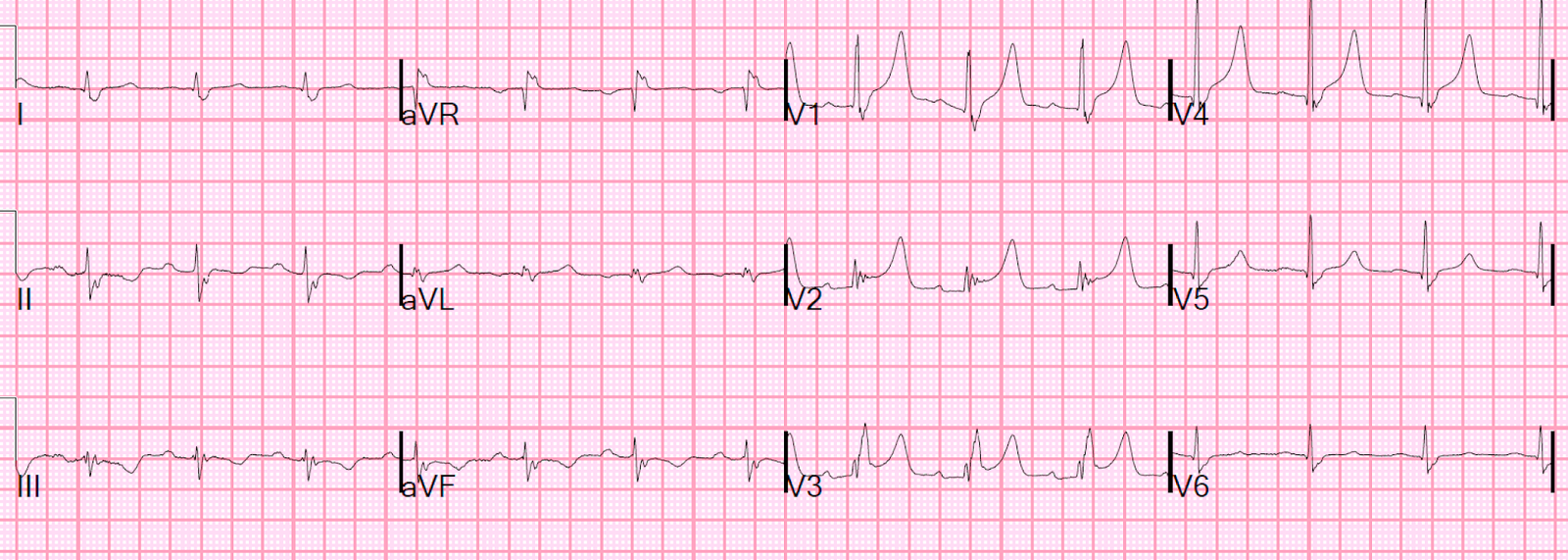
I was shown this ECG, without any clinical data:
What do you think?
My answer: “I think it is a baseline ECG, not ischemic.”
Why did I say that? Because of the very high voltage. Whenever you see voltage like that, ST-T abnormalities which at first appear to be ischemic are probably simply secondary to the abnormal depolarization and due to LVH or some other baseline disease.
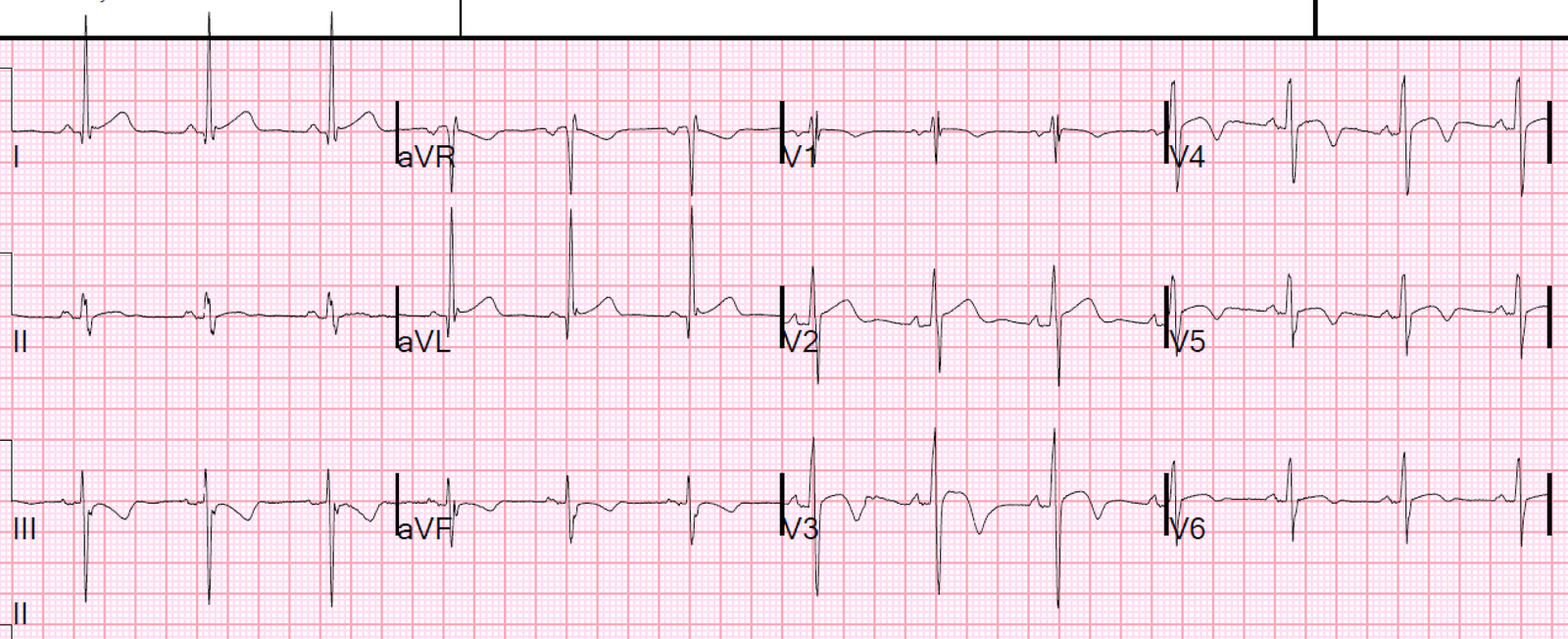
And so it was indeed the patient’s baseline ECG: The patient had presented for nonspecific symptoms and had the ECG recorded. So they searched for a previous ECG.
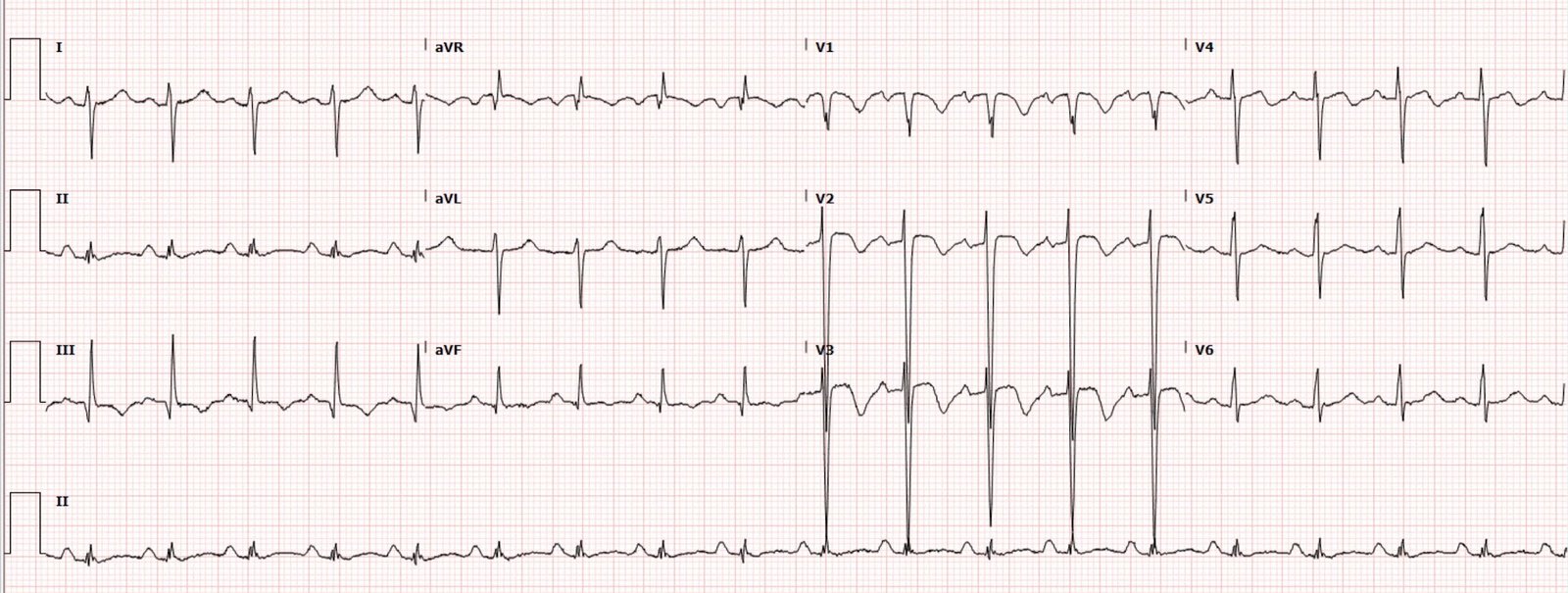
Here it is from 20 months prior.
Quite similar
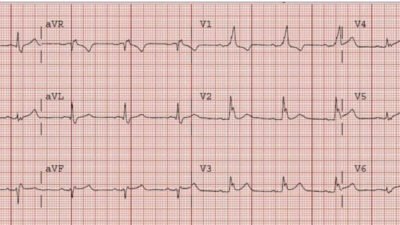
It turns out the patient had had an echocardiogram 22 months prior:
Prominent trabeculation is noted in the distal LV segments but not definitive for Left Ventricular Noncompaction Cardiomyopathy (LVNC).
Serial troponins and Serial ECGs were negative.
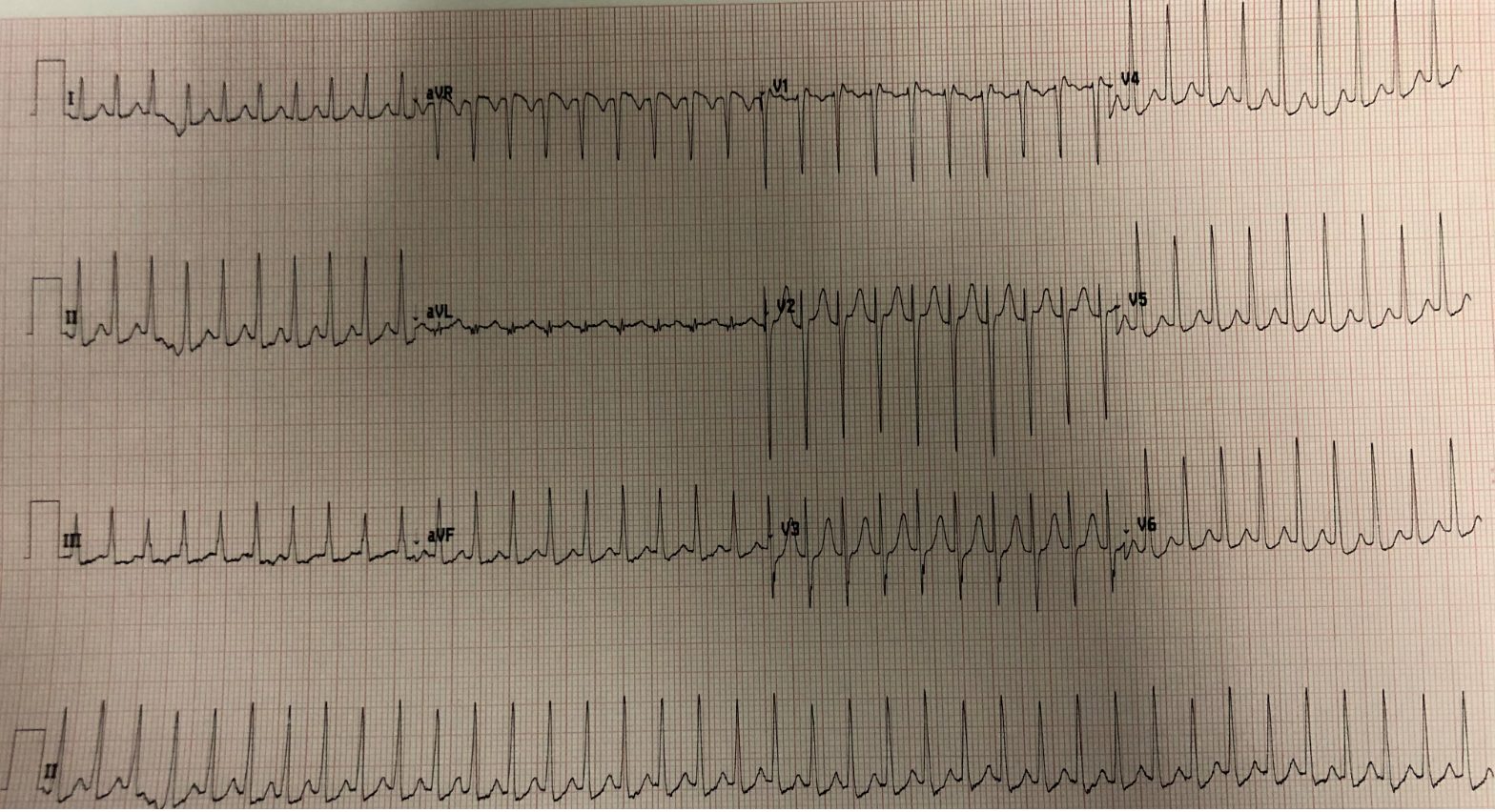
Another ECG was recorded that day:
Slightly different, but not significantly so. No evidence of developing ischemia.
The patient was discharged with followup.
Noncompaction Cardiomyopathy
A few pearls on LVNC copied from UpToDate (quotes):
Left ventricular noncompaction (LVNC) is a distinct phenotype characterized by prominent LV trabeculae and deep intertrabecular recesses. LVNC was previously also called spongy myocardium or hypertrabeculation syndrome but these terms should not be used interchangeably with LVNC.
LVNC is characterized by the following features:
●An altered myocardial wall with prominent trabeculae and deep intertrabecular recesses, resulting in thickened myocardium with two layers consisting of noncompacted myocardium and a thin compacted layer of myocardium (picture 1) [5-7].
●Continuity between the LV cavity and the deep intertrabecular recesses, which are filled with blood from the ventricular cavity without evidence of communication to the epicardial coronary artery system.
As discussed below, criteria for the extent of noncompaction have been developed to help distinguish the trabeculation seen in LVNC from that seen in other forms of heart disease and in healthy individuals. However, criteria are evolving and there may be morphologic overlap between LVNC and other types of cardiomyopathy and other pathologic and nonpathologic phenotypes. (See ‘Diagnosis’ below and ‘Differential diagnosis’ below.)
CLINICAL MANIFESTATIONS
Clinical manifestations of LVNC are variable and may include dyspnea, chest pain, palpitations, syncope, or an abnormal electrocardiogram (ECG) or echocardiogram [8,11,43]. Cardiac symptoms and signs may not be present. The major complications of LVNC are HF, atrial and ventricular arrhythmias, sudden cardiac arrest, and thromboembolic events, including stroke [5,11,18,44].
Echocardiography criteria
The presence of all four of the following echocardiographic criteria are required for diagnosis:
•A thickened LV wall consisting of two layers: a thin compacted epicardial layer and a markedly thickened endocardial layer with numerous prominent trabeculations and deep recesses with a maximum ratio of noncompacted to compacted myocardium >2:1 at end-systole in the parasternal short-axis view (image 2).
•Color Doppler evidence of flow within the deep intertrabecular recesses.
•Prominent trabecular meshwork in the LV apex or midventricular segments of the inferior and lateral wall.
•Compacted wall thickness ≤8.1 mm. The criterion of maximal systolic compacta thickness of ≤8.1 mm was found to be very specific for myocardial thickening in LVNC compared to normal controls or patients with aortic stenosis [54].
Great Full Text Review Article on Noncompaction Cardiomyopathy from the Journal of the American College of Cardiology. Hussein A et al. JACC 2015;66(5):578-586.
Some Pearls on the ECG from this article:
“94% of patients had an abnormal electrocardiogram (the most common abnormality was left bundle
branch block, observed in 44%).”
“Resting
electrocardiogram abnormalities are found in most
patients, but findings are nonspecific and include
left ventricular hypertrophy, repolarization changes,
inverted T waves, ST-segment changes, axis shifts,
intraventricular conduction abnormalities, and
atrioventricular blocks. Arrhythmias are
common, including ventricular tachyarrhythmias,
atrial fibrillation, and paroxysmal supraventricular
tachycardia, all of which can precipitate sudden death.”